Introduction
Our objectives were to compare the skeletal, dentoalveolar, and soft tissue effects of the AdvanSync appliance (Ormco, Glendora, Calif) with intermaxillary elastics in the correction of Class II malocclusions in growing patients.
Methods
A retrospective study was conducted using lateral cephalograms of patients taken before and after comprehensive orthodontic treatment; 41 patients consecutively treated with the AdvanSync were compared with 41 similar patients treated with intermaxillary Class II elastics. All patients had significant growth potential during treatment, as assessed by cervical vertebral maturation. A comparison group was generated from historical data bases and matched to the experimental groups for skeletal age, sex, and craniofacial morphology. Treatment changes were evaluated between the time points using a custom cephalometric analysis generating 31 variables as well as regional superimpositions. Data were analyzed using 1-way analysis of variance and Tukey-Kramer tests.
Results
The effects of the AdvanSync and fixed orthodontics included maxillary growth restriction, protrusion, proclination, and intrusion of the mandibular incisors as well as mesialization of the mandibular molars ( P <0.01). The effects of Class II elastics and fixed orthodontics were similar to AdvanSync, with the exceptions of less maxillary growth restriction and greater retrusion and retroclination of the maxillary incisors ( P <0.01). Significant mandibular growth stimulation, relative to the untreated controls, did not occur with either modality.
Conclusion
AdvanSync and intermaxillary elastics were effective in normalizing Class II malocclusions during comprehensive fixed orthodontics. AdvanSync produced its effects through maxillary skeletal growth restriction and mandibular dentoalveolar changes. Class II elastics worked primarily through dentoalveolar changes in both the maxilla and the mandible.
Highlights
- •
Class II correction with AdvanSync was compared with intermaxillary elastics.
- •
Both modalities were effective in normalizing Class II malocclusions.
- •
AdvanSync worked through maxillary restriction and mandibular dentoalveolar changes.
- •
Intermaxillary elastics worked through dentoalveolar changes in both jaws.
Treatment of Class II malocclusions has been a prime focus of orthodontic investigators for decades. Class II malocclusions occur in 23% of children aged 8 to 11 years, 15% of youths aged 12 to 17 years, and 13% of adults aged 18 to 50 years, thereby making it the most prevalent skeletal disharmony encountered in all age groups.
Numerous treatment modalities have been developed to correct Class II malocclusions. These include selective extraction patterns, orthopedic forces delivered with headgear, jaw orthopedics using functional appliances, removable and fixed intra-arch and interarch appliances, as well as orthognathic surgery to reposition 1 jaw or both jaws. Intermaxillary Class II elastics, a typical interarch modality, is perhaps the most common method used to correct Class II malocclusions. Numerous authors have investigated the effects of Class II elastics, including a systematic review, which have consistently shown that Class II elastics produce their effects primarily at the dentoalveolar level: mesial movement and extrusion of the mandibular molars, mesial movement and proclination of the mandibular incisors, and distal movements, retroclination, and extrusion of the maxillary incisors.
Fixed or removable functional appliances are designed to alter the position of the jaws both sagittally and vertically, resulting in orthopedic and orthodontic changes. Although the effects of some fixed functional appliances such as the Herbst and the mandibular anterior repositioning appliance (MARA) have been well documented in the literature, the effects of the AdvanSync appliance (Ormco, Glendora, Calif) are not well understood. This fixed functional appliance consists of crowns cemented to the maxillary and mandibular permanent first molars, which are connected by telescoping rods. The AdvanSync was designed to allow for simultaneous use of conventional edgewise appliances since the crowns have 0.022 × 0.028-in slots. The telescoping mechanism acts to constantly posture the mandible forward upon closure, with the goal of enhancing mandibular growth to correct the Class II malocclusion.
To date, there has only been 1 study published in the literature that has evaluated the effects of AdvanSync. Al-Jewair et al compared the effects of the AdvanSync with MARA and found that both were effective in normalizing Class II malocclusions; the AdvanSync appeared to show more of a headgear effect (maxillary restriction), but less mandibular length enhancement compared with the MARA. The 2 appliances produced similar dentoalveolar changes (mesial movement of the mandibular molars and proclination and protrusion of the mandibular incisors). No known study has compared the effects of AdvanSync with Class II elastics.
The purpose of this study was to compare the cephalometric skeletal, dentoalveolar, and soft tissue effects of the AdvanSync appliance and intermaxillary elastics in the correction of Class II malocclusions in growing patients when used with preadjusted edgewise appliances. Both treatment groups were also compared with an untreated control group.
Materials and methods
Ethics approval was obtained from the Health Research Ethics Board of the University of Manitoba in Winnipeg, Manitoba, Canada. Treatment records were all obtained from 1 private orthodontic practice. Records included dated pretreatment (T1) and postcomprehensive treatment (T2) cephalometric radiographs, sex, date of birth, and dates of AdvanSync insertion and removal. All patients had signed consent forms permitting the use of their records for research purposes. Pretreatment overjet and severity of Class II malocclusion (molar relationship) were also obtained from the clinical examination notes. All digital radiographs were taken with a Kodak 8000C digital imaging system (Carestream Health, Rochester, NY).
Inclusion criteria were pretreatment Class II malocclusion of a half cusp (end-to-end) at the molars or greater, skeletal Class II malocclusion indicated by an ANB angle greater than 4°, Class I posttreatment molar relationship, prepubertal stage of development at T1, and postpubertal stage at T2 according to the cervical vertebral maturation (CVM) method, no missing teeth (excluding third molars), nonextraction treatment protocol (based on crowding, protrusion, soft tissue factors, and growth potential), and no syndromic or craniofacial anomaly.
The AdvanSync group included 41 consecutively treated Class II malocclusion patients (24 boys, 17 girls). The Class II elastics group included 41 randomly selected patients (with the exception of sex matching subjects in the AdvanSync group) from the data base of treated patients between 2009 and 2013. An untreated Class II control sample of 37 subjects was generated from the University of Michigan and the Bolton-Brush growth studies and matched with the treated groups for skeletal age, sex, and observation period. Mean ages, observation periods, and sex distribution for each group are listed in Table I .
| Group | Mean (±SD) age at T1 (y) | Mean (±SD) age at T2 (y) | Observation period (±SD) (y) | Boys/girls |
|---|---|---|---|---|
| AdvanSync | 11.55 ± 1.58 | 14.30 ± 1.33 | 2.74 ± 0.88 | 24/17 |
| Class II elastics | 11.54 ± 1.45 | 14.40 ± 1.38 | 2.85 ± 0.43 | 24/17 |
| Control | 11.55 ± 0.58 | 14.34 ± 0.66 | 2.79 ± 0.61 | 22/15 |
| ANOVA P value |
0.99 | 0.93 | 0.76 |
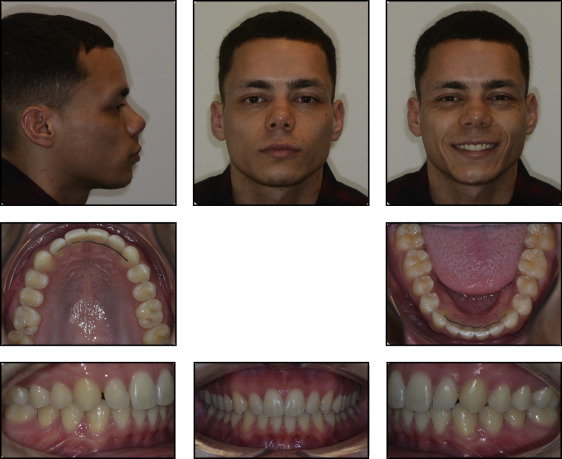
Patients in the AdvanSync and Class II elastics groups were treated in a similar fashion by 1 practitioner (S.M.H.). All patients were treated with the same prescription of Damon Q brackets (Ormco) and consistent archwire sequencing. All patients were initially prescribed elastics to correct the Class II malocclusion. In compliant patients, elastics were used until the sagittal discrepancy was corrected (approximately 22-24 months). Elastics were typically quarter inch, 3.5 oz, and worn from the maxillary canines to the mandibular first molars. In patients who were not compliant with the elastics, the AdvanSync appliance was installed and used to correct the malocclusion. In these patients, the molar relationship had not improved since the start of treatment and before delivery of the appliance. The AdvanSync was used following a similar protocol to that suggested by Dischinger, who helped to develop the appliance. The appliance was activated in increments until an edge-to-edge incisor relationship was achieved. After overcorrection of the sagittal discrepancy, the appliance was removed, and treatment was completed with conventional appliances. The average length of the AdvanSync treatment was 12.5 months (±1.5 months). Interproximal reduction was not used in any AdvanSync or Class II elastics patient. Figure 1 (T1), Figure 2 (progress with appliance in place), and Figure 3 (T2) provide a clinical example of treatment progression with the AdvanSync.


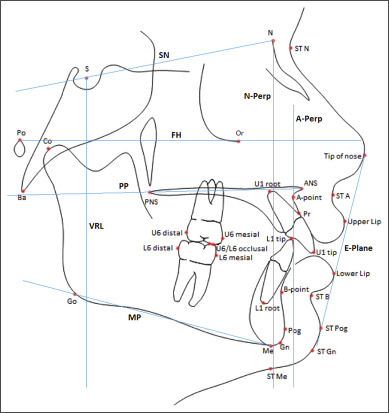
For the cephalometric analysis, the cephalometric radiographs taken at T1 and T2 were imported into a commercial software (version 11.7; Dolphin Digital Imaging and Management Solutions, Chatsworth, Calif). For the AdvanSync and Class II elastics patients, the magnification of the radiographs was accounted for using known ruler measurements that were captured on the cephalograms. The radiographs from the Michigan growth study and the Bolton-Brush study had magnifications of 12.9% and 6%, respectively. To standardize the radiographs, all magnifications were corrected to 0%. Radiographs were digitally traced using a custom digitized analysis adapted and modified from that of Al-Jewair et al, which included 35 landmarks and produced 31 measurements. The analysis included a combination of the variables described by Jacobson, McNamara, Ricketts, and Steiner. Cephalometric landmarks and reference lines are illustrated in Figure 4 .
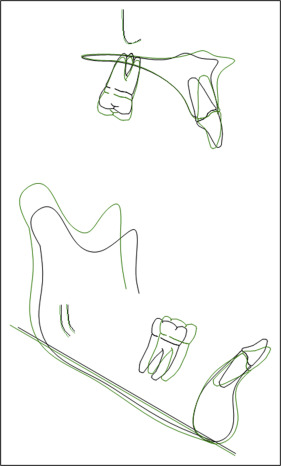
Regional superimpositions were conducted manually to evaluate sagittal and vertical dentoalveolar changes. Maxillary superimpositions were made along the palatal plane, registering on the internal structures of the maxilla and the surfaces of the hard palate. Mandibular superimpositions were made on the inner contour of the posterior symphysis, the outline of the inferior mandibular canal, and the germ of the third molar, if present. The superimpositions used in this study are illustrated in Figure 5 . Once superimposed, the vertical and sagittal dentoalveolar changes were measured using the methods described by McNamara. Skeletal maturity was also assessed on each radiograph, using the CVM method.
One investigator (S.J.) made all tracings and measurements. This investigator retraced the records of 10 subjects in each group (randomly selected), including CVM assessments, 2 weeks after the initial data collection to test for intrarater reliability. A second investigator (L.O.D.) traced the same randomly selected sample to test for interrater reliability.
Statistical analysis
Statistical software (version 9.2; SAS Institute, Cary, NC) was used to analyze the data. Normal distribution of the study variables was confirmed. Descriptive statistics were performed and reported as means, standard deviations, and 95% confidence intervals for all variables in each group. Comparisons of the T1 and T2 measurements of the treatment groups and the control group were carried out by 1-way analysis of variance (ANOVA). Ages at T1 and T2 as well as observation periods were also compared using ANOVA. If these results were significant, the Tukey-Kramer test was used to determine where the significant differences occurred and to adjust for multiple comparisons. CVM values at T1 and T2 were compared among the 3 groups using the Fisher exact test. Interrater and intrarater reliabilities were examined using intraclass correlation tests. All statistical tests were interpreted at the 5% significance level.
Results
The comparisons of the parameters at T1 of the treatment and control groups are shown in Table II . Only 2 measurements were significantly different between the 2 treatment groups. The Class II elastics patients initially had a greater overjet ( P <0.01) and retruded soft tissue B point (B-VRL; P <0.05) relative to the AdvanSync group. Three measurements were significantly different between the AdvanSync and control groups (L1-APo, molar relationship, and L lip to E-plane; P <0.05), and 7 were significantly different between the Class II elastics and control groups (A-Na perp, Wits appraisal, PP, U1-A perp, IMPA, overjet, and B-VRL; P <0.05).
| Variables | AdvanSync (A), mean ± SD | Class II elastics (E), mean ± SD | Control (C), mean ± SD | ANOVA P value | Tukey-Kramer P value |
||
|---|---|---|---|---|---|---|---|
| A-C | E-C | A-E | |||||
| Cranial base | |||||||
| Ba-S-N (°) | 131.97 ± 4.23 | 130.93 ± 4.12 | 131.17 ± 4.59 | 0.53 | 0.70 | 0.97 | 0.52 |
| Maxillary skeletal | |||||||
| SNA (°) | 81.25 ± 3.96 | 81.28 ± 3.35 | 80.19 ± 3.46 | 0.33 | 0.40 | 0.38 | 0.99 |
| A-Na perp (mm) | −1.07 ± 3.38 | −0.01 ± 2.87 | −1.97 ± 2.98 | 0.02 ∗ | 0.40 | <0.01 ∗ | 0.27 |
| Co-A (mm) | 81.75 ± 4.39 | 80.94 ± 3.36 | 80.73 ± 3.89 | 0.47 | 0.48 | 0.97 | 0.61 |
| Mandibular skeletal | |||||||
| SNB (°) | 76.10 ± 3.47 | 75.44 ± 3.33 | 75.24 ± 2.81 | 0.47 | 0.47 | 0.96 | 0.63 |
| Pg-Na perp (mm) | −8.33 ± 6.27 | −8.13 ± 5.73 | −10.28 ± 4.46 | 0.18 | 0.27 | 0.20 | 0.99 |
| Co-Gn (mm) | 106.11 ± 5.43 | 104.86 ± 5.14 | 105.36 ± 5.39 | 0.56 | 0.81 | 0.91 | 0.54 |
| Co-Go (mm) | 52.56 ± 4.20 | 50.76 ± 4.09 | 50.45 ± 4.37 | 0.06 | 0.07 | 0.94 | 0.14 |
| Intermaxillary | |||||||
| ANB (°) | 5.14 ± 0.75 | 5.49 ± 0.83 | 5.17 ± 0.97 | 0.62 | 0.99 | 0.71 | 0.65 |
| Wits (mm) | 4.16 ± 2.22 | 4.31 ± 2.18 | 3.05 ± 1.90 | 0.02 ∗ | 0.06 | 0.02 ∗ | 0.94 |
| Mx/md difference (mm) | 21.50 ± 3.56 | 20.95 ± 3.91 | 21.86 ± 4.04 | 0.58 | 0.91 | 0.55 | 0.80 |
| Convexity (mm) | 3.26 ± 2.13 | 3.80 ± 1.74 | 3.45 ± 2.21 | 0.47 | 0.91 | 0.72 | 0.45 |
| Vertical skeletal | |||||||
| PP (°) | 1.78 ± 3.09 | 2.55 ± 2.67 | 0.01 ± 3.91 | <0.01 ∗ | 0.06 | <0.01 ∗ | 0.53 |
| FMA (°) | 24.67 ± 4.66 | 25.22 ± 5.14 | 26.54 ± 3.35 | 0.17 | 0.16 | 0.40 | 0.84 |
| MPA (°) | 32.83 ± 5.22 | 33.97 ± 5.29 | 34.23 ± 4.03 | 0.40 | 0.42 | 0.97 | 0.55 |
| Y-axis (°) | 67.94 ± 3.51 | 68.97 ± 3.63 | 68.04 ± 3.50 | 0.36 | 0.99 | 0.48 | 0.39 |
| LFH (mm) | 60.86 ± 4.81 | 61.22 ± 5.05 | 60.40 ± 4.78 | 0.76 | 0.91 | 0.74 | 0.94 |
| Maxillary dentoalveolar | |||||||
| U1-A perp (mm) | 3.35 ± 3.00 | 4.65 ± 2.23 | 3.05 ± 2.27 | 0.01 ∗ | 0.86 | 0.02 ∗ | 0.06 |
| U1-FH (°) | 110.34 ± 8.94 | 113.80 ± 6.97 | 109.88 ± 6.10 | 0.04 ∗ | 0.96 | 0.06 | 0.09 |
| U1-SN(°) | 102.69 ± 9.07 | 105.05 ± 7.26 | 102.19 ± 6.02 | 0.20 | 0.96 | 0.22 | 0.34 |
| Mandibular dentoalveolar | |||||||
| L1-APo (mm) | −0.23 ± 2.57 | −0.05 ± 2.34 | 1.24 ± 2.37 | 0.02 ∗ | 0.02 ∗ | 0.06 | 0.94 |
| IMPA (°) | 97.29 ± 5.72 | 94.26 ± 6.21 | 98.13 ± 5.98 | 0.01 ∗ | 0.81 | <0.01 ∗ | 0.06 |
| Interdental | |||||||
| Overjet (mm) | 6.80 ± 2.40 | 8.21 ± 2.22 | 5.83 ± 1.77 | <0.01 ∗ | 0.12 | <0.01 ∗ | <0.01 ∗ |
| Overbite (mm) | 4.68 ± 2.56 | 4.65 ± 2.21 | 5.01 ± 2.15 | 0.76 | 0.81 | 0.78 | 0.99 |
| U1/L1 (°) | 128.67 ± 13.35 | 126.72 ± 8.46 | 125.46 ± 8.93 | 0.40 | 0.37 | 0.86 | 0.68 |
| Molar relationship (mm) | 2.16 ± 1.15 | 1.94 ± 1.37 | 1.50 ± 1.00 | 0.05 ∗ | 0.04 ∗ | 0.24 | 0.67 |
| Soft tissue | |||||||
| A-VRL (mm) | 77.80 ± 4.78 | 76.51 ± 4.46 | 78.54 ± 4.60 | 0.17 | 0.78 | 0.16 | 0.41 |
| B-VRL (mm) | 67.03 ± 5.41 | 63.61 ± 6.12 | 67.04 ± 4.95 | 0.01 ∗ | 1.00 | 0.03 ∗ | 0.02 ∗ |
| Pg-VRL (mm) | 68.42 ± 6.95 | 65.26 ± 7.11 | 68.17 ± 5.76 | 0.07 | 0.99 | 0.17 | 0.09 |
| U lip to E-plane (mm) | −1.43 ± 2.81 | −0.45 ± 2.01 | −0.11 ± 2.39 | 0.05 ∗ | 0.06 | 0.83 | 0.16 |
| L lip to E-plane (mm) | −1.02 ± 3.18 | −0.51 ± 2.75 | 0.73 ± 2.78 | 0.04 ∗ | 0.04 ∗ | 0.18 | 0.71 |
The treatment effects (T2-T1) are presented in Table III . The AdvanSync in combination with preadjusted edgewise appliances, compared with the untreated controls, produced maxillary skeletal growth restriction (SNA, A-Na perp, and Co-A; P <0.01), improvement in the intermaxillary skeletal relationship (ANB, Wits appraisal, Mx/mn difference, and convexity; P <0.01), maxillary incisor extrusion (U1-vertical; P <0.05), mandibular incisor protrusion, proclination, and intrusion (L1-APo, L1-horizontal, IMPA, and L1-vertical; P <0.01), as well as mandibular molar mesialization (L6-horizontal; P <0.01). The magnitude of the maxillary skeletal restriction relative to the controls was 2.57° according to SNA, 2.00 mm according to A-Na perp, and 2.53 mm according to Co-A. Figure 6 illustrates a typical overall superimposition of a patient treated with the AdvanSync.
| Variable | AdvanSync (A), mean ± SD | Class II elastics (E), mean ± SD | Control (C), mean ± SD | ANOVA P value | Tukey-Kramer P value |
||
|---|---|---|---|---|---|---|---|
| A-C | E-C | A-E | |||||
| Cranial base | |||||||
| Ba-S-N (°) | 0.19 ± 1.75 | −0.51 ± 1.42 | 1.04 ± 2.30 | <0.01 ∗ | 0.11 | <0.01 ∗ | 0.20 |
| Maxillary skeletal | |||||||
| SNA (°) | −2.05 ± 1.39 | −0.17 ± 1.26 | 0.52 ± 1.71 | <0.01 ∗ | <0.01 ∗ | 0.10 | <0.01 ∗ |
| A-Na perp (mm) | −1.99 ± 1.34 | −0.23 ± 1.32 | 0.01 ± 1.88 | <0.01 ∗ | <0.01 ∗ | 0.78 | <0.01 ∗ |
| Co-A (mm) | 1.66 ± 2.84 | 2.63 ± 2.09 | 4.19 ± 3.00 | <0.01 ∗ | <0.01 ∗ | 0.03 ∗ | 0.23 |
| Mandibular skeletal | |||||||
| SNB (°) | 0.41 ± 1.24 | 0.80 ± 1.37 | 0.74 ± 1.44 | 0.38 | 0.54 | 0.97 | 0.39 |
| Pg-Na perp (mm) | 0.79 ± 1.97 | 1.07 ± 2.70 | 0.38 ± 2.94 | 0.49 | 0.76 | 0.46 | 0.87 |
| Co-Gn (mm) | 7.53 ± 4.09 | 7.11 ± 3.30 | 7.01 ± 2.57 | 0.77 | 0.78 | 0.99 | 0.84 |
| Co-Go (mm) | 5.03 ± 3.65 | 4.69 ± 2.40 | 4.49 ± 2.83 | 0.72 | 0.71 | 0.95 | 0.87 |
| Intermaxillary | |||||||
| ANB (°) | −2.46 ± 1.18 | −0.97 ± 1.32 | −0.20 ± 1.20 | <0.01 ∗ | <0.01 ∗ | 0.02 ∗ | <0.01 ∗ |
| Wits (mm) | −3.80 ± 1.73 | −2.70 ± 1.86 | 0.54 ± 1.89 | <0.01 ∗ | <0.01 ∗ | <0.01 ∗ | 0.02 ∗ |
| Mx/md difference (mm) | 5.58 ± 2.67 | 4.44 ± 2.76 | 3.21 ± 2.76 | <0.01 ∗ | <0.01 ∗ | 0.12 | 0.15 |
| Convexity (mm) | −2.47 ± 1.24 | −0.79 ± 1.26 | −0.24 ± 1.23 | <0.01 ∗ | <0.01 ∗ | 0.13 | <0.01 ∗ |
| Vertical skeletal | |||||||
| PP (°) | −0.13 ± 1.92 | −0.58 ± 2.08 | −0.80 ± 2.08 | 0.33 | 0.31 | 0.88 | 0.57 |
| FMA (°) | −0.32 ± 2.23 | 0.11 ± 1.58 | −0.46 ± 1.59 | 0.35 | 0.93 | 0.35 | 0.54 |
| MPA (°) | −0.39 ± 2.56 | 0.07 ± 1.59 | −0.84 ± 1.55 | 0.13 | 0.57 | 0.11 | 0.55 |
| Y-axis (°) | 0.37 ± 1.30 | 0.33 ± 1.46 | 0.11 ± 1.15 | 0.66 | 0.66 | 0.75 | 0.99 |
| LFH (mm) | 3.70 ± 2.42 | 4.61 ± 2.34 | 3.41 ± 2.07 | 0.06 | 0.84 | 0.06 | 0.17 |
| Maxillary dentoalveolar | |||||||
| U1-A perp (mm) | 0.20 ± 2.74 | −2.80 ± 2.68 | −0.32 ± 1.44 | <0.01 ∗ | 0.60 | <0.01 ∗ | <0.01 ∗ |
| U1-FH (°) | −1.23 ± 8.54 | −6.47 ± 9.22 | −1.55 ± 3.64 | <0.01 ∗ | 0.98 | 0.01 ∗ | 0.01 ∗ |
| U1-SN (°) | −1.17 ± 8.57 | −6.41 ± 9.17 | −1.16 ± 3.28 | <0.01 ∗ | 1.00 | 0.01 ∗ | 0.01 ∗ |
| U1-vertical (mm) | 1.7 ± 1.7 | 1.5 ± 1.4 | 0.9 ± 1.1 | 0.03 ∗ | 0.03 ∗ | 0.11 | 0.84 |
| U1-horizontal (mm) | 0.3 ± 2.7 | −2.9 ± 2.7 | 0.2 ± 1.6 | <0.01 ∗ | 0.99 | <0.01 ∗ | <0.01 ∗ |
| U6-vertical (mm) | 1.7 ± 1.4 | 2.7 ± 1.6 | 2.4 ± 1.3 | 0.01 ∗ | 0.09 | 0.66 | 0.01 ∗ |
| U6-horizontal (mm) | 1.8 ± 2.3 | 1.2 ± 1.9 | 1.3 ± 1.6 | 0.40 | 0.53 | 0.99 | 0.43 |
| Mandibular dentoalveolar | |||||||
| L1-APo (mm) | 3.39 ± 2.00 | 2.66 ± 1.58 | −0.08 ± 1.35 | <0.01 ∗ | <0.01 ∗ | <0.01 ∗ | 0.13 |
| IMPA (°) | 8.98 ± 6.83 | 9.33 ± 5.49 | 0.36 ± 3.70 | <0.01 ∗ | <0.01 ∗ | <0.01 ∗ | 0.96 |
| L1-vertical (mm) | −0.6 ± 2.2 | −0.3 ± 2.0 | 2.4 ± 1.3 | <0.01 ∗ | <0.01 ∗ | <0.01 ∗ | 0.75 |
| L1-horizontal (mm) | 1.9 ± 2.5 | 1.6 ± 1.9 | 0.1 ± 1.4 | <0.01 ∗ | <0.01 ∗ | <0.01 ∗ | 0.85 |
| L6-vertical (mm) | 2.4 ± 1.7 | 2.2 ± 1.6 | 1.7 ± 1.4 | 0.09 | 0.09 | 0.25 | 0.84 |
| L6-horizontal (mm) | 2.6 ± 1.5 | 2.9 ± 1.9 | 1.3 ± 1.3 | <0.01 ∗ | <0.01 ∗ | <0.01 ∗ | 0.76 |
| Interdental | |||||||
| Overjet (mm) | −4.21 ± 2.25 | −5.84 ± 2.43 | −0.57 ± 1.40 | <0.01 ∗ | <0.01 ∗ | <0.01 ∗ | <0.01 ∗ |
| Overbite (mm) | −2.92 ± 2.51 | −3.01 ± 2.32 | 0.09 ± 1.29 | <0.01 ∗ | <0.01 ∗ | <0.01 ∗ | 0.98 |
| U1/L1 (°) | −7.44 ± 12.02 | −2.98 ± 10.48 | 1.63 ± 5.03 | <0.01 ∗ | <0.01 ∗ | 0.10 | 0.10 |
| Molar relationship (mm) | −4.90 ± 1.50 | −4.39 ± 1.38 | −0.19 ± 0.88 | <0.01 ∗ | <0.01 ∗ | <0.01 ∗ | 0.14 |
| Soft tissue | |||||||
| A-VRL (mm) | 2.10 ± 2.78 | 2.27 ± 2.35 | 3.51 ± 3.22 | 0.08 | 0.08 | 0.15 | 0.96 |
| B-VRL (mm) | 3.17 ± 3.48 | 4.48 ± 2.96 | 3.19 ± 3.21 | 0.13 | 1.00 | 0.22 | 0.16 |
| Pg-VRL (mm) | 3.55 ± 3.75 | 3.52 ± 3.56 | 4.34 ± 3.55 | 0.57 | 0.63 | 0.61 | 1.00 |
| U lip to E-plane (mm) | −2.54 ± 1.90 | −2.51 ± 1.43 | −1.84 ± 2.34 | 0.23 | 0.27 | 0.30 | 0.99 |
| L lip to E-plane (mm) | −1.00 ± 2.13 | −0.41 ± 2.09 | −1.80 ± 2.41 | 0.03 ∗ | 0.28 | 0.03 ∗ | 0.45 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


