Introduction
The aim of this study was to evaluate and compare the effects of 2 protocols of bone-anchored maxillary protraction with an untreated control group.
Methods
Thirty growing Class III subjects with maxillary deficiency in the late mixed or early permanent dentition were included in the study. In group 1 (n = 10), skeletally anchored facemasks were used with miniplates placed at the zygomatic buttress. In group 2 (n = 10), the patients were treated with Class III elastics extending from infrazygomatic miniplates in the maxilla to symphyseal miniplates in the mandible. Group 3 (n = 10) was an untreated control group. Pretreatment and posttreatment cephalometric radiographs were analyzed.
Results
The treatment periods were 8 and 8.9 months in groups 1 and 2, respectively, and the untreated control group was observed for 9.4 months. The maxilla moved forward significantly in groups 1 and 2 compared with the untreated control group (4.87 mm in group 1, 5.81 mm in group 2); overjet and maxillary incisor display were improved without proclination or mesialization of the maxillary teeth relative to the maxillary base. Soft tissue harmony demonstrated the great improvement. However, group 1 showed more opening rotation of the mandible and lingual inclination of the mandibular incisors than did group 2.
Conclusions
The 2 skeletal anchorage protocols for maxillary protraction effectively resolved the severe maxillary deficiently in growing Class III patients. However, vertical changes and retroclination of the mandibular incisors were better controlled by Class III elastics extending from the infrazygomatic miniplates in the maxilla to the symphyseal miniplates in the mandible (group 2).
Highlights
- •
Skeletal anchorage methods for maxillary protraction were compared in growing Class III patients.
- •
In group 1, facemasks were anchored to miniplates in the zygomatic buttress.
- •
In group 2, elastics connected infrazygomatic miniplates to symphyseal miniplates.
- •
Vertical changes and mandibular incisor retroclination were better controlled by elastics.
Class III malocclusions are considered to be among the most challenging orthodontic problems and include different combinations of abnormal dental and skeletal patterns. The Class III skeletal pattern can be due to maxillary retrognathism, mandibular prognathism, or a combination of both; maxillary retrognathism is present in 67% of Class III patients.
Facemask therapy is most commonly used for treatment of growing Class III patients with a maxillary deficiency. Almost always, an intraoral appliance is placed on the maxillary teeth with elastics stretched between the intraoral and extraoral parts. Indirect application of force limits orthopedic effects and causes undesirable changes such as extrusion and mesial movement of the maxillary molars, proclination of the maxillary incisors, and retroclination of the mandibular incisors. In addition to the closing rotation of the maxilla, an opening rotation of the mandible occurs, causing the chin to move downward and backward. Lower anterior facial height increases, whereas overbite decreases.
Trials have been made to transfer orthopedic forces directly to the circummaxillary sutures using ankylosed deciduous canines, osseointegrated implants in the zygomatic buttress, titanium lag screws, and onplants on the palatal bone as anchorage for facemask treatment. Titanium miniplates have been used successfully as temporary anchorage devices to provide absolute skeletal anchorage in many orthodontic applications. Facemasks have been used with surgical miniplates to apply orthopedic forces directly to the maxillofacial skeletal complex and to reduce the undesired effects of conventional facemask therapy.
De Clerck et al suggested an innovative intraoral treatment protocol for correcting Class III malocclusions consisting of Class III elastics applied 24 hours a day from infrazygomatic miniplates in the maxilla to symphyseal miniplates in the mandible. Investigators concluded that bone-anchored maxillary protraction is more effective than tooth-anchored maxillary protraction.
This is the first study to evaluate and compare the effects of skeletally anchored facemasks using miniplates and the effects of Class III elastics from infrazygomatic miniplates in the maxilla to symphyseal miniplates in the mandible with an untreated control group.
Material and methods
This study was conducted in the orthodontic departments of 2 universities (Tanta University, Tanta, Egypt, and the University of Illinois at Chicago). A total of 30 growing Class III patients were selected from patients seeking orthodontic treatment according to the following inclusion criteria: (1) growing Class III patients with a prepubertal stage of skeletal maturity according to the cervical vertebral maturation method ; (2) skeletal Class III malocclusion with maxillary deficiency (ANB, <0°; Nperp-A, <0°) with or without mandibular prognathism; (3) late mixed or early permanent dentition at the start of treatment characterized by a Wits appraisal of −1 mm or less and an Angle Class III molar relationship or anterior crossbite; (4) vertically normal growth pattern determined by cephalometric x-rays; (5) no cleft and other craniofacial anomaly; and (6) no previous orthodontic treatment.
The patients and their parents were informed about the study and the steps of treatment, and the parents signed consent forms. In addition, assent forms were required from the children who participated in the study. The study was approved by the research ethical committees of both universities. All patients were treated by the same operator (M.H.E.).
The patients were divided by random number tables into 3 groups.
- 1.
Group 1 (n = 10; 6 boys, 4 girls; mean age, 11.9 ± 1.3 years). They were treated with facemasks anchored with miniplates in the zygomatic buttress area of the maxilla (skeletally anchored facemask).
- 2.
Group 2 (n = 10; 7 boys, 3 girls; mean age, 12.24 ± 1 years), They were treated with Class III elastics extending from the infrazygomatic miniplates in the maxilla to the symphyseal miniplates in the mandible.
- 3.
Group 3 (n = 10; 7 boys, 3 girls; mean age, 11.7 ± 1.6 years) was the control group; records were taken before and after the observation period to distinguish treatment changes from growth changes. Then these patients started treatment.
In Group 1, anchor surgical miniplates (55-0851; Stryker Leibinger, Freiburg, Germany) were placed at the zygomatic buttress area to prevent damage to the underlying developing tooth buds of the permanent teeth. The incision was made at the buccal vestibule below the zygomatic buttress area under local anesthesia. A mucoperiosteal flap was elevated, and the surface of the cortical bone was exposed. A surgical miniplate was bent freehandedly using a bird-beak orthodontic pliers according to the anatomy of the zygomatic buttress in a curvilinear pattern and fixed with 3 self-tapping bone screws per side (2-mm diameter, 6-mm length; 50-20706; Stryker Leibinger). At least 3 or 4 screws were used to resist a protraction force of approximately 400 to 500 g per side. The end of the miniplate was exposed over the keratinized attached gingiva near the canine to prevent gingival irritation and to control the vector of elastic traction. The end hole of the miniplate was cut to create a hook for the elastics ( Fig 1 ).

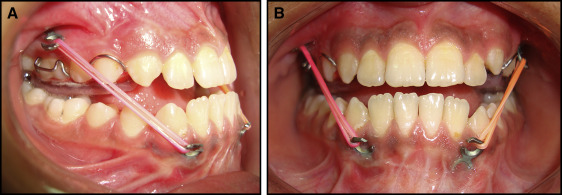
Three weeks after the miniplates were placed, their stability was assessed with a metal instrument. The facemask was inserted, and an orthopedic force of at least 400 to 500 g per side directed 30° downward and forward from the occlusal plane was applied by heavy extraoral elastics (Ormco, Orange, Calif). The force was measured by a force gauge (Correx Tension Gauge; Haag-Streit Diagnostics, Koeniz, Switzerland). Patients were instructed to wear the appliance for at least 14 to 16 hours a day and to change the elastics daily. A removable maxillary biteplate covering the posterior occlusal surfaces was placed to eliminate occlusal interference in the incisor region until correction of the anterior crossbite was obtained ( Fig 2 ).

In group 2, 4 straight miniplates (55-0851, Stryker Leibinger) were placed in each patient at the infrazygomatic crest of the maxillary buttress and in the mandible between, and inferior to, the left and right permanent lateral incisors and canines. In the maxilla, an L-shaped flap was made with a vertical incision mesial to the infrazygomatic crest, and a horizontal incision was extended distally 2 mm below and parallel to the mucogingival line; a mucoperiosteal flap was elevated for bone exposure. Straight surgical miniplates, 25 mm or 6 holes in length, were bent freehandedly using a bird-beak orthodontic pliers to adapt to the anatomy of the infrazygomatic buttress and fixed with 3 self-tapping bone screws per side (2-mm diameter, 6-mm length; 50-20706; Stryker Leibinger). An insert bayonet bend in the miniplates was made using 3-prong orthodontic pliers just below the inferior bone screw hole to make intimate contact with the cortical bone and minimize stresses on the bone screws ( Fig 3 ).
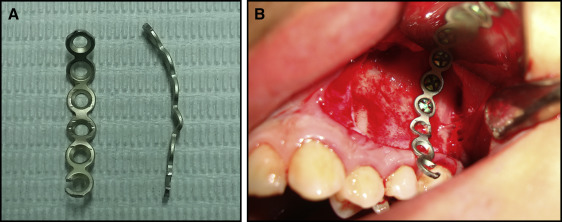
In the mandible, an inverted L-shaped flap was made with the horizontal part of the incision located 2 mm above the mucogingival line, and a mucoperiosteal flap was elevated for bone exposure. Straight miniplates of 21 mm or 5 holes in length were bent freehandedly to adapt to the bone anatomy inferiorly between the mandibular lateral incisors and the canines (after eruption of mandibular canines) and fixed with 2 or 3 self-tapping bone screws per side so that the upper screw was at the level of root apices. At all sites, the ends of the miniplates were exposed over the keratinized attached gingiva to prevent gingival irritation, and the distal end holes of the miniplates were cut to create a hook for the elastics. All mucoperiosteal flaps were secured and sutured. The surgical sites were allowed to heal for 2 to 3 weeks, and the stability of the miniplates was assessed before orthopedic loading ( Fig 4 ).

In the orthopedic protocol, the miniplates were loaded 2 to 3 weeks after surgery. Elastics were placed on each side to give vectors of force downward and forward for the maxilla, and backward and upward (closing rotation) for the mandible. The elastics were chosen to provide a force of approximately 250 g to each side. The forces was measured with the patient in maximum intercuspation using a force gauge (Correx Tension Gauge; Haag-Streit Diagnostics). The patients were instructed to wear the elastics 24 hours per day. The elastics were replaced at least once a day. A removable biteplate covering the occlusal surface of maxillary teeth was placed to eliminate occlusal interference in the incisor region until correction of the anterior crossbite was obtained ( Fig 5 ).
In both groups, oral hygiene instructions were reiterated with particular emphasis on brushing the tissues around the miniplates with a soft toothbrush. The decision to discontinue orthopedic treatment in both groups was made by the operator when the patients had 3 to 4 mm of positive anterior overjet.
Cephalometric radiographs were obtained before (T1) and after the maxillary protraction or observation periods (T2) in all groups. All cephalometric radiographs were scanned and analyzed by 1 investigator (M.H.E.) using Dolphin software (version 11.7; Dolphin Imaging and Management Solutions, Chatsworth, Calif). The analysis consisted of the following.
- 1.
Reference system described by Tollaro et al constructed through 2 lines ( Fig 6 ): stable basicranial line that extended from the most superior point of the anterior wall of sella turcica at the junction with tuberculum sellae (point T), drawn tangent to lamina cribrosa of the ethmoid bone; these basicranial structures do not undergo remodeling after the age of 4 to 5 years; and vertical T (VertT), a line constructed perpendicular to the stable basicranial line and passing through point T.
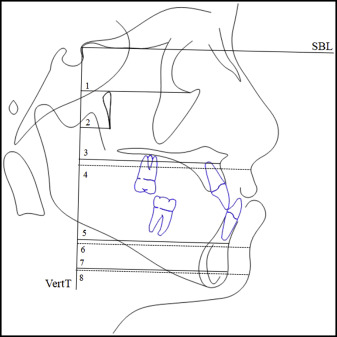
Fig 6 Measurements based on the stable basicranial line and Vert T: 1 , Or-VertT; 2 , Ptm-VertT; 3 , A-VertT; 4 , A′-VertT; 5 , B-VertT; 6 , B′-VertT; 7 , Pg′-VertT. - 2.
Angular measurements (SNA, SNB, ANB, ANO, SN-GoGn, SN-palatal plane, gonial angle, U1-palatal plane, and L1-MP) ( Fig 7 ).
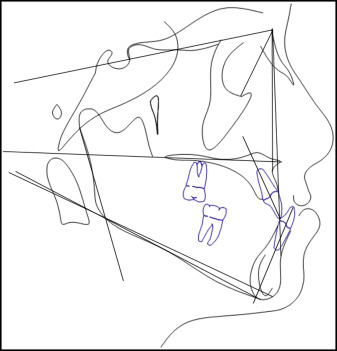
Fig 7 Angular measurements. - 3.
Linear measures (A-Na Perp, Co-A, Co-Gn, U6-VRmx, overjet, and overbite) ( Fig 8 ).
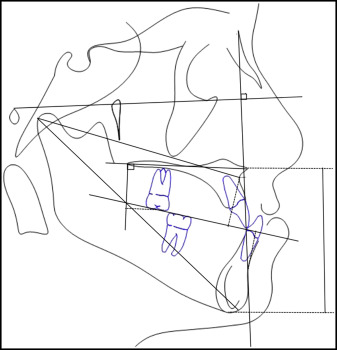
Fig 8 Linear measurements.
To assess the reliability of the measurements, 10 cephalometric radiographs were randomly selected and analyzed 3 weeks after the initial measurements by the same operator. The intraclass correlation coefficients were greater than 0.900 for all variables.
Statistical analysis
The assumption of normal distribution was verified using the Shapiro-Wilk test. One-way analysis of variance followed by 1-sample Student t tests were performed. A P value of ≤0.05 was set to be statistically significant. All calculations and tests were carried out using SPSS Statistics for Windows (version 22.0; IBM, Armonk NY).
The Shapiro-Wilk test showed that most variables in the study had a normal distribution. Descriptive statistics were computed for all variables. Based on the distribution of the raw data, mean differences from the T1 measurements and the differences between the final and initial measurements (T2−T1) among the 3 study groups were investigated using 1-way analysis of variance. For each group separately, a 1-sample t test was performed for the mean differences between time points (T2−T1). Parametric tests were used, and nonparametric tests were performed when needed; similar results were found.
Results
There were no statistically significant differences between the 3 groups at T1 for age and the analyzed cephalometric parameters ( Table I ). There were significant active treatment effects in the changes between T1 and T2 in groups 1 and 2. The changes from T1 to T2 in the 3 groups are shown in Table II and Figures 9 through 14 .
| Parameter | Group 1: MP + FM (group 1) | Group 2: MP + Class III elastics | Group 3: Control | P | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Age (y) | 11.92 | 1.29 | 12.24 | 1.08 | 11.67 | 1.64 | NS |
| Anteroposterior relationship | |||||||
| Or-VertT (mm) | 44.05 | 3.74 | 44.1 | 2.63 | 44.18 | 3.6 | NS |
| Ptm-VertT (mm) | 12.45 | 2.22 | 12.48 | 1.76 | 12.57 | 2.51 | NS |
| A-VertT (mm) | 54.84 | 4.77 | 54.3 | 3.72 | 54.02 | 5.37273 | NS |
| B-VertT (mm) | 52.92 | 5.42 | 52.5 | 4.91 | 52.77 | 5.76 | NS |
| Pg-VertT (mm) | 52.03 | 6.02 | 51.71 | 4.97 | 51.61 | 6.3 | NS |
| SNA (°) | 76.99 | 2.06 | 76.57 | 2.06 | 77.18 | 2.36 | NS |
| SNB (°) | 80.58 | 2.26 | 80.09 | 1.58 | 81.23 | 3.85 | NS |
| ANB (°) | −3.59 | 2.43 | −3.52 | 1.36 | −2.53 | 3.62 | NS |
| SNO (°) | 53.26 | 3.46 | 52.29 | 4.28 | 55.78 | 3.64 | NS |
| (A-Na Perp) (mm) | −4.25 | 1.99 | −4.35 | 1.77 | −4.05 | 3.01 | NS |
| (Co-A) (mm) | 72.34 | 4.95 | 72.16 | 3.74 | 72.81 | 4.43 | NS |
| (Co-Gn) (mm) | 102.86 | 4.97 | 103.06 | 6.24 | 103.82 | 7.04 | NS |
| Wits appraisal (mm) | −8.37 | 2.86 | −8.47 | 1.94 | −8.34 | 3.16 | NS |
| Vertical relationship | |||||||
| LAFH (ANS-Me) (mm) | 57.02 | 3.21 | 59.43 | 4.08 | 60.16 | 4.24 | NS |
| SN-GoGn (°) | 34.71 | 5.52 | 36.23 | 3.66 | 37.17 | 5.02 | NS |
| SN-palatal plane (°) | 9 | 3.57 | 10.91 | 3.05 | 11.12 | 4.1 | NS |
| Gonial angle (°) | 131.52 | 5.86 | 129.95 | 3.87 | 132.42 | 5.78 | NS |
| U1-palatal plane (°) | 116.8 | 6.6 | 117.06 | 6.39 | 115.59 | 7.32 | NS |
| IMPA (L1-MP) (°) | 86.84 | 7.68 | 87.92 | 6.39 | 86.65 | 7.32 | NS |
| Dental relationship | |||||||
| U6-VRmx (mm) | 16.88 | 3.39 | 16.981 | 1.86 | 15.35 | 1.82 | NS |
| Overbite (mm) | 3.67 | 2.61 | 3.07 | 1.69 | 2.45 | 1.93 | NS |
| Overjet (mm) | −4.17 | 1.23 | −4.14 | 1.34 | −3.52 | 1.33 | NS |
| Soft tissue relationship | |||||||
| A′-VertT (mm) | 69.61 | 5.92 | 69.61 | 4.23 | 69.54 | 6.04 | NS |
| B′-VertT (mm) | 68.82 | 5.84 | 67.5 | 5 | 68.12 | 7.07 | NS |
| Pg′-VertT (mm) | 67.07 | 8.67 | 66.01 | 4.94 | 68.24 | 8.55 | NS |
| Parameter | Group 1: MP + FM | Group 2: MP + Class III elastics | Group 3: Control | G 1-2 | G 1-3 | G 2-3 | |||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||||
| Treatment period (mo) | 8 | 1.33 | 8.9 | 2.33 | 9.4 | 1.77 | NS | NS | NS |
| Anteroposterior relationship | |||||||||
| Or-VertT (mm) | 3.03 | 1.77 | 3.88 | 1.7 | 0.61 | 0.54 | NS | † | ‡ |
| Ptm-VertT (mm) | 2.1 | 0.9 | 2.73 | 0.58 | 0.49 | 0.41 | NS | ‡ | ‡ |
| A-VertT (mm) | 4.87 | 1.56 | 5.81 | 1.23 | 1.18 | 0.6 | NS | ‡ | ‡ |
| B-VertT (mm) | −1.45 | 0.32 | −0.67 | 0.35 | 1.67 | 0.45 | ‡ | ‡ | ‡ |
| Pg-VertT (mm) | −1.55 | 0.35 | −0.65 | 0.09 | 1.94 | 0.09 | ‡ | ‡ | ‡ |
| SNA (°) | 4.78 | 1.14 | 5.65 | 0.83 | 0.44 | 0.49 | NS | ‡ | ‡ |
| SNB (°) | −1.21 | 0.85 | −0.39 | 0.59 | 0.89 | 0.7 | ∗ | ‡ | † |
| ANB (°) | 5.99 | 1.54 | 6.04 | 1.16 | 0.82 | 0.68 | NS | ‡ | ‡ |
| SNO (°) | 2.78 | 0.74 | 3.29 | 1.15 | 0.292 | 0.39 | NS | ‡ | ‡ |
| (A-Na Perp) (mm) | 5.55 | 2.45 | 6.07 | 1.29 | −0.73 | 0.6 | NS | ‡ | ‡ |
| (Co-A) (mm) | 4.8 | 1.29 | 5.74 | 1.2 | 1.21 | 2.26 | NS | ‡ | ‡ |
| (Co-Gn) (mm) | 0.95 | 0.25 | 1.74 | 0.37 | 2.12 | 3.34 | NS | NS | NS |
| Wits appraisal (mm) | 7.01 | 2.34 | 7.32 | 1.28 | −1.03 | 1.1 | NS | ‡ | ‡ |
| Vertical relationship | |||||||||
| LAFH (ANS-Me) (mm) | 2.94 | 1.68 | 1 | 0.18 | 1.9 | 1.86 | ∗ | NS | NS |
| SN-GoGn (°) | 2.03 | 0.76 | −0.98 | 0.51 | −0.53 | 0.76 | ‡ | ‡ | NS |
| SN-palatal plane (°) | −0.65 | 0.24 | −0.7 | 0.86 | −0.61 | 1.17 | NS | NS | NS |
| Gonial angle (Ar-Go-Me) (°) | −3.2 | 0.61 | −4.18 | 0.49 | −0.26 | 0.61 | NS | ‡ | ‡ |
| U1-palatal plane (°) | 0.25 | 0.37 | 0.14 | 0.44 | 0.59 | 0.98 | NS | NS | NS |
| IMPA (L1-MP) (°) | −2.56 | 1.76 | 1.1 | 0.18 | 0.42 | 0.22 | ‡ | ‡ | NS |
| Dental relationship | |||||||||
| U6-VRmx (mm) | 0.14 | 0.31 | 0.119 | 0.06 | 0.28 | 0.13 | NS | NS | NS |
| Overbite (mm) | −1.48 | 1.52 | −0.65 | 0.71 | 0.82 | 1.05 | NS | ‡ | ∗ |
| Overjet (mm) | 7.13 | 1.25 | 7.11 | 1.59 | −0.57 | 0.56 | NS | ‡ | ‡ |
| Soft tissue relationship | |||||||||
| A′-VertT (mm) | 5.24 | 1.98 | 6.75 | 2.61 | 1.22 | 0.48 | NS | ‡ | ‡ |
| B′-VertT (mm) | −1.125 | 1.12 | −0.48 | 0.62 | 1.69 | 6.44 | NS | ‡ | NS |
| Pg′-VertT (mm) | −1.08 | 0.87 | −0.72 | 0.62 | 1.83 | 0.2 | NS | ‡ | ‡ |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


