Figure 11.1. Types of cleft lip deformities. Upper left illustration from Veau V. Bec-de-Lièvre: Formes Cliniques — Chirurgie. Paris: Masson et Cie; 1938.
The same process that produced the cleft can also cause other congenital anomalies. In fact, 35% of all infants with cleft lip and palate have additional associated anomalies. This incidence rises to 54% for infants with a cleft palate alone.5 Therefore, when evaluating a patient with cleft lip and palate, it is necessary to perform a thorough examination.6
Periodically, such anomalies occur together and are named after their descriptor, as there is no apparent singular cause. Presumably, the multiple anomalies that make up the syndrome are related. Numerous syndromes have been delineated that involve orofacial clefting.6,7 As research in genetics grows, the source of some of these syndromes has been isolated. The most common syndrome to be associated with cleft palate is Stickler syndrome (mutation of collagen genes COL2A1, COL11A1, or COL11A2).8 Other common syndromes include Shprintzen (velocardiofacial syndrome; 22q11 micro-deletion) and van der Woude (IRF6 mutation) syndromes.9–11
With the increasing sophistication of ultrasonography, the anatomy of the lip can now be discerned prenatally. If a complete cleft is present, it may be detected by 16 weeks, and an incomplete cleft can be detected by 27 weeks.12 A prenatal consultation with the mother can help allay her fears and offer expectations for surgical treatment. Obstetric anxiety can also be reduced with a simple statement of hope, describing accomplishments of other children with cleft lip and palate, “. . . and she plays the trumpet.”
Once a child is born with a cleft, the most pressing concern is feeding. Since they are unable to form a seal around the nipple to produce adequate negative pressure required for sucking, these infants are faced with an immediate problem. This can be ameliorated by using a modified nipple (wider aperture and squeeze chamber), such as a Haberman nipple, as well as several others that are commercially available.
After the baby is able to feed and demonstrates growth, surgical correction can be contemplated. Wilhelmsen and Musgrave emphasized the “rule of 10”: weight 10 pounds, hemoglobin 10 g, age 10 weeks.13 In general, however, in a wide cleft of the lip, the option of a lip adhesion may be considered before definitive lip and nasal correction. If the lip adhesion is performed after 10 weeks, a definitive repair can be scheduled 2 to 3 months later.
Before any attempt to correct a deformity, the norm has to be correctly understood. Farkas has documented the normal anthropometry of the face in detail.14 By using this guide, a lip may be constructed to achieve optimal results. It is crucial to maintain photographic and numeric records, so that an accurate assessment can be done on the results of a surgeon’s protocol. Newer three-dimensional anthropometry systems are particularly convenient as they can record accurate measurements in a split second.15
11.2 Unilateral Cleft Lip and Nasal Deformity: Surgical Principles
Alexander Limberg first described the concept of extending a rotational flap with the help of a back-cut.16 Several geometric repairs had been proposed to correct the deficient length of the medial (noncleft) side of the cleft lip. Being dissatisfied with the obvious scars and distortion of key features of the upper lip, Millard proposed using the rotation flap with a back-cut to lengthen the medial portion of the cleft lip.2,17 This hid the scar along the reconstructed philtral column and was flexible enough to be modified according to the length of the lip. The lateral lip was then advanced across the cleft to complete the closure. This constituted the rotation-advancement correction of the cleft lip, which has withstood the test of time.18,19 The Millard rotation advancement flap and its variants are the most common methods of cleft lip repair today.
The following principles have been proposed to correct a unilateral cleft lip: (1) symmetry — staged procedures result in better symmetry in the wide unilateral cleft; (2) primary muscular continuity — the abnormal insertion of the orbicularis oris along the cleft edge at the base of the nose is horizontally reoriented across the cleft; (3) proper philtral shape — the rotation flap is hidden along the neophiltrum, and extension of this flap to the opposite philtrum is avoided; (4) augmenting the median tubercle from lateral lip elements — white-roll and vermilion flaps are inserted into the medial, deficient counterparts; (5) primary nasal correction — a C flap is used to augment the hemicolumella, and correct the positioning of the alar cartilage and alar base.2,20
11.2.1 Surgical technique markings
Important landmarks of the lip and nose should be marked (Figure 11.2). On the lateral side, the subalar point (sbal) on the affected side is marked first. Note that the sbal will be splayed laterally secondary to the under-rotated alar base of the cleft nose. The most important point to mark is the Cupid’s bow peak (cphi) on the lateral side. To obtain a desirable result, an equal vertical length of the cutaneous upper lip must be achieved. Landmarks unaffected by the cleft are the sbal and the cphi on the unaffected side. Therefore, this length should serve as a template for the affected side. Calipers are useful to first determine the length of the upper lip on the unaffected side (sbal to cphi), and then to mark the cphi on the affected side by marking the point where the arc of the length of the lip meets the vermilion–cutaneous (white roll) junction. The horizontal length between the cphi and its ipsilateral commissure, or chelion, is recorded. However, it has been shown that a short preoperative horizontal distance lengthens after correction of the complete oral sphincter.20,21 Once the cphi on the affected side has been determined, the marking can be made for the rotation and advancement flaps.22
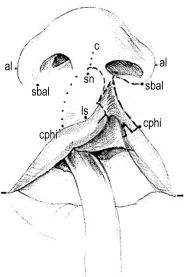
Figure 11.2. Important landmarks and markings for a unilateral cleft lip repair. On the medial element, Cupid’s bow peaks (cphi) and low-point (ls), philtral column, subalar point (sbal), subnasal point (sn), lateral alar point (al), and midline of the columella (c). Note that the sbal–cphi distance should be equal on both sides of the cleft. Reprinted with permission from Wolters Kluwer Health in Ref. 20. Copyright © 1999 American Society of Plastic Surgeons.
The rotation flap is marked along the medial margin of the cleft curving toward the columella. The advancement flap is marked on the lateral lip from the proposed cphi to the nasal sill along the cleft margin and is extended to the alar base. The columellar flap (C flap) is marked from the superior edge of the rotation flap to the membranous septum. This flap will be used to augment the hemicolumella and reconstruct the nasal sill. Attention then turns to the vermilion and mucosa of the lip. The vermilion is deficient on the medial edge of the cleft; therefore, a triangular flap of vermilion is designed at the vermilion–mucosal junction (“red line”). The labiobuccal mucosa is also deficient; a triangular flap of mucosa is planned from the lateral lip to elongate it. A gingivobuccal incision is planned from the cleft edge to raise the cheek flap for advancement across the cleft. A third triangular flap carrying the white roll will be designed just before closure of the philtral incision (Figure 11.2).20,23,24
11.2.2 Dissection
Incisions are made along the markings, and the mucosa lining the cleft is discarded. The buccal sulcus incision is made, although it does not extend to the level of the parotid duct. A supraperiosteal dissection is performed on the maxilla up to the level of the infraorbital foramen. If a lip adhesion has been performed previously, extensive maxillary dissection is not necessary. The alar base is elevated along with this flap off the piriform rim. The orbicularis is first separated from its anomalous attachment to the alar base, then dissected away from skin and mucosa of the lip. A mucosal back-cut in the buccal sulcus assists in advancing the lateral lip elements across the cleft. Scissors are placed between the medial crura (under the columellar flap), and blunt dissection is used to separate it from the opposite medial crura and dome. A sharp back-cut at the top of the rotation flap (on the columella, toward the opposite philtral column) is then created while the affected nostril is held at optimal level with a retractor. The back-cut is performed till the cphi are level.23 If not addressed during a lip adhesion, the septal mucoperichondrium and the lateral vestibular mucosa are elevated for nasal floor reconstruction.20,22
11.2.3 Closure
The nasal floor is closed by approximating the septal mucoperichondrium and the lateral vestibular mucosa. While retracting the nostril to a level symmetric to the contralateral side, the columellar flap is retrogressed into the hemicolumella. The alar base flap is rotated endonasally and is approximated (end-to-side) to the columellar flap to form the nasal sill. The buccal sulcus is closed after advancing the back-cut. A triangular mucosal flap at the leading edge of this flap is interdigitated into the labial frenum to augment the mucosa on the cleft side. The buccal side of the lip mucosa is then closed. The orbicularis oris is then apposed from an inferior to a superior accession. The most superior portion of the orbicularis is affixed to the anterior nasal spine to create the appearance of a pout.20,22
The alar base is secured to the underlying orbicularis muscle to a point where the interalar distance is symmetric. The cutaneous closure of the lip starts at the vermilion–cutaneous junction. A small triangular flap (the white-roll flap) is inserted into a releasing incision on the medial side to complete the white roll and dictate the balance of the Cupid’s bow.2 The triangular flap of vermilion is inserted into a releasing incision along the vermilion–mucosal line (wet–dry junction or red line) to complete closure of the mucosa of the upper lip.24 The advancement flap is then trimmed to a convex shape and is closed to the rotation flap in an inferior-to-superior direction. The subnasal portion of the incision is trimmed as needed and closed along the nasal sill. The distal edge of the advancement flap is trimmed and inserted into the superior portion of the philtral incision without any tension.
Through a marginal incision, the lower lateral cartilage is exposed. Using a cotton-tipped applicator, the contralateral dome is delivered through the marginal incision; an interdomal suture is placed between this spot and the proposed dome of the affected cartilage. The lateral portion of the lower lateral cartilage is suspended from the ipsilateral upper lateral cartilage to reconstruct the scroll (which is usually separated due to the stretch across a complete cleft; however, it may be intact in an incomplete cleft and therefore unnecessary). Correction of the alar cartilage usually results in redundancy or webbing of the vestibular mucosa and warrants a lenticular excision to open up the nostril. If necessary, a crescentic excision may be performed just superior to the marginal incision before closure in order to remove some of the stretched, excess skin of the nostril (Figure 11.3).20,23

Figure 11.3. Closure of a unilateral cleft lip. Triangular flaps are used to complete the white roll and to augment the vermilion on the medial side. A resorbable splint can be used (after interdomal apposition of the lower lateral cartilages) to maintain the nasal correction.25 Reprinted with permission from Wolters Kluwer Health in Ref. 25.
11.2.4 Nasal correction
Primary correction of the nasal deformity is prescribed in all clefts. Internal resorbable sutures are recommended. The use of percutaneous sutures yields a nonanatomic correction, and the use of bolsters is inadequate since they are usually removed in a week (cartilage healing takes considerably longer).
Owing to incisions along the columella, nasal floor, alar base, and nostril roof (marginal incision), a circumferential contraction of scar can lead to nostril stenosis. To avoid nostril stenosis, a postsurgical silicone conformer can be used during the healing phase.26 However, an external splint is usually not tolerated by infants and can also cause frictional abrasions and pressure-related ulcerations. To address these challenges, Wong et al. recommend the use of an internal resorbable splint.25 A resorbable plate can be placed over the corrected cartilage to act as an internal splint (Figure 11.3). This splint obviates the need for an external conformer or preoperative nasal molding.25
11.2.5 Dentofacial orthopedics
There are a variety of options for presurgical treatment of the alveolus. They vary depending on expertise, accessibility, finances, and individual protocols. There are three basic methods of presurgical molding: (1) taping, (2) passive molding, and (3) active orthopedic devices. Taping is the simplest method, with external force placed by gradual approximation of the cleft edges of the lip with adhesive tape. A dental plate may be used in conjunction with taping to prevent collapse of the lesser segment. However, accurate alignment is challenging, and dermatitis and epidermolysis from frequent tape removal can be annoying.27 Alveolar approximation is also possible by progressive molding of a dental plate. The dental plate is held in place with an adhesive and gradually shaved on the palatal surface. External force by taping assists in moving the arches along this molded surface. Since infant cartilage can be molded nonsurgically, a nasal phalange is added when the interalveolar distance is less than 6 mm. This nasal molding bulb is progressively straightened to achieve an excellent preoperative position of the affected lower lateral cartilage. Usually, this process takes 10 to 12 weeks. A simultaneous correction of the lip, nose, and alveolus (gingivoperiosteoplasty) is possible after nasoalveolar molding.28
An active dentomaxillary appliance accomplishes alveolar alignment much more quickly (3–5 weeks). A custom-made prosthesis is secured to the palate with pins (under anesthesia). A screw is turned daily to activate an arm that moves the lesser segment along the radius of the arm. An auxiliary elastic chain can be engaged to assist in decreasing the interalveolar gap. A stronger force is applied on the maxillary segments for proper positioning.28,29 Presurgical orthopedics effectively narrows the cleft, facilitating primary repair and decreasing the need for secondary repair.30 No long-term effects have been noted with use of dentofacial orthopedics.31
11.2.6 Lip adhesion
A lip adhesion can be a useful adjunct in the treatment of a complete cleft lip.32 An adhesion may be used instead of or in conjunction with dentofacial orthopedics. If access to presurgical orthopedics is unavailable, a lip adhesion can be performed as a staged procedure to narrow the cleft and approximate the dental arches, allowing for staged correction of the nasal deformity. This may decrease the number of secondary procedures necessary.20,32,33 However, many centers have abandoned a preliminary adhesion as it may increase exposure to anesthesia, complications, scarring, and cost.34,35
Markings for a lip adhesion are made beyond any landmarks that are important for the ultimate cleft lip repair. On the medial side, a linear incision is marked 2 mm beyond the vermilion–cutaneous junction that extends along the base of the caudal septum. On the lateral side, a similar, corresponding incision is marked in the lip (beyond the vermilion–cutaneous junction) to the level of the piriform. A perpendicular incision is marked from the vestibular–piriform margin along the lateral buccal sulcus. The lip incisions are made to the level of the submucosa until the underlying muscle is visualized. However, the muscle is not dissected. The cheek is elevated along the supraperiosteal plane so it may be advanced across the cleft for a tension-free closure. A back-cut in the mucosa greatly assists in advancing the flap along the buccal sulcus, and the posterior mucosa of the adhesion is closed. The nasal floor is constructed by apposing the septal mucoperichondrium and the lateral vestibular mucosa. Interrupted sutures are placed in the muscular layer and the anterior mucosa is carefully approximated. Thin adhesive skin-closure strips (Steri-strips) reduce the tension across the adhesion in the immediate postoperative period. Typically, the final correction of the cleft lip is delayed for 2 to 3 months after the adhesion.20,33
11.2.7 Gingivoperiosteoplasty
Efforts to close the cleft alveolus primarily (with bone grafts) may produce detrimental effects on maxillary growth, especially if dissection is aggressive. Primary bone grafting has been abandoned at most institutions.36 However, an unrepaired alveolar cleft can result in fluid and air leakage. One option to close the cleft alveolus is a gingivoplasty or gingivoperiosteoplasty.2,28 After approximation of the arches with dentofacial orthopedics, local gingival tissue can be used with limited undermining to close the alveolar cleft. A gingivoperiosteoplasty effectively closes the alveolar cleft and completes the dental arch to provide a stable platform for nasal correction and tooth eruption.
More commonly, the alveolar cleft is left untreated until secondary bone grafting. Typically, secondary alveolar bone grafting is performed at a stage of mixed dentition, when the canine root has not fully formed (ages 8–10). A bone graft is performed to provide bony support for the teeth adjacent to the cleft and a dental implant (for the missing lateral incisor), or to allow for movement of the permanent canine into the lateral incisor position. Secondary grafting is successful using cancellous bone from the iliac crest.37
11.2.8 Controversy of adjunctive treatment in cleft lip and nasal deformity
Anecdotally, the incomplete cleft is easiest to correct. The dental arches are well aligned, the alar base is in a good symmetric position, and there is greater orbicularis bulk secondary to tension from partial completion of the oral sphincter.33 In fact, just the presence of a skin bridge across the cleft (Simonart’s band) greatly minimizes the severity of the cleft. Based on these observations, Millard et al. introduced a protocol to convert a complete cleft to an incomplete cleft.38 A dentofacial appliance is first used to approximate the dental arches. Then, a lip adhesion and gingivoperiosteoplasty are performed to set up the foundation for correction of a complete cleft. This protocol has the advantages of arch alignment, preferred alar base position, and increased muscle bulk, as well as a slight lengthening of the medial element of the lip.33 This can reduce the length of the back-cut necessary for the rotational flap so that it does not encumber the lip or philtrum on the normal side. Staged correction of the nasal deformity also yields better and more consistent results (Figure 11.4).
Alignment of the arches may be performed by either active or passive dentofacial orthopedics.28
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


