Correcting a Class III subdivision malocclusion is usually a challenge for an orthodontist, especially if the patient’s profile does not allow for any extractions. One treatment option is to use asymmetric intermaxillary elastics to correct the unilateral anteroposterior discrepancy. However, the success of this method depends on the individual response of each patient and his or her compliance in using the elastics. The objectives of this article were to present a successful treatment of a Class III subdivision patient with this approach and to illustrate and discuss the dentoskeletal changes that contributed to the correction.
Orthodontic treatment of adult Class III patients is difficult, especially if the malocclusion is asymmetric. A precise diagnosis of the dentoskeletal components of the malocclusion associated with the patient’s primary concern is essential for correct treatment planning. Similar to correction of Class II subdivision malocclusions, Class III subdivision malocclusions can have a variety of orthodontic treatment options such as nonextraction protocols with intermaxillary elastics, unilateral extraction of 1 mandibular premolar on the Class III side, or extraction of 2 mandibular premolar extractions and 1 maxillary premolar extraction on the Class I side. Malocclusion correction based on the use of intermaxillary elastics is difficult and controversial. However, if it is well indicated in a compliant patient, it can provide satisfactory results. Therefore, the objective of this article was to present the successful orthodontic treatment of a Class III subdivision patient with asymmetric intermaxillary elastic forces. This procedure allowed obtaining a good and stable occlusal relationship and a better esthetic facial profile and smile for the patient.
Diagnosis and etiology
The patient was a man (age, 23 years 11 months) with a Class III subdivision left malocclusion with negative overjet and facial imbalance. His chief concerns were his anterior crossbite and lower lip protrusion. His parents had no Class III characteristics.
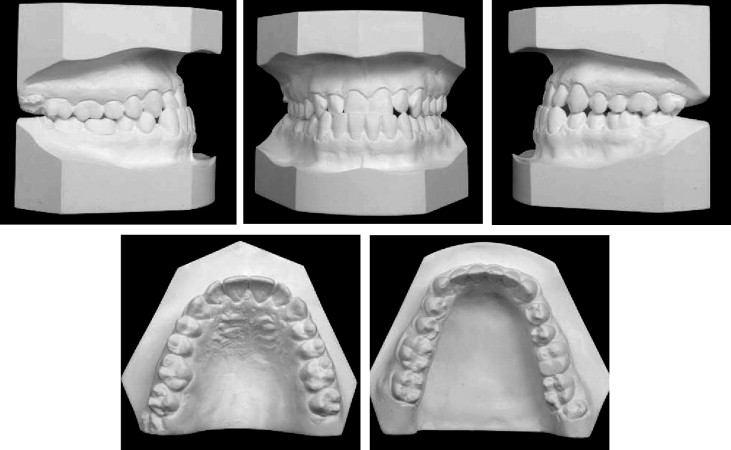
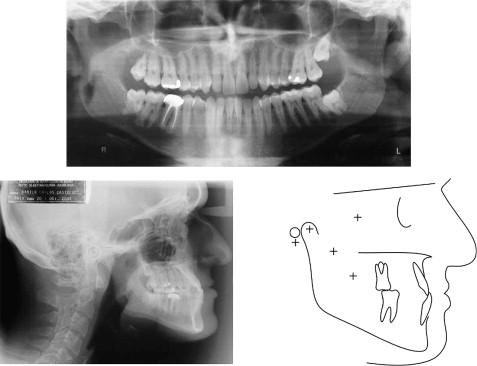
The facial photographs showed a prognathic mandible and a Class III appearance ( Fig 1 ). The patient could close his lips without mentalis strain, but he was self-conscious about the way his teeth occluded and the appearance of his teeth. The pretreatment intraoral photographs and dental casts show a Class III subdivision malocclusion with Class I on the right and Class III on the left ( Figs 1 and 2 ) . There was good alignment of the mandibular incisors, and all teeth were present including the third molars ( Fig 3 , A ) . Cephalometrically, he had maxillary retrusion, slight mandibular protrusion, and a balanced facial pattern, with the exception of excessive lower anterior face height. The maxillary incisors were bucally tipped and protruded, and the mandibular incisors were lingually tipped and retruded. He had an acute nasiolabial angle ( Fig 3 , B and C ; Table ).

| Measurement | Standard measurement | Pretreatment | Posttreatment | Two-year follow-up |
|---|---|---|---|---|
| Maxillary components | ||||
| SNA ( o ) | 82 | 75.4 | 76 | 76 |
| Co-A (mm) | 85 | 85 | 85 | 85.4 |
| A-Nperp (mm) | +1 | −8.0 | −8.2 | −8.5 |
| Mandibular components | ||||
| SNB ( o ) | 80 | 81 | 78.5 | 79.0 |
| Co-Gn (mm) | 108 | 119 | 119 | 119 |
| P-Nperp (mm) | −2 /+4 | −5.1 | −7.2 | −7.0 |
| Maxillomandibular components | ||||
| ANB ( o ) | 2 | −5.6 | −2.5 | −3.1 |
| Wits (mm) | 0 | −7.7 | −4.7 | −6.4 |
| Growth pattern | ||||
| FMA ( o ) | 25 | 25 | 27 | 26.4 |
| SN.Ocl ( o ) | 14 | 12 | 11 | 11.9 |
| SN.GoGn ( o ) | 32 | 29 | 31.4 | 30.4 |
| LAFH (mm) | 62 | 65.5 | 65.8 | 65.6 |
| Maxillary dental components | ||||
| Mx1.NA ( o ) | 22 | 31 | 38 | 40.1 |
| Mx1-NA (mm) | 4 | 7.5 | 9 | 9.2 |
| Mx1.PP ( o ) | 112.1 | 118.3 | 125.5 | 127.4 |
| Mx1-PP (mm) | 33.0 | 26.1 | 25.1 | 25.6 |
| Mx6-PP (mm) | 27.9 | 24.7 | 25.6 | 25.0 |
| Mandibular dental components | ||||
| Md1.NB ( o ) | 25 | 16 | 14 | 14.9 |
| Md1-NB (mm) | 4 | 1.6 | 0.3 | 0.8 |
| IMPA ( o ) | 95.3 | 80 | 78 | 79.0 |
| Md1-GoMe (mm) | 48.9 | 39.0 | 39.2 | 39.3 |
| Soft-tissue components | ||||
| Nasolabial angle ( o ) | 110 | 91 | 90 | 88.9 |
| Upper lip to S Line (mm) | 0 | 0.8 | 1.3 | 1.8 |
| Lower lip to S Line (mm) | 0 | 2.3 | 1.9 | 2.1 |
Treatment objectives
The treatment objectives consisted of correcting the Class III canine and molar relationships on the left side, the dental anterior crossbite, the midline deviation, and the prognathic appearance of the mandible. Functionally, we sought to obtain normal canine and incisal guidance and an esthetic smile.
Treatment objectives
The treatment objectives consisted of correcting the Class III canine and molar relationships on the left side, the dental anterior crossbite, the midline deviation, and the prognathic appearance of the mandible. Functionally, we sought to obtain normal canine and incisal guidance and an esthetic smile.
Treatment alternatives
Two treatment alternatives were presented to the patient. The first consisted of an orthodontic-surgical approach including maxillary advancement. This protocol would provide a better esthetic result, but the risks and treatment expenses would be high. The second alternative consisted of attempting to correct the asymmetric malocclusion with asymmetric intermaxillary elastics. If the elastics were ineffective, extraction of the mandibular left premolar would assist in correcting the canine Class III relationship on the left side. This option would provide excellent occlusal results, but improvement of the facial profile would be limited. Because dental appearance was the patient’s chief concern, he chose the orthodontic treatment protocol.
Treatment progress
Fixed conventional 0.022 × 0.025-in slot edgewise appliances were placed to level and align the maxillary and mandibular arches. The archwire sequence progressed from 0.016-in nickel-titanium alloy to 0.019 × 0.025-in rectangular stainless steel archwires. Concurrently, Class III intermaxillary elastics were combined with anterior diagonal elastics ( Fig 4 ). Class III elastics with rectangular archwires were used for 12 months. After the anteroposterior discrepancy correction, the elastics were used during sleeping hours for 5 months until appliance removal. Patient cooperation in using the elastics was excellent. Treatment time was 2 years 3 months. After debonding, a maxillary Hawley retainer was delivered, and a mandibular canine-to-canine retainer was bonded.




