This case study describes the retreatment and long-term follow-up care of a patient with a medical history of 2 heart surgeries and a Class II malocclusion that included a severe anteroposterior skeletal discrepancy characterized by mandibular deficiency. The patient’s initial orthodontic camouflage treatment was poorly performed and failed to correct the maxillofacial disorders. In this article, we report the successful retreatment with a surgical-orthodontic protocol and include the 5-year follow-up records showing stable results. Guidelines for the stratification of cardiac risk are included.
Elective dental treatment, except for conservative emergency procedures, has traditionally been contraindicated in patients who have experienced unstable angina and acute myocardial infarction during the previous 6 months. The American College of Cardiology and the American Heart Association published risk stratification guidelines for professionals who are performing several types of noncardiac surgical procedures in patients with various cardiopathologies. This topic is important for orthodontists because more orthodontic patients have a history of heart disease or surgery; these guidelines emphasize how a dental treatment plan should be established to ensure that reasonable and safe decisions are made and specifically to determine with confidence whether a patient will be able to tolerate a planned procedure. For example, surgical orthodontic treatment for maxillomandibular disharmony could be indicated for a patient with a history of acute myocardial infarction as long as the patient is stratified as having a low cardiac risk.
Over the past few years, great progress has been made in surgical orthodontic protocols for the treatment of malocclusions with skeletal involvement that had previously been arbitrarily addressed by orthodontic camouflage. Camouflaging sometimes achieves limited results, unacceptable facial esthetics, or unstable occlusal contacts that do not meet the patient’s expectations.
In this article, we present guidelines for the stratification of cardiac risks. We also present 5 years of follow-up care for a patient with a Class II malocclusion, mandibular deficiency, and a medical history of 2 heart surgeries, who was treated with a surgical-orthodontic protocol after a poorly performed orthodontic camouflage treatment.
Diagnosis and etiology
A 30-year-old woman came for an initial examination in a generally good state of health. Her medical history indicated that she was a cardiac patient with 2 previous heart surgeries (internal thoracic artery and myocardial revascularization). Her cardiac risk stratification for extensive maxillofacial surgical procedures, such as orthognathic surgery, was intermediate according to Eagle et al, with an overall reported cardiac risk below 5%. Parafunctional habits were not considered, except lingual interposition during swallowing. Unsatisfactory facial esthetics and masticatory function were the patient’s chief complaints, especially in the tearing of foods with the anterior teeth. The patient’s dental history showed the loss of the mandibular right first and second molars because of caries and the extraction of the maxillary right and left first premolars during the previous orthodontic treatment, with the unattained goal of correcting an overjet caused by mandibular deficiency.
The facial evaluation of the patient showed an absence of labial seal at rest and an inverted contour of the upper lip, indicating an esthetic deficiency. The soft-tissue profile was convex, and the nasolabial angle was harmonious. There was also a general appearance of premature aging ( Fig 1 ).

The intraoral clinical examination and an evaluation of the orthodontic documentation supported the diagnosis of a Class II malocclusion ( Figs 1 and 2 ) with an accentuated anteroposterior maxillomandibular discrepancy (ANB, 8.5°; SNA, 74.5°; SNB, 66°), with greater mandibular retrusion than maxillary retrusion ( Fig 3 ). The convex bone profile was accentuated (convexity, 11.5°), the direction of growth was severely vertical (y-axis, 64.5°; SN-GoGn, 47°), and there was transversal skeletal atresia of the maxilla, with an intercanine distance of 30.7 mm and an intermolar distance of 44.9 mm.
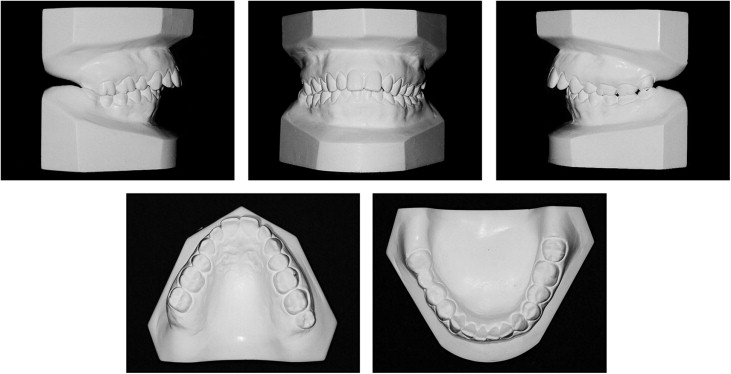
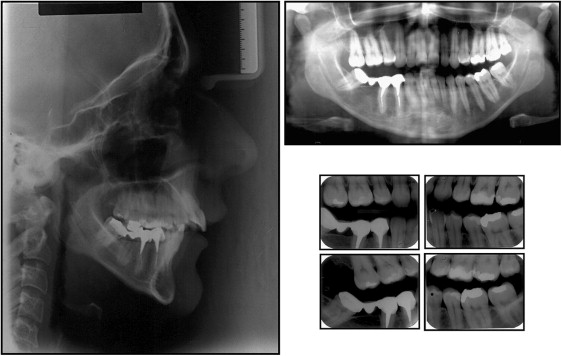
Dental evaluation showed an excessive overjet (11.5 mm) and an overbite of 5.5 mm. There was a slight deviation to the right of the mandibular midline and an accentuated mandibular curve of Spee ( Fig 1 ). The maxillary incisors appeared to be slightly vestibularized and protruded (1-NA, 24°, and 1-NA, 5.5 mm, respectively), and the mandibular incisors were lingualized (1-NB, 20.5°) ( Fig 3 ). The patient had a poorly planned fixed bridge with abutments on the mandibular right first and second premolars and third molar, which interfered with the protrusive function of the mandible by the third molar.
Evaluation of the panoramic radiograph showed the absence of the maxillary right third molar, the mandibular left third molar, and the mandibular right first and second molars ( Fig 3 ); distal positioning of the abutment of the fixed bridge on the mandibular right third molar; the mesioangular and extrusive position of the mandibular right third molar; and root dilaceration of the mandibular right second premolar ( Fig 3 ).
Treatment objectives
The patient had a medical history of 2 surgeries and previous orthodontic camouflage treatment, including the extraction of the maxillary first premolars, and was motivated to follow the proposed treatment plan, which included a combined surgical-orthodontic protocol.
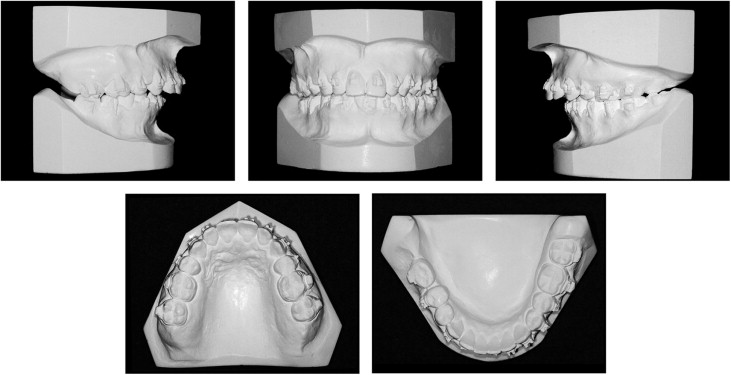
Surgical disjunction to correct the maxillary atresia was conducted at a separate time, because of the large discrepancy, so that the patient would not be subjected to a long surgery (in a combined surgery) and to prevent the risk of maxillary segmentation, which would cause a more complex scarring process. A slight vestibular torque was measured for the incisors, and increases in the intercanine and intermolar distances were observed.
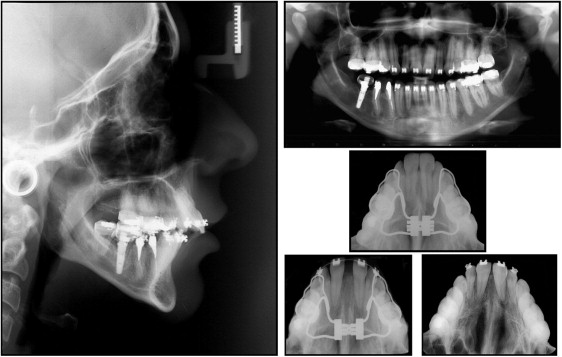
Mandibular retrusion was corrected by orthognathic surgery (bilateral sagittal split osteotomy maintaining the vertical component). Intrusion of the anterior mandibular teeth was planned using segmented mechanics to correct the curve of Spee. The removal of the fixed mandibular bridge and the placement of an implant in the space for the mandibular right first molar was also planned.
Treatment objectives
The patient had a medical history of 2 surgeries and previous orthodontic camouflage treatment, including the extraction of the maxillary first premolars, and was motivated to follow the proposed treatment plan, which included a combined surgical-orthodontic protocol.
Surgical disjunction to correct the maxillary atresia was conducted at a separate time, because of the large discrepancy, so that the patient would not be subjected to a long surgery (in a combined surgery) and to prevent the risk of maxillary segmentation, which would cause a more complex scarring process. A slight vestibular torque was measured for the incisors, and increases in the intercanine and intermolar distances were observed.
Mandibular retrusion was corrected by orthognathic surgery (bilateral sagittal split osteotomy maintaining the vertical component). Intrusion of the anterior mandibular teeth was planned using segmented mechanics to correct the curve of Spee. The removal of the fixed mandibular bridge and the placement of an implant in the space for the mandibular right first molar was also planned.
Treatment alternatives
A dental plan for the correction of the mandibular deficiency using dental compensation (orthodontic camouflage) had been attempted previously with little success. A surgical-orthodontic protocol for the correction of the Class II defects was considered to have the greatest likelihood of restoring the patient’s esthetics and correcting the dental malocclusion.
The cardiologist, an anesthesiologist, and an oral maxillofacial surgeon discussed the direction of the orthognathic surgery and preventive measures, and treatment decisions were made according to the cardiac risk stratification to ensure the safety of the procedure (<5% risk). These measures included control of arterial pressure and anxiety and the temporary discontinuation of the patient’s anticoagulant medications.
Treatment progress
A hyrax palatal expander was placed, and the patient underwent osteotomy surgery through the lateral maxillary wall and the median palatine suture, according to previous protocols. The protocol called for 1 complete turn of the expanding screw on the first day and subsequent quarter turns in the morning and at night after the second day (twice a day) for 10 days. Once expanded, the apparatus was left in place for passive retention for 4 months. The dental implant was placed in the space for the mandibular right first molar during the maxillary surgery to create a skeletal anchor, and the patient’s accentuated mandibular curve of Spee was corrected through the intrusion of the anterior mandibular teeth using the segmented-arch technique.
During the restraint phase of the disjunction, the mandibular dental arch was leveled with minimum proclination of the incisors; this is fundamental for mandibular advancement. The apparatus used had an MBT prescription and a 0.022 × 0.028-in slot (Abzil Ind. e Com. Ltda, São Paulo, Brazil). The orthodontic leveling of the maxillary and mandibular arches was performed with nickel-titanium 0.014- and 0.016-in arches and stainless steel 0.016-, 0.018-, 0.020-, and 0.019 × 0.025-in archwires to prepare the dental arches.
Figures 4, 5, and 6 show the dental and facial modifications before surgery, the predictive tracing over the cephalometric radiograph, the surgical models mounted on a semiadjustable articulator, and the fabrication of the surgical splint.


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


