Introduction
The Herbst appliance has been used in the treatment of Class II malocclusions with deficient mandibles. Various protocols, including different durations of the orthopedic treatment phase and stepwise advancement of the mandible, have been advocated for increasing the orthopedic effects. The objective of this study was to investigate the skeletal and dental changes in patients treated with a reinforced banded Herbst appliance for an extended duration and fixed appliance therapy.
Methods
The study group consisted of 30 patients (16 boys, 14 girls; mean age, 12.3 ± 2.5 years) with Class II Division 1 malocclusions who were successfully treated with the new Herbst protocol followed by fixed appliances. Lateral cephalometric radiographs were taken before treatment, at the completion of Herbst treatment, and after removal of fixed appliances. The average treatment times were 1.5 ± 0.7 years for the Herbst treatment and 1.8 ± 0.5 years for the fixed appliances. A control Class II sample from the Bolton-Brush study was used to subtract growth from treatment changes to determine the appliance effect. Data were analyzed using analysis of variance and the Tukey-Kramer test.
Results
After the Herbst treatment, the incisal relationships of all subjects had been overcorrected to end-to-end relationships. Overjet was reduced by 7.2 mm after subtracting changes from growth. The skeletal contribution was 2.5 mm (35%), and the dental contribution was 4.7 mm (65%). The molar relationship was overcorrected to a more Class I relationship by 7.5 mm. The Wits appraisal was improved by 4.2 mm. Vertically, overbite was decreased by 3.3 mm. The maxillary and mandibular molars were extruded by 1 mm. The occlusal plane rotated clockwise by 5° with little change in the mandibular plane angle. After the treatment with fixed appliances, the overjet correction was maintained at 7.6 mm. The skeletal contribution was 2.9 mm (38%), and the dental contribution was 4.7 mm (62%). The molar relationship was corrected to a Class I relationship by 5.9 mm. The Wits appraisal was improved by 3.2 mm. Vertically, overbite was decreased by 4.2 mm. The maxillary and mandibular molars were extruded by 0.3 and 0.8 mm, respectively. The occlusal plane rotated clockwise by 1.2° with little change in the mandibular plane angle.
Conclusions
Doubling the usual orthopedic treatment time with the reinforced Herbst appliance followed by fixed appliance therapy was effective in correcting Class II Division 1 malocclusions with excess overjet and overbite. In this sample of successfully treated patients, most changes after Herbst and fixed appliance therapy were dentoalveolar (62%). However, the skeletal changes attained in the orthopedic phase of treatment were maintained after fixed appliance therapy.
Highlights
- •
We increased the average duration of Herbst orthopedic appliance therapy to 1.5 ± 0.5 years.
- •
The appliance was modified to reinforce the Herbst design to minimize breakage.
- •
Herbst therapy was followed by an average of 1.8 years of fixed appliance therapy.
- •
Most skeletal changes during orthopedic therapy were maintained after fixed appliance therapy.
- •
A longer orthopedic phase allowed a more favorable dental and skeletal results after fixed appliance therapy.
The Herbst appliance proposed by Emil Herbst and Hans Pancherz had orthodontic bands to secure the appliance to the molars. These bands were custom-made and much thicker than conventional bands. Clinicians who tried to use conventional bands soon realized that the occlusal forces were too great and the bands would eventually fail. This led to the development of other variations of the Herbst appliance. Bands were eventually replaced by cobalt-chromium alloy cast splints that were cemented with glass ionomer cement, ensuring a precise fit on the teeth. In 1988, Howe and McNamara started using removable acrylic-splint Herbst appliances, with occlusal coverage extending posteriorly from the canines to the first molars on the maxillary arch and full occlusal coverage on the mandibular arch. However, the bonded acrylic splint proved to be too difficult to remove and had the added risk of enamel decalcification. In the late 1980s, Langford introduced the crowned Herbst appliance consisting of stainless steel crowns cemented to the mandibular first premolars and maxillary first molars. Clinicians soon found that the stainless steel crowns do not adapt closely to the teeth and have a tendency for bite opening and interfering with chewing function. Also, they can impinge on the gingivae and can be difficult to remove.
The effects of the Herbst appliance have been published extensively in the literature and systematically reviewed by several authors. The appliance has a restraining effect on maxillary growth similar to headgear. Studies have shown that growth of the maxilla in patients treated with the Herbst is consistently less than in control groups without treatment. The overall size of the maxilla seems to be unaffected by treatment. The effects of the appliance on the mandible, however, are inconclusive. Some studies have suggested that the Herbst appliance increases mandibular length as much as 1.3 to 3.5 mm compared with control groups during 6 to 8 months of treatment. Although vertical condylar growth was unaffected, sagittal condylar growth appeared to increase with treatment. Various protocols, including treatment period, single-step vs stepwise advancement of the mandible, and length of treatment time, have been advocated to stimulate growth of the mandible. However, systematic reviews of the literature with functional appliances have reported that only two thirds of the studies showed clinically significant supplementary elongation in total mandibular length greater than 2.0 mm compared with the control groups. In addition, few studies have investigated the effects after fixed appliance therapy.
Rogers proposed the use of a banded Herbst appliance and doubling the length of treatment with the appliance for long-term stability. A reinforced Herbst appliance was introduced to minimize its breakage associated with the increased length of appliance use. The objective of this study was to investigate the skeletal and dental changes of patients treated with the reinforced banded Herbst appliance during orthopedic treatment and then with fixed appliance therapy.
Material and methods
After obtaining ethical approval from the Institutional Review Board of West Virginia University (protocol number 1405291690) and approval from 2 authors (M.R. and L.A.) for the use of orthodontic records from their office, the records of 100 Class II patients successfully treated with the reinforced Herbst appliance from 2005 to 2012 were retrospectively examined with the following inclusion criteria: convex facial profile, Class II malocclusion with at least a half-step Class II molar relationship, late mixed dentition to early permanent dentition (age, 10-16 years) at the start of treatment, nonextraction treatment, no previous orthodontic treatment, and availability of pretreatment, posttreatment, and final records taken within 12 months after removal of fixed appliances. The exclusion criteria included patients in the primary or early mixed dentition, with craniofacial syndromes or severe facial asymmetry, or with a history of periodontal disease. A total of 30 treated subjects (16 boys, 14 girls) fulfilled these criteria. The average age at the start of treatment was 12.3 ± 2.5 years (range, 10-15 years). The average treatment time with the Herbst appliance was 1.5 ± 0.7 years, and the average treatment time with the fixed appliance was 1.8 ± 0.5 years. The control sample, obtained from the Bolton-Brush study, was matched closely for age, sex, and craniofacial morphology with the experimental sample. No significant differences in craniofacial morphology were found between the 2 groups ( Table I ).
| Variable | T1 | t1 | Mean difference | P value | Significance | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Sagittal (mm) | |||||||
| Olp-Co | 9.32 | 2.85 | 10.0 | 2.2 | −0.68 | 0.1788 | NS |
| Olp-A-pt | 73.59 | 4.72 | 70.3 | 4.2 | 3.29 | 0.1635 | NS |
| Olp-Ms | 50.76 | 4.46 | 49.2 | 3.8 | 1.56 | 0.2327 | NS |
| Olp-Mi | 50.90 | 4.62 | 49.0 | 4.3 | 1.9 | 0.2767 | NS |
| Olp-ls | 81.63 | 5.20 | 77.2 | 5.5 | 4.43 | 0.3368 | NS |
| Olp-li | 74.85 | 5.27 | 71.9 | 4.8 | 2.95 | 0.4952 | NS |
| Olp-Pg | 75.47 | 6.02 | 73.9 | 4.8 | 1.57 | 0.7232 | NS |
| Wits | 3.78 | 2.61 | 0.6 | 1.7 | 3.18 | 0.0643 | NS |
| Vertical (mm) | |||||||
| OLs-A-pt | 30.85 | 3.37 | 26.9 | 2.2 | 3.95 | 0.8119 | NS |
| ANS-Me | 57.86 | 4.94 | 59.0 | 5.1 | −1.14 | 0.9519 | NS |
| Is-NL | 26.88 | 3.05 | 26.0 | 2.6 | 0.88 | 0.9769 | NS |
| Ii-ML | 37.01 | 3.10 | 35.4 | 3.3 | 1.61 | 0.9682 | NS |
| Overbite | 4.44 | 1.44 | 3.1 | 1.4 | 1.34 | 0.8677 | NS |
| Msc-NL | 19.56 | 2.04 | 18.5 | 2.0 | 1.06 | 0.7854 | NS |
| Mic-ML | 26.51 | 2.50 | 27.0 | 2.4 | −0.49 | 0.7226 | NS |
| Angular (°) | |||||||
| SNA | 82.88 | 4.75 | 80.1 | 2.8 | 2.78 | 0.7538 | NS |
| SNB | 77.17 | 3.70 | 75.8 | 2.9 | 1.37 | 0.5209 | NS |
| ANB | 5.71 | 2.15 | 4.3 | 1.3 | 1.41 | 0.2954 | NS |
| SNL-NL | 6.20 | 3.86 | 6.4 | 2.9 | −0.2 | 0.0877 | NS |
| SNL-ML | 29.52 | 4.87 | 33.4 | 4.8 | −3.88 | 0.0923 | NS |
| SNL-OLs | 15.69 | 4.14 | 19.9 | 3.1 | −4.21 | 0.0937 | NS |
| Is/NL | 112.47 | 9.29 | 110.0 | 5.0 | 2.47 | 0.1041 | NS |
| Ii/ML | 97.14 | 5.78 | 95.1 | 7.5 | 2.04 | 0.1801 | NS |
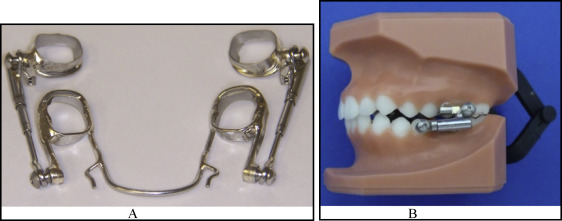
Separators were placed 5 to 7 days before the fitting appointment. At the next appointment, maxillary and mandibular molar bands with facial and lingual cleats prewelded as guides for accurate positioning in an alginate impression were fitted. An alginate impression was taken, and the bands were transferred from the patient, glued in the impression (Great Lakes Adhesive, Tonawanda, NY), and poured up as soon as possible. A wax bite registration was not necessary because the amount of advancement and the midline position were noted on the laboratory prescription. A skeletal midline discrepancy was corrected during Herbst treatment. If there was a dental midline discrepancy, the correction was made after the Herbst was removed and full brackets were placed. The initial advancement was usually 1 to 2 mm short of the edge-to-edge position, and then the mandible was advanced in gradual increments (1 or 2 mm every 8 weeks) until an edge-to-edge or an anterior crossbite position was achieved. A laboratory prescription was completed including any special features requested by the clinician in the Herbst construction. Also, at the fitting appointment, brackets were bonded to the maxillary incisors, and a sectional wire was placed to align those teeth before the Herbst was delivered at the next appointment. This is particularly helpful in patients with a Class II Division 2 malocclusion whose incisors need alignment and advancement. Separators were placed about a week before delivery of the appliance to provide adequate band space. The Herbst appliance was modified by an investigator (M.R.; Fig 1 ). The transpalatal arch was eliminated for added comfort. For stability, buccal archwire tubes were incorporated on the maxillary molar bands, and a larger 0.051-in lingual arch was used on the mandibular arch. Although the thicker 0.010-in bands were less likely to break than conventional bands, 0.051-in reinforcing wires were soldered to the distal occlusal margins of the maxillary and mandibular bands to give them even more bulk and strength. In addition, 0.025-in wires were soldered to the mesial occlusal margins of the mandibular and maxillary bands. Finally, the universal nut and a 0.022 × 0.028-in archwire tube were welded on a 0.020-in unibody plate (Specialty Appliances, Cumming, Ga) and brazed to the mesial area of the maxillary bands, permitting the archwires to be used for alignment and control of the maxillary anterior segment. This design does not require occlusal rests on the second molars because the support wire soldered to the distal surfaces of the maxillary and mandibular bands prevents overeruption of the second molars. Although clinicians have tried to use a cantilever Herbst design with bands, they have reported excessive breakage.
At the insertion appointment, the appliance was tried in the mouth before cementation, with the telescope inspected and shims added if necessary to make sure that the midlines matched the prescription (centered for a skeletal problem or off center for a dental discrepancy). The use of the M-4 telescopes developed by Specialty Appliances eliminated some of the old problems with rods and tubes coming apart and rods impinging on the ascending ramus. The 0.051-in mandibular lingual arch should lie no more than 0.5 mm from the mandibular incisors. If the wire is slightly off the incisors, it will settle against them in several days. Once the fit was satisfactory, the appliance was removed and dried. The maxillary telescopes were secured to the maxillary pivots in the laboratory before trying on the Herbst by placing Ceka Bond (Specialty Appliances) on the screw threads. The mandibular telescopes were secured after cementation. Ceka Bond ensures that the threads will not back out during treatment. Before cementation, the molars were pumiced and cleaned and etched on the buccal aspect only with GC Ortho Conditioner (GC America, Alsip, Ill), a 10% polyacrylic acid solution. Using Fuji I (GC America) band cement, the maxillary molar bands were cemented. A laboratory soldered the upper pivots as far mesially as feasible so that they would not impinge on the ascending ramus. Immediately after the bands were firmly seated, the excess cement was removed with a cotton roll. This saved considerable cleanup time and was more comfortable for the patient.
When arch development is needed, maxillary or mandibular rapid palatal expanders can be added to the Herbst appliance. The maxillary rapid palatal expander should be turned once a day until the desired expansion is achieved; the mandibular screw should be turned once every 4 days. Thumb cribs or tongue prongs for habit control could also be easily incorporated into this Herbst design. The mandible was initially advanced 1 to 2 mm short of the edge-to-edge position and reactivated by adding shims 1 to 2 mm every 8 weeks until an overcorrected Class III canine relationship was achieved. An advantage of the Herbst is that patients and parents can immediately see improvement in the facial profile; this boosts their enthusiasm and cooperation. One great advantage with this design, however, is its ease of removal when the Herbst phase of treatment is finished. The mandibular screws were removed, and the maxillary telescopes were left attached during removal. The mandibular arch and bands were then taken out with a band-removing plier. The maxillary anterior brackets, archwires, telescopes, and bands were removed as a unit, reducing the risk of a patient’s swallowing a band or a compontent.
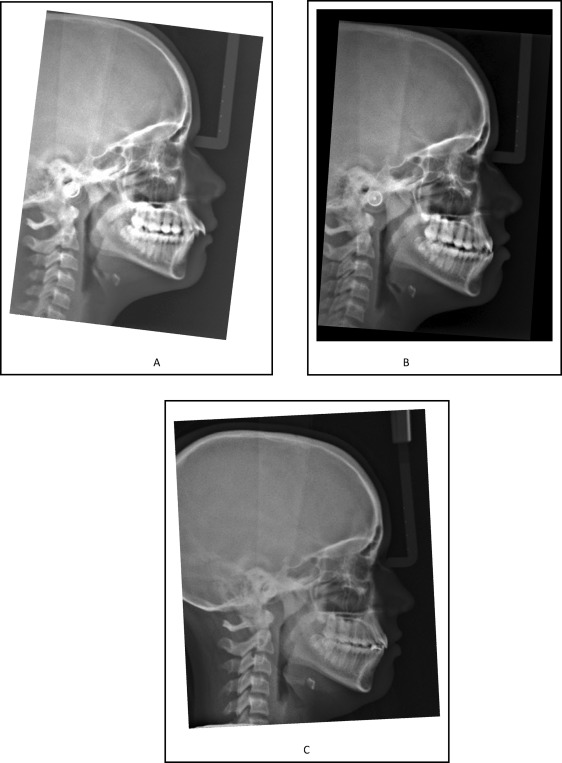
Lateral cephalograms were taken before treatment (T1), immediately after removal of the Herbst appliance (T2), and at completion of fixed appliance therapy (T3). Figure 2 shows the skeletal and dental changes of a typical subject in the study. The radiographs in digital format were uploaded into the software (Dolphin Imaging and Management Solutions, Chatsworth, Calif) and traced digitally to ensure a 1:1 conversion. The lateral cephalometric images were then printed out on a printer (C510; Lexmark International, Lexington, Ky) using photographic paper. The digital lateral cephalometric radiographs for the control subjects were obtained from the Bolton-Brush study and matched closely for age, sex, and craniofacial morphology with the experimental subjects. The images were scanned at 12-bit gray scale resolution with a spatial resolution of 0.1 mm per pixel and stored in uncompressed TIFF format. The images were converted to JPEG format with the IrfanView software (version 4.0; IrfanView, Jajce, Bosnia) and loaded into Photoshop (version 6.0; Adobe Systems, San Jose, Calif) for size analysis. All original radiographs from the Bolton-Brush study were indexed with 4 corner fiduciary points using a template according to the method described by Baumrind and Miller. In Photoshop, the resolutions of the images were verified (600 dpi), and the images were resized to the original dimensions of the unscanned radiographs. Printouts were then made on the C510 printer, and the fiduciary points were measured with an electronic digital caliper to ensure a 1:1 conversion with no distortion from the original radiographs.
Tracings were made on printouts obtained from the digitized cephalograms by an operator (T.T.) using a number 2 HB mechanical lead pencil (0.5 mm; Pentel, Torrance, Calif), an orthodontic protractor, and 0.003-in matte cephalometric acetate tracing film (3M Unitek, Monrovia, Calif). A custom cephalometric analysis was performed using landmarks correlating with the cephalometric systems described by Bjork, Pancherz, VanLaecken et al, and Wigal et al. The data were normalized to account for magnification differences between the cephalometric machine used for the Bolton-Brush study (5.6%) and the cephalometric machine used for the experimental subjects. All linear measurements were made with a digital caliper (accurate to 0.01 mm) and reported to the nearest 0.1 mm. Analyses of the sagittal skeletal and dental changes were recorded along the occlusal plane (OLs) and to the occlusal plane perpendicular (OLp) from the first cephalogram; this formed the reference grid. The grid was then transferred to subsequent cephalograms by superimposing the tracing on the midsagittal cranial structures. The changes in overjet and molar relationships were calculated using the formula in Table II . The measurement for each angular variable was performed with a cephalometric protractor and evaluated to the nearest 0.5°. The measurement for each sagittal and vertical measurement was performed with an electronic digital caliper and evaluated to the nearest 0.01 mm. The caliper was calibrated to 0.0 mm before each measurement. Because lateral cephalograms often show landmarks with right and left images, the midpoint bisecting the 2 images was used.
| Overjet | Molar relationship |
|---|---|
| Skeletal contribution | Skeletal contribution: |
| 1. OLp–A-pt | 1. OLp–A-pt |
| 2. OLp–Pg | 2. OLp–Pg |
| Dental contribution | Dental contribution |
| 3. OLp–A-pt minus Is/OLp | 3. OLp–A-pt minus Is/OLp |
| 4. OLp–Pg minus Ii/OLp | 4. OLp–Pg minus Ii/OLp |
| Overjet correction | Molar relationship correction |
| Sum of 1, 2, 3, and 4 | Sum of 1, 2, 3, and 4 |
Statistical analysis
The starting forms of the control and experimental samples were compared and analyzed using a matched-pairs t test. The skeletal and dental differences between the treatment and control subjects for each variable across the 3 time periods (T1, T2, and T3) were analyzed. A matched-pairs t test was used for each variable to identify treatment effects of the Herbst appliance, growth, and Herbst appliance plus growth (T2-T1, T3-T2, and T3-T1). Matched-pairs t tests were also used to analyze T2-T1 to t2-t1, T3-T2 to t3-t2, and T3-T1 to t3-t1. A level of significance of P <0.05 (95% confidence interval) was used in this study.
The reliability of the cephalometric measurements was tested by investigating the errors in locating, superimposing, and measuring the changes of all landmarks. Ten patients were randomly selected; for both lateral cephalometric images and dental casts, all measurements for all time points (T1, T2, and T3) were made at least 2 weeks after the initial tracing and analyzed to evaluate errors. The intraclass correlation coefficient of reliability ( R ) was used to determine the reliability of cephalometric measurements. The R values ranged from 0 to 1.00, with values greater than 0.90 indicating high reliability. The correlations of all the cephalometric variables ranged from 0.96 to 0.99, with most above 0.98. The errors in sagittal and vertical measurements did not exceed 0.8 mm, and the errors in angular measurements did not exceed 0.5°. The method of cephalometric analysis used in this study was deemed to be reliable and repeatable.
Results
Table III shows the treatment effects with the Herbst appliance for the time period T2 to T1. A total of 18 of 23 variables investigated showed significant differences after 1.5 years of treatment with the Herbst appliance. For the sagittal measurements, no significant change in condylar position was noted. The maxilla moved forward 0.34 mm (Olp–A-pt). The maxillary molars and incisors moved backward 1.46 and 2.02 mm, respectively (Olp-Ms, Olp-Mi). The mandible moved forward 3.7 mm (Olp-Pg). The mandibular molars moved forward 5.5 mm, and the mandibular incisors moved forward 5 mm (Olp-Is, Olp-Ii). For the vertical variables, the maxilla moved downward 2.2 mm (OLs-Apt). Overbite decreased by 3.3 mm. The maxillary molars intruded by 0.8 mm (Msc-NL), and the mandibular molars intruded by 0.6 mm (Mic-ML). The mandibular incisors intruded by 0.9 mm (Ii-ML). For the angular variables, SNA decreased by an average of 0.6°, SNB increased by 4.0°, and ANB decreased by 4.6°. The Wits appraisal decreased by 4.4 mm. The palatal plane (SNL-NL) increased by 2.6°, and the occlusal plane (SNL-OLs) was 2.5° steeper. The maxillary incisors were retracted by 5.5°, and the mandibular incisors were proclined by 8.8°.
| Variable | T2-T1 | T3-T1 | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | P value | Sig | Mean | SD | P value | Sig | |
| Sagittal (mm) | ||||||||
| Olp-Co | 0.34 | 2.14 | 0.3907 | NS | 2.09 | 2.43 | 0.0001 | ‡ |
| Olp-A-pt | 0.34 | 2.35 | 0.0037 | † | 1.87 | 2.87 | 0.1311 | NS |
| Olp-Ms | −1.46 | 2.50 | 0.0032 | † | 0.71 | 3.05 | 0.0437 | ∗ |
| Olp-Mi | 5.53 | 2.58 | 0.0001 | ‡ | 7.0 | 3.45 | 0.0001 | ‡ |
| Olp-ls | −2.02 | 3.64 | 0.0021 | † | −0.39 | 3.84 | 0.5813 | NS |
| Olp-li | 5.04 | 3.75 | 0.0001 | ‡ | 7.2 | 4.47 | 0.0001 | ‡ |
| Olp-Pg | 3.7 | 3.18 | 0.0001 | ‡ | 5.5 | 4.68 | 0.0069 | † |
| Wits | −4.39 | 2.40 | 0.0001 | ‡ | −2.32 | 2.37 | 0.0048 | † |
| Vertical (mm) | ||||||||
| OLs-A-pt | 2.19 | 1.41 | 0.0001 | ‡ | 4.51 | 2.23 | 0.0001 | ‡ |
| ANS-Me | 2.19 | 6.09 | 0.3085 | NS | 4.65 | 3.49 | 0.0001 | ‡ |
| Is-NL | 0.16 | 1.46 | 0.5647 | NS | 0.7 | 2.34 | 0.1152 | NS |
| Ii-ML | −0.87 | 1.59 | 0.0055 | † | 0.71 | 2.17 | 0.0857 | NS |
| Overbite | −3.25 | 1.35 | 0.0001 | ‡ | −3.64 | 1.50 | 0.0001 | ‡ |
| Msc-NL | −0.81 | 1.14 | 0.0014 | † | 0.89 | 1.77 | 0.0026 | † |
| Mic-ML | −0.6 | 1.33 | 0.0022 | † | 1.38 | 1.84 | 0.0001 | ‡ |
| Angular (°) | ||||||||
| SNA | −0.58 | 1.67 | 0.1169 | NS | 0.37 | 2.32 | 0.1479 | NS |
| SNB | 4.03 | 1.61 | 0.0022 | † | 3.15 | 2.09 | 0.0012 | † |
| ANB | −4.61 | 1.68 | 0.0001 | ‡ | −2.78 | 1.61 | 0.0002 | ‡ |
| SNL-NL | 2.55 | 2.61 | 0.0025 | † | 1.6 | 2.87 | 0.0466 | ∗ |
| SNL-ML | −0.56 | 2.29 | 0.1917 | NS | −1.23 | 3.15 | 0.0401 | ∗ |
| SNL-OLs | 4.47 | 2.87 | 0.0001 | ‡ | 1.8 | 3.65 | 0.0026 | † |
| Is/NL | −5.52 | 7.77 | 0.0019 | † | −4.32 | 8.18 | 0.0045 | † |
| Ii/ML | 8.82 | 5.69 | 0.0001 | ‡ | 5.24 | 9.8 | 0.0065 | † |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


