The American Journal of Orthodontics and Dentofacial Orthopedics celebrates its centennial, safeguarded by the nearly 115-year-old American Association of Orthodontists. This journey witnessed the rise and demise of various developments, concepts, and procedures, while basic knowledge is still needed. Various periods can be defined in the past century, but the goals remain to obtain more accurate diagnosis through precise anatomic imaging, more controlled and faster tooth movement, more discreet appliances, and the balance of esthetics, function, and stability. The most recent technologic advances have buttressed these goals. Cone-beam computed tomography has brought 3-dimensional assessment to daily usage, albeit the original enthusiasm is tempered by the risk of additional radiation. Temporary anchorage devices or miniscrews have revolutionized orthodontic practice and loom as a solid cornerstone of orthodontic science. Decortication and microperforation promise to speed up tooth displacement by stimulating vascularization. The concept of the regional acceleratory phenomenon has touched upon even the timing of orthognathic surgery. The burden of esthetic appliances remains, with the demand for “cosmetic” appliances and clear aligners. Have these developments changed the face of orthodontics? Have we engaged in another turn wherein certain treatment modalities may fade, while others join mainstream applications? These questions are addressed in this essay on the challenges, promises, and limitations of current orthodontic technology, enhancement of biologic response, and personalized treatment approaches.
Highlights
- •
Organized orthodontics is nearly 115 years old.
- •
Basic knowledge is still needed.
- •
Unchanged goals are accurate diagnosis, and balance of esthetics, function, and stability.
- •
Controlled, fast tooth movement and discreet appliances are desired.
- •
Changes in orthodontics are also related to developments in dentistry.

Happy centennial anniversary, American Journal of Orthodontics and Dentofacial Orthopedics ( AJO-DO ), the American journal of worldwide orthodontics. You have been the meeting place of minds across the universe of orthodontists and their prime reference. A reverend salute to a mission accomplished with dedicated editors, writers, and thousands of unknown soldiers, along with millions of smiles.
An anniversary is an intersection of memory and outlook, with their loads of meditation and inspiration: what have we achieved, and where are we going? At some level, it holds in its folds the grains of a tabula rasa (clean slate) to invite rejuvenation. This centennial invites contemplation of a rich heritage and a projection of destination.
The anatomy of a century
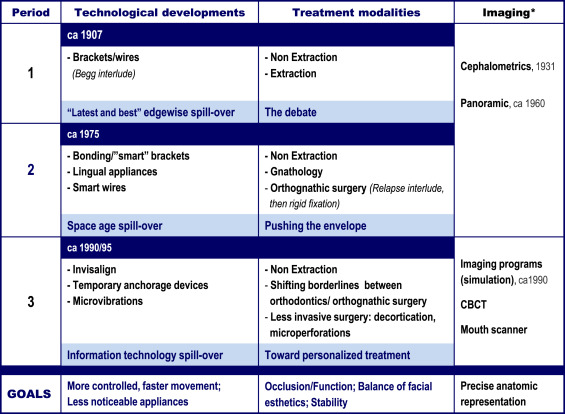
Three periods may be defined in the past orthodontic century, based on 2 major panels—technologic developments and treatment modalities—both with obvious correspondence in the respective temporal periods ( Fig 1 ). Imaging represents a parallel theme that deserves distinction, albeit defined in technology.
The first period: edgewise spill-over
Bracketed between the turn of the 20th century until the 1970s, this long phase was dominated by Edward Angle’s technologic breakthrough with the edgewise bracket, except for the Begg bracket/technique “interlude,” which in essence was more an extraction treatment mode. Thus, the period can be entitled the “latest and best” edgewise spill-over, in reference to Angle’s famous quote regarding the edgewise bracket: “the latest and the best; use it.”
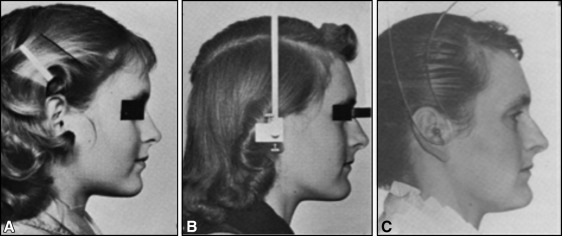
Originally embraced by Angle’s nonextraction approach to achieve Class I occlusion, maintenance of the full dentition at the expense of stability or esthetics was tested after Angle’s death (1930) by one of his students, Charles Tweed, who reintroduced tooth extraction in the United States, and later in Australia by another student, Raymond Begg. Tweed’s retreatment of patients with the extraction of 4 first premolars influenced American orthodontists to do more extractions (nearly half of orthodontic treatments in the 1960s). The rationale was that discrepancies between tooth and jaw sizes were genetically determined. The extraction pendulum swung too far, affecting facial esthetics toward a “dished-in” profile or an “extraction look” ( Fig 2 ). The debate on extraction or nonextraction reached far into the minds and skills of orthodontists to a point where lines were drawn between extractionists and nonextractionists.
Accompanying these developments were key radiographic innovations. Cephalometry (1931) at a minimum supported the clinical findings but also elevated them to more comprehensive diagnosis, justification for treatment planning, and evaluation of treatment outcome. Later, panoramic radiography (about 1960) considerably facilitated assessment and became the trademark record to evaluate perfection in treatment through root parallelism.
The second period: space-age spill-over
This period was shorter than the first, probably because, in the first period, World War II interrupted the flow of developments in science and technology, which picked up speed exponentially in the last quarter of the 20th century, if only gauged by the arrival of the personal computer in offices and homes.
The mid-1970s ushered in a series of technologic developments that mark orthodontics to this day. The introduction of the straight-wire method with prescription brackets, along with the 6 keys of normal occlusion by Andrews, had an initial impact of “dialing a treatment” that was tempered with daily practice. But the introduction of the “smart wires” made possible by a by-product of space exploration, the nickel-titanium alloy wire, stole the show, warranting the nickname of this second period as “space-age spill-over.” The promises with such developments were gentler tooth movement and more comfort for the patient. The latter was yet to be served by the incoming lingual braces. These unseen appliances, as well as ceramic brackets, provided answers to the demand for less noticeable and thus more esthetic appliances.
The practitioner was provided with faster, more practical techniques (eg, bonding replaced or complemented banding, and elastomeric attachments with color-on-demand supplanted the more time-consuming ligatures). Self-ligating brackets were introduced in this era and expanded in the next, with the premise of better controlled mechanics, greater patient comfort, and improved practice management. However, their use remained more limited than the still thriving “regular” brackets, probably owing to mixed research outcomes, cost, and operator variables.
On the treatment front, physics was formally injected into the science of tooth movement, thanks to the leading works of Burstone, who with coworkers also carried the clinically applicable concepts to wire architecture (beta-titanium alloy wire). While gnathologic concepts were permeating dentistry, Roth championed their application in orthodontics. Expanding from the dentition to understand and “treat” the associated structures (musculature, temporomandibular joint, and healthy periodontium), the age of the total occlusion—thus, interactive multidisciplinary treatment—was at the door, increasingly encompassing the treatment of adults rather than mostly children. Finally, the triple crown of function, esthetics, and stability helped push the envelope of orthognathic surgery beyond the seminal works of Harvard’s Kazanjian (1879-1974), France’s Tessier (1917-2008), and the University of Zurich’s Obwegeser (1920-), when leading American surgeons modified and diversified the original surgical methods through critical research. The earlier problems of treatment relapse were addressed with the onset of rigid fixation.
Underlying all those developments was the clear statement that orthodontics was dedicated not only to occlusal morphology and associated functions, but also at least equally to facial esthetics. By the 1990s, the trend to extraction had reversed to nonextraction but emphasized esthetics and stability and thus distalization mechanics, rather than proclination of anterior teeth. Yet, transverse expansion emerged, also reinforced by “smile esthetics” to reduce the black corridors between the posterior teeth and the corners of the mouth, and provide “consonance” of the lower lip and the maxillary anterior teeth curvatures. If any negative perception was held regarding orthodontics yielding an “extraction look” or a “dished-in” face, the American Association of Orthodontists campaigns featuring Miss America dispelled the stigma ( Fig 3 ). These efforts were buttressed when the AJO-DO not only served as a vehicle reflecting through scientific publications the paradigm shifts worldwide, but also featured on its cover the “smile” label and, later, the smiles of actual patients every month.

Orthodontics was at a new platform, ready for a new slate of developments at the eve of the 21st century, having crossed the 20th century under Edward Angle’s shadow; kept pace with technologic developments (from imaging to high tech); engaged in research with increasing adherence to scientific rigor (eg, a series of randomized prospective clinical trials generated by the National Institutes of Health in the late 1980s and 1990s ); accomplished excellent organization in its institutions (academia and associations); and built partnerships for scientific discovery between universities and associations (eg, through the American Association of Orthodontists Foundation and its Planning and Awards Review Committee [PARC] ), among universities (Graduate Orthodontic Residents Program experience), and among universities, associations, and industry.
Yet in education, the century closed on a critical issue felt into the next period: while the benefits of technology entered the university classroom, the full-time academician became an “endangered species.” Recruiting and retaining junior faculty faltered for various reasons: lack of competitive salary with private practice; unsatisfactory university environment, including failure in departmental and school administrative leadership and even political influences; lack of or insufficient mentoring and protected time for professional development; work overload; unrealistic criteria for promotion; and lack of “qualifications and ambition for an academic career.” Articles in the AJO-DO and other American orthodontic journals reflect the academic retention problem: increasingly more research articles were from international non-American institutions, albeit this development also echoed a healthy scientific globalization.
The third period: information technology spill-over
The present third period picked up on 4 intersecting tracks: esthetic means of treatment delivery, faster treatment, improved anchorage, and more precise imaging (diagnosis and treatment simulation). Technologic developments may be classified under information technology spill-over, while treatment has solidly moved, along with all areas of medicine, toward personalized delivery.
Three main technologic headlines emerged in this period.
Temporary anchorage devices
“The latest and best in anchorage control,” orthodontic miniscrews, also known as mini-implants and (nonosseointegrated) temporary anchorage devices, may be viewed as the revolution of the orthodontic century, “the holy grail of orthodontics,” a solution to both compliance and controlled anchorage. A rush-hour melée about types, heads, widths, and lengths of screws was followed by corresponding research before more order set in regarding dimensions, properties, and indications. The pierced metal devices succeeded thanks to the biologic tolerance of bone and the surrounding soft tissues, where the story of tooth movement truly unfolds. This solid success has led to the use of mini-implants at younger ages in the permanent dentition because their insertion in the mixed dentition is hazardous to unerupted permanent teeth. In this perspective, an important question arises, warranting research for answers: would the distalization of the maxillary arch against implants generate the orthopedic differential growth between the jaws similar to that engendered by headgear in the correction of Class II malocclusion?
Esthetic appliances
Operator difficulties and cost, if not compromised results, prevented a wider application of various modes of lingual appliances, now stratified into 2-dimensional and 3-dimensional (3D) modes. On the other hand, clear aligners augured an esthetic revolution. The concert of various computing, imaging, milling, and robotic technologies brought about a variety of aligners, known popularly by the brand that eventually became the generic household name Invisalign (Align Technology, San Jose, Calif). Research has disclosed limitations in success and compromised excellence in more complicated malocclusions: the aligner alone does not seem adequate to achieve high-quality results but, rather, requires multiple adjunctive approaches for various clinical situations. Accordingly, case selection and awareness of limitations are critical to the operator, who must amass experience and competence after an initial learning curve, and use proper sequencing of movements to reduce the need for case refinement.
Imaging methods
Diagnosis and treatment planning were enhanced by 3D imaging (cone-beam computed tomography [CBCT]), outcome simulation, and mouth scanners. Computed tomography became user-friendly in orthodontics and implant dentistry by the advent of CBCT, but the risks of additional radiation prompted the recommendation of a commissioned panel by the American Academy of Oral and Maxillofacial Radiology against its routine use. Accordingly, until it can be provided with less radiation, CBCT should be used when it supports better diagnosis and treatment; it is a perfect tool in various situations (eg, impacted canines). Journal editors and peer reviewers are sensitized to the issue and request clear institutional review board statements to prevent abuse, possible deception, and questionable statements in the literature. CBCT also has not on average provided growth and outcome data with major differences from 2-dimensional cephalometric findings.
Outcome simulation, particularly helpful in orthognathic surgery, was further enhanced by the CBCT-provided 3D application. Although existing programs already provided a practical guideline for daily practice, prediction of treatment outcome has yet to become more precise, pending the generation of more data accounting for the vast individual variations. Soft tissue assessment has not reached routine evaluation comparable to that of hard tissues (bone and teeth) in most studies of treatment outcomes. A greater volume of such assessments is needed for the development of algorithms with more accurate applications.
Mouth scanners are on the scene to replace dental casts in at least basic functions, also providing the benefits of better appreciation of soft tissue characteristics and 3D manipulation, space analysis, and dental simulations. The American Board of Orthodontics and other examining bodies (Angle Society) already allow the use of scanned models, which are expected to prevail with further developments and wider adherence by educational programs and practitioners.
Treatment approaches of the ongoing third period maintain an anchor in esthetics and the smile and they increase, albeit slowly, reliance on biologic principles and individual variations, moving away from the more mechanistic modes.
Nonextraction treatment
The pendulum stays swung toward nonextraction, with the dished-in (half-moon) extraction profile replaced by a fuller profile, most likely representing cultural trends of beauty preferences. The possibility of extractions without profile flattening remains, but the extraction (including early removal) of third molars still does not figure in the statistics of extraction.
Techniques for faster treatment: decortication (Wilckodontics and microperforations) and microvibrations
“Accelerated osteogenic orthodontics” through interproximal surgical cortical cuts (decortication) is but another application of the regional acceleratory phenomenon, yielding faster results than regular similar treatment, regardless of agreement with the treatment plan, the perfection of finishing, or the possibility of periodontal recession. Adjunct microperforation was presented as a viable alternative to forego the “aggressiveness” of decortications, aiming at generating inflammation-enhanced tooth movement. Initial animal and human studies demonstrated the potential of the method to promote faster movement, but several questions remain regarding the frequency of microperforations (how often should they be repeated) and the number of microperforations (how many times should they be repeated and should the rate be variable in different patients). At a practical level, commercial microperforation kits are available allowing the orthodontist to “dial” the depth of microperforation (eg, 2-3 mm). This method can also be applied through the repeated insertion and withdrawal of orthodontic miniscrews ( Fig 4 ).





