INTRODUCTION
COMPOSITION OF COMPOSITES
• Organic Matrix
• Fillers
• Coupling Agent
• Coloring Agents
LIV Absorbers
• Initiator Agents
• Inhibitors
CLASSIFICATION OF COMPOSITES
TYPES OF COMPOSITE RESINS
• Macrofilled Composite Resins
• Microfilled Composite Resins
• Hybrid Composite Resins
RECENT ADVANCES IN COMPOSITES
• Flowable Composite Resins
• Condensable (Packable) Composites
• Giouiers
• Compomers (Polyacid Modified Composite Resins)
• ORMOCER (Organically Modified Ceramic)
• Antibacterial Composites/Ion Releasing Composites
• “Smart” Composites
PROPERTIES OF COMPOSITE RESTORATIVE MATERIALS
• Coefficient of Thermal Expansion
• Water Absorption
• Wear Resistance
• Surface Texture
• Radiopacity
• Modulus of Elasticity
• Solubility
• Creep
• Polymerization Shrinkage
• Configuration or “C-factor”
• Esthetics of Composites
• Microleakage and Nanoleakage
• Biocompatibility
• Working and Setting Times
POLYMERIZATION OF COMPOSITES
• Curing Time
• Shade of Composite
• Distance and Angle between Light Source and Resin
• Temperature
• Resin Thickness
• Inhibition of Air
• Intensity of Curing Light
• Type of Filler
INDICATIONS OF COMPOSITE RESTORATIONS
CONTRAINDICATIONS OF COMPOSITES
ADVANTAGES OF COMPOSITES
DISADVANTAGES OF COMPOSITES
TOOTH PREPARATION FOR COMPOSITE RESTORATIONS
CLASS III TOOTH PREPARATION
• Conventional Class III Tooth Preparation
• Beveled Conventional Class III Tooth Preparation
• Modified (Conservative) Class III Tooth Preparation
CLASS V TOOTH PREPARATION
• Conventional Class V Preparation
• Beveled Conventional Class V Tooth Preparation
• Modified (Conservative) Class V Tooth Preparation
RESTORATIVE TECHNIQUE FOR COMPOSITES
• Pulp Protection
• Etching of the Tooth Preparation
• Application of Adhesive System
• Matrix Application
• Composite Placement
• Final Contouring, Finishing and Polishing of Composite Restoration
• Checking the Occlusion
• Glazing
FAILURES IN COMPOSITE RESTORATIONS
INTRODUCTION
The modern history of tooth colored restorative materials was started with silicate cement which was introduced by Fletcher in the year 1878 in England, which was further encouraged by Steenback and Ashor in 1903. Silicate cements were discouraged later on because of their poor strength, irritation to pulp tissue and brittleness. Moreover tooth preparations for silicate cement need to be of the conventional type.
Self-curing acrylic resins were developed in 1930 in Germany, but they became popular in dentistry in late 1940s. They were used as veneers on the facial surface of metal restorations and as facings in crowns and bridges. But they too showed poor physical properties like high polymerization, shrinkage and coefficient of thermal expansion (CTE), lack of wear resistance, poor marginal seal, irritation to pulp and dimensional instability.
In an attempt to improve their properties, R Bowen, in 1962, developed a polymeric dental restorative material reinforced with silica particles used as fillers. These materials were called `composites’. Thus we can say that composite resins have been introduced in operative dentistry to overcome the drawbacks of the acrylic resins that replaced silicate cements in the 1940s. Over the past two decades, there has been a substantial progress in the development and application of resin-based composites. Earlier composites were recommended only as a restorative material for anterior restorations, but now they have become one of the most commonly used direct restorative materials for both anterior and posterior teeth. This is because of better understanding of their application methods, including composite placement and curing and improvement of their physical and mechanical properties. The principal reasons for the shifting from dental amalgam to composites are the reduced need for preparation and the strengthening effect on the remaining tooth. Roeters et al have said once that the introduction of resin composites is not just a change in materials and techniques but also a change in treatment philosophy. Nowadays, composite resins are considered as an economical and aesthetic alternative to other direct and indirect restorative materials. They can be used in different clinical conditions like diastema closures, veneers for anterior teeth and restorations for Class I, II, III, IV and V conservative restorations. If properly manipulated, they can prove the success rate and longevity equal to those of other materials. Since composite do not have self-adhering property, an adhesive is required before their placement. Placement of a composite resin is very technique-sensitive than the placement of other restorations.
By definition, a composite is a compound composed of atleast two different materials with properties which are superior or intermediate to those of an individual component.
Dental composite resins have two primary components which are matrix phase and the filler phase and many secondary components like polymerization initiators, pigments for providing different shades and silane coupling agents. Though secondary components are required for every composite material, most of the properties of material are dependent upon filler and matrix phases.
Although different composite materials have specific composition and distribution of the matrix and filler particles, they are often composed of bisphenol-A-diglycidyl- methacrylate (Bis-GMA) or urethane di-methacrylate (UDMA) matrix polymers and glass filler particles. Both the amount and the size of the filler particles determine mechanical properties of different composites.
History of composite resins (From 1901 to 2007)
1901 Synthesis and polymerization of methyl methacrylate
1930 Use of PMMA as denture base resin
1944 First acrylic filling material
1951 Addition of inorganic fillers to direct filling materials
1955 Acidetch technique introduced by Buonocore
1956Bowen investigated dimethacrylates (Bis-GMA) and silanized inorganic filler
1962 Introduction of silane coupling agents
1964 Marketing of Bis-GMA composites
1968 Development of polymeric coatings on fillers
1973 UV-cured dimethacrylate composite resins
1976 Introduction of microfilled composites
1977 Visible light cured dimethacrylate composite resins
1996 Development of flowable composites
1997 Development of packable composites
1998 Development of fiber reinforced, ion releasing composites and ormocers.
COMPOSITION OF COMPOSITES
Composites are basically modified methacrylates or acrylates with other ingredients to produce different structures and properties. The methacrylates are used because of their refractive index of 1.3 which is close to tooth. This allows metamerism (chameleon effect) giving the effect of similarity since methacrylates shrinks, inorganic inert filler particles of similar refractive index are added.
In general, dental composites are composed of following materials (Fig. 11.1):
• Organic matrix or organic phase
• Inorganic matrix
• Filler or disperse phase
0 An organosilane or coupling agent
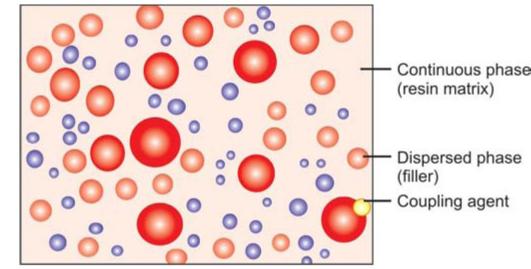
Fig. 11.1: Composition of composite resin
• Activator-initiator system
• Inhibitors
• Coloring agents.
Composition of composites
Organic resins
• Bis-GMA (Bowen’s resin)
• Dipentaerythritol pentaacrylate monophosphate
• Urethane dimethacrylate
• Urethane tetramethacrylate
• Hexamethylenediisocyanate
Fillers
• Fused or crystalline quartz
• Silicon dioxide
• Borosilicate/Lithium aluminosilicate glass
• Ceramics
• Ytterbium trifluoride
• Radiopaque silicates
• Organically modified ceramics (ORMOCERS)
Others
• Triethyleneglycol dimethacrylate (TEGDMA)
• HEMA
• Camphorquinone (CQ)
• META; phosphorated esters
• Silane coupling agents
• Antibacterial monomers
• Benzoyl peroxide and amine activator
Organic Matrix
The matrix base consists of polymeric mono-, di- or trifunctional monomers like Bis-GMA or UDMA. The monomer system represents as the backbone of the composite resin system. Most preferred monomer is Bis-GMA either alone or in conjunction with urethane dimethacrylate UDMA. Since this resin is very viscous, in order to improve clinical handling, it is diluted with low viscosity monomers to control the viscosity. These can be bisphenol A dimethacrylate (Bis-DMA), ethylene glycol dimethacrylate (EGDMA), triethylene glycol dimethacrylate (TEGDMA), methyl methacrylate (MMA). Bis-GMA and
TEGDMA have been tried in the ratio of 1:1 and 3:1, latter is preferred because an increase in TEGDMA increases the chances of polymerization shrinkage.
Fillers
The dispersed phase of composite resins is made up of an inorganic filler material. Since filler particles are added to improve the physical and mechanical properties of the organic matrix, the basic aim is always to incorporate high percentage of filler. Commonly used fillers are silicon dioxide, boron silicates and lithium aluminium silicates. The filler particles are silanated so that the hydrophilic filler can bond to the hydrophobic resin matrix. The wear of composite restorations depends on filler particle size, interparticle spacing and filler loading. Composites with smaller particles show decreased wear due to fewer voids and smaller interparticle spacing.
Addition of filler causes following effects
• Reduces the thermal expansion coefficient
• Reduces polymerization shrinkage
• Increases abrasion resistance
• Decreases water sorption
• Increases tensile and compressive strengths
• Increases fracture toughness
• Increases flexure modulus
• Provides radiopacity
• Improves handling properties
• Increases translucency
In some composites, the quartz is partly replaced with heavy metal particles like zinc, aluminium, barium, strontium or zirconium. Nowadays calcium metaphosphate has also been tried. Since these are less hard than glass, they cause less wear on the opposing tooth.
Recently nanoparticles having the size of 25 nm and nanoaggregates of 75 nm, made up of zirconium/silica or nanosilica particles have also been introduced. The smaller size of filler particles results in better finish to the restoration.
Coupling Agent
Interfacial bonding between the matrix phase and the filler phase is provided by coating the filler particles with silane coupling agents. In other words a coupling agent is used to bond the filler to the organic resin. This agent is a molecule with silane groups at one end (ion bond to Si02) and methacrylate groups at the other.
Functions of Coupling Agents
• Bonding of filler and resin matrix.
• Transfer forces from flexible resin matrix to stiffer filler particles.
• Prevent penetration of water along filler resin interface, thus provide hydrolytic stability.
Examples Organic silane
Coloring Agents
Coloring agents are used in very small percentage to produce different shades of composites. Mostly metal oxides such as titanium oxide and aluminium oxides are added to improve the opacity of composite resins.
UV Absorbers
They are added to prevent discoloration, in other words they act like a “sunscreen” to composites. Commonly used UV absorber is Benzophenone.
Initiator Agents
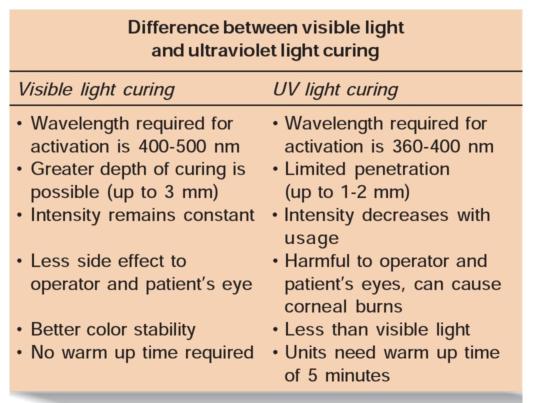
These agents activate the polymerization of composites. Most common photoinitiator used is camphoroquinone. Currently most recent composites are polymerized by exposure to visible light in the range of 410-500 nm.
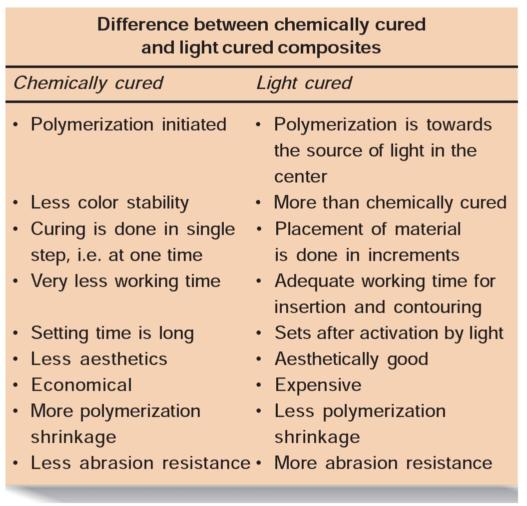
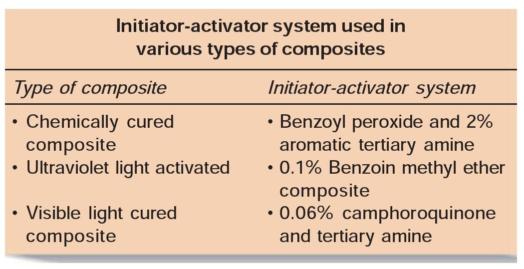
Initiator varies with type of composites whether it is light cured or chemically cured.
Inhibitors
These agents inhibit the free radical generated by spontaneous polymerization of the monomers. For example, Butylated hydroxyl toluene (0.01%).
CLASSIFICATION OF COMPOSITES
Composite resins can be classified by filler size and % filler loading and by the viscosity of the composite. With the expanded categories of composite resins, they can also be classified by their uses.
Composite resins have been classified in different ways:
1. According to Skinner:
a. Traditional or conventional composite-8-12 pm
b. Small particle filled composites-1-5 pm
c. Microfilled composites-0.4-0.9 pm
d. Hybrid composites-0.6-1 pm
2. Philips and Lutz classification according to filler particle size:
a. Macrofiller composites (particles from 0.1-100 p)
b. Microfiller composites (0.04 p particles)
c. Hybrid composites (fillers of different sizes).
3. According to the mean particles size ofthe major fillers:
a. Traditional composite resins
b. Hybrid composite resins
c. Homogeneous microfilled composites-if the composite simply consists of fillers and uncured matrix material, it is classified as homogeneous
d. Heterogeneous microfilled composites-if it includes procured composites and other unusual filler, it is called heterogeneous.
4. Classification according to Bayne and Heyman:
5. Classification according to matrix compositions:
a. Bis-GMA
b. UDMA
6. Classification according to polymerization method
a. Self-curing
b. Ultraviolet light curing
c. Visible light curing
d. Dual curing
e. Staged curing.
TYPES OF COMPOSITE RESINS
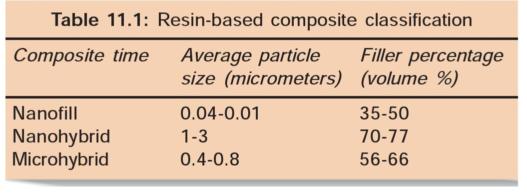
Though composites have been classified according to different characteristics, the most commonly followed classification is based on the type, distribution and filler phase of composites (Table 11.1).
Composite resin can be divided into three types based on the size, amount and composition of the inorganic filler (Figs 11.2A to C):
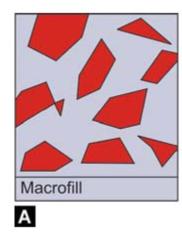
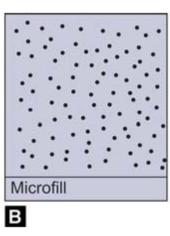
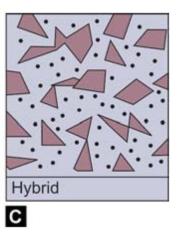
Figs 11.2A to C: Diagrammatic representation of different composites
1. Macrofilled composite resins
2. Microfilled resins
3. Hybrid composite resins.
Macrofilled Composite Resins
Average particle size of macrofill composite resins is from 5-25 micron. Filler content is approximately 75-80% by weight.
It exhibits a rough surface texture because of the relatively large size and extreme hardness of the filler particles. The surface becomes more rough as the resin matrix being less hard, wears at faster rate.
Due to roughness, discoloration and wearing of occlusal contact areas and plaque accumulation take place quickly than other types of composites.
Advantage of Conventional Composite
• Physical and mechanical performance is better than unfilled acrylic resins.
Disadvantages
• Rough surface finish
• Poor polishability
• More wear
• More prone to staining.
Microfilled Composite Resins
Microfilled composites were introduced in the early 1980s. Average particle size of microfilled resins ranges from 0.04-0.1 micrometer. Filler content of microfilled resins is 35-50% by weight. The small particle size results in smooth polished surface which is resistant to plaque, debris and stains.
But because of less filler content, some of their physical properties are inferior. They have low modulus of elasticity and high polishability, excellent translucency. However, they exhibit low fracture toughness and increased marginal breakdown.
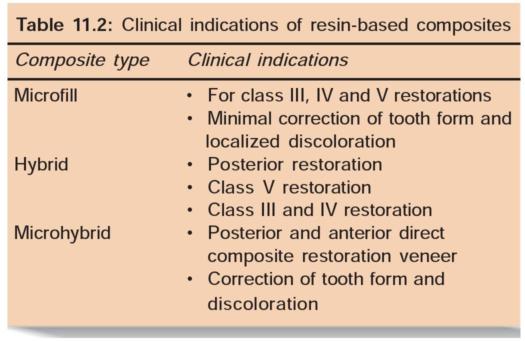
They are indicated for the restoration of anterior teeth and cervical abfraction lesions (Table 17.2).
Advantages
• Highly polishable
• Good esthetic.
Disadvantages
• Poor mechanical properties due to more matrix content
• Poor color stability
• Low wear resistance.
• Less modulus of elasticity and tensile strength
0 More water absorption
• High coefficient of thermal expansion
Hybrid Composite Resins
In order to combine the advantages of conventional and microfilled composites, hybrid composites were developed.
Hybrid composites are named so because they are made up of polymer groups (organic phase) reinforced by an inorganic phase. Hybrid composites are composed of glasses of different compositions and sizes, with particle size diameter of less than 2 pm and containing 0.04 pm sized fumed silica. Filler content in these composites is 75-80% by volume. This mixture of fillers is responsible for their physical properties similar to those of conventional composites with the advantage of smooth surface texture.
Advantages of Hybrid Composites
• Availability in various colors
• Different degrees of opaqueness and translucency in different tones and fluorescence
• Excellent polishing and texturing properties
• Good abrasion and wear resistance
• Similar coefficient of thermal expansion
• Ability to imitate the tooth structure
• Decreased polymerization shrinkage
• Less water absorption.
Disadvantages of Hybrid Composites
• Not appropriate for heavy stress-bearing areas.
• Not highly polishable as microfilled because of presence of larger filler particles in between smaller ones.
• Loss of gloss occurs when exposed to toothbrushing with abrasive toothpaste.
Two new generations ofhybrid composite resins are:
1. Nanofill and nanohybrids
2. Microhybrids.
1. Nanofill and nanohybrid composites: Nanofill and nanohybrid composites have average particle size less than that of microfilled composites.
The introduction of these extremely small fillers and their proper arrangement within the matrix results in physical properties equivalent to the original hybrid composite resins.
Advantages
• Highly polishable
• Tooth-like translucency with excellent aesthetic
• Optimal mechanical properties
• Good handling characteristics.
• Good color stability
• Stain resistance
• High wear resistance
• Can be used for both anterior and posterior restorations and for splinting teeth with fiber ribbons.
2. Microhybrid composites: Microhybrid composites have evolved from traditional hybrid composites.
Filler content in microhybrids are 56 to 66% by volume. The average particle size in these composites range from 0.4-0.8 pm.
Incorporation of smaller particles makes them better to polish and handle than their hybrid counterparts. Because of presence of large filler content, microhybrid composites have improved physical properties and wear resistance than microfilled composites.
Advantages
• Better polish and surface finish
• Easy handling
• Improved physical properties
• Good wear resistance.
RECENT ADVANCES IN COMPOSITES
• Flowable composite resins
• Condensable (packable) composites
• Giomers
• Compomers
• Ormocers
• Antibacterial/ion releasing composites
• “Smart” composites
Flowable Composite Resins
They were introduced in the dentistry in late 1996. These resins have lower filler content ranging from 41-53% by volume. Low filler loading is responsible for decreased viscosity of composites, which allows them to be injected into both preparation, this makes them a good choice as a pit and fissure restorative.
They have an average particle size ranging from 0.04-1 pm. Their decreased viscosity is achieved by reducing the filler volume.
Type
Filler content in flowable resins is 60% by weight. It is usually silica which are 0.02 to 0.05 pm in size. Lower filler content is responsible for poor mechanical properties of these composites than conventional composites.
Advantages
• Low viscosity
• Improve marginal adaptation of posterior composites by acting as an elastic, stress absorbing layer over which composite is placed
• High wettability of the tooth surface
• High depth of cure
• Penetration into every irregularity of preparation
• Ability to form layers of minimum thickness, thus eliminate air entrapment
• High flexibility, so less likely to be displaced in stress concentration areas
• Radiopaque
• Availability in different colors
• Require minimally invasive tooth preparations
• For the pediatric patient to be used in narrow and deep pits and fissures.
Disadvantages
• More susceptible to wear in stress-bearing areas
• Weaker mechanical properties
• More polymerization shrinkage and wear
• Sticks to the instrument, so difficult to smoothen the surface.
Indications
• Preventive resin restorations
• Small pit and fissure sealants
• Small, angular class V lesions
• For repairing ditched amalgam margins
0 Repair of small porcelain fractures
• Inner layer for class II posterior composite resin placement for sealing the gingival margin
• Resurfacing of worn composite or glass ionomer cement restorations
• For repair of enamel defects
• For repair of crown margins
• Repair of composite resin margins
• For luting porcelain and composite resin veneers
• Class I restorations
• Small class III restorations
• As base or liner
• Tunnel restorations.
Condensable (Packable) Composites
Condensable composites have been developed in an attempt to improve the compressive, tensile and edge strength and handling of the composite. The principle of the high viscosity of packable composites is that they can be pushed into the posterior tooth preparation and have greater control over the proximal contour of class II preparations. Their basis is polymer rigid inorganic matrix material (PRIMM). In this components are resin and ceramic inorganic fillers which are incorporated in silanated network of ceramic fibers. These fibers are composed of alumina and silicon dioxide which are fused with each other at specific sites to form a continuous network of small compartments. Filler content in packable composites ranges from 48-65% by volume. Average particle size ranges from 0.7-20 pm.
Packable composites possess improved mechanical properties because of presence of ceramic fibers. They have improved handling properties because of presence of higher percentage of irregular or porous filler, fibrous filler and resin matrix. The consistency of the condensable composites is like freshly triturated amalgam. Each increment can be condensed similar to amalgam restoration and can be cured to a depth of over 4 mm.
Indications
• Indicated for stress-bearing areas
• In class II restorations as they allow easier establishment of physiological contact points.
Advantages
• Increased wear resistance because of presence of ceramic fibers
• Condensability like silver amalgam restoration
• Greater ease in achieving a good contact point
• Produce better reproduction of occlusal anatomy
• Deeper depth of cure because of light conducting properties of individual ceramic fibers
• High flexural modulus
• Decreased polymerization shrinkage because of presence of ceramic fibers
• Reduced stickiness
• Physical and mechanical performance is similar to that of silver amalgam.
Disadvantages
• Difficulties in adaptation between one composite layer and another
• Difficult handling
• Poor aesthetics in anterior teeth.
Giomers
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


