Nonextraction camouflage treatment along with Class III elastics was used to treat a 39-year-old woman with a skeletal Class III pattern and a low mandibular plane angle and short lower anterior facial height. The total active treatment time was 26 months. Her occlusion, smile esthetics, and soft tissue profile were significantly improved after treatment.
Highlights
- •
A surgical patient was treated nonsurgically.
- •
The patient was in braces for only 26 months.
- •
Occlusion, smile esthetics, and soft tissue profile were significantly improved (ABO cast radiograph evaluation score, 14).
Skeletal Class III malocclusions are some of the most complex cases to treat. Currently, orthognathic surgery and orthodontic camouflage are the standard techniques for treating this condition in fully grown patients. Although the surgical approach is aimed at improving their facial esthetics and correcting their skeletal and dental discrepancies, the surgical correction might not result in enough change in the facial profile of borderline patients. Camouflage treatment may not give the desired outcome, either.
With skeletal Class III patients, orthodontic camouflage can be used to treat milder cases with Class III elastics, but it is limited to patients with a low mandibular plane angle and a deepbite. This method is therefore unacceptable for most Class III patients who have high mandibular plane angles and increased lower anterior face heights. Class III elastics extrude the maxillary molars and cause clockwise mandibular rotation that results in increased lower anterior face height. Furthermore, Class III elastics exacerbate the already proclined maxillary anterior teeth, compromising both esthetics and overall stability of treatment. Even so, when the patient declines orthognathic surgery or when temporary skeletal anchorage devices are used to prevent the extrusion of the maxillary molars and the proclination of the maxillary dentition, camouflage treatment with Class III elastics is a valid option.
This case report presents the use of camouflage treatment and Class III elastics to correct a skeletal Class III malocclusion with crossbites. Clinically acceptable and esthetically pleasing treatment results were achieved.
Diagnosis and etiology
A 39-year-old Hispanic woman was referred for an evaluation of orthodontic treatment. Her chief complaints were underbite and crowding. She had a mesofacial, symmetrical face and a concave profile with a strong chin projection ( Fig 1 ). Clicking sounds were heard in the temporomandibular joint during the evaluation, but she did not have any symptoms such as pain, restricted jaw movement, joint noise, or other symptoms.

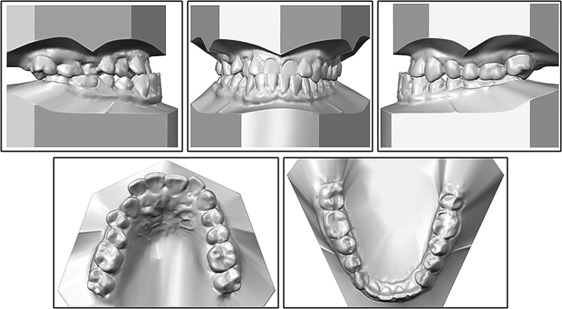
Intraorally, she had anterior crossbites on the maxillary central incisors, maxillary right lateral incisor, and maxillary right canine, and posterior crossbites on the maxillary right second premolar and first molar. She also had incisal attrition on the maxillary central incisors from occlusal trauma and significant restorations on the posterior teeth. She had a −3-mm overjet and a 2-mm overbite of her maxillary central incisors. She had end-on Class III molar relationships on both sides. The maxillary arch showed moderate crowding, and the mandibular arch showed mild crowding with a flat curve of Spee. Her maxillary dental midline was coincident with her facial midline, and her mandibular dental midline was deviated 1 mm to the right. When her mandible was guided into centric relation, a functional shift was detected because of the anterior and posterior crossbites ( Figs 1 and 2 ).
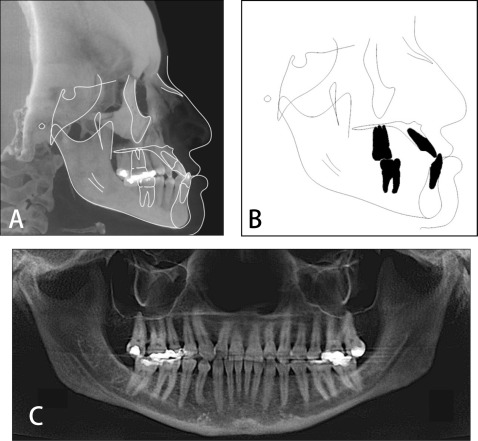
A panoramic radiograph showed several restorations on her posterior teeth, and all third molars had been extracted ( Fig 3 ). The lateral cephalometric analysis indicated a skeletal Class III pattern (ANB, −2.4°; Wits appraisal, −7.9 mm) with a hypodivergent growth pattern (SN-MP, 24.8°). The maxillary incisors were proclined (U1-SN, 121.0°), and the mandibular incisors were retroclined (IMPA, 85.8°) ( Fig 3 ; Table ). Her father also had a skeletal Class III pattern, so the etiology of her Class III malocclusion appeared to be a combination of heredity and environmental factors. Her American Board of Orthodontics Discrepancy Index score was 33 ( Supplementary material ).
| Measurement | Norm | Pretreatment | Posttreatment |
|---|---|---|---|
| SNA (°) | 82.0 | 87.5 | 88.8 |
| SNB (°) | 80.0 | 89.9 | 88.3 |
| ANB (°) | 2.0 | −2.4 | 0.5 |
| Wits appraisal (mm) | −1.0 | −7.9 | −3.9 |
| SN-MP (°) | 32.0 | 24.8 | 26.7 |
| FH-MP (°) | 24.0 | 21.6 | 23.4 |
| LFH (ANS-Me/N-Me) (%) | 55.0 | 50.8 | 52.2 |
| U1-SN (°) | 104.0 | 121.0 | 121.8 |
| U1-NA (mm) | 4.0 | 6.2 | 7.1 |
| IMPA (°) | 90.0 | 85.8 | 80.6 |
| L1-NB (mm) | 4.0 | 6.0 | 5.1 |
| U1/L1 (°) | 131.0 | 121.4 | 124.0 |
| Upper lip to E-plane (mm) | −4.0 | −6.2 | −4.4 |
| Lower lip to E-plane (mm) | −2.0 | 0.6 | −0.9 |
Treatment objectives
The following treatment objectives were established: (1) reduce facial concavity, (2) correct anterior and posterior crossbites, (3) eliminate the functional shift and correct the dental midline, (4) establish Class I molar relationships, (5) obtain normal overjet and overbite, (6) relieve crowding, (7) obtain a stable occlusal relationship, and (8) improve facial and dental esthetics by establishing an esthetic smile.
Treatment objectives
The following treatment objectives were established: (1) reduce facial concavity, (2) correct anterior and posterior crossbites, (3) eliminate the functional shift and correct the dental midline, (4) establish Class I molar relationships, (5) obtain normal overjet and overbite, (6) relieve crowding, (7) obtain a stable occlusal relationship, and (8) improve facial and dental esthetics by establishing an esthetic smile.
Treatment alternatives
Orthognathic surgery to set back the mandible with the possibility of maxillary protraction, combined with fixed orthodontic treatment, was discussed with the patient. Skeletal discrepancy correction, maximum facial and dental esthetics, and establishment of an ideal occlusion would all be possible with this approach.
Orthodontics alone could help camouflage some skeletal and dental aspects of the malocclusion, improving esthetics and function. The orthodontic options included distalization of the mandibular dentition with temporary skeletal anchorage devices to establish Class I dental relationships and slow maxillary expansion to correct the posterior crossbites, a protraction facemask at night to correct the anterior crossbites, and, if necessary, mandibular incisor extraction to correct the anterior crossbite. Because the mandibular incisors were retroclined, extraction of 2 mandibular first premolars to correct her negative overjet was not advisable.
The patient declined orthognathic surgery, temporary skeletal anchorage devices, and the facemask. She did not want extractions; therefore, we decided to treat her with traditional orthodontic therapy using Class III elastics.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


