Thermal injuries to the skin can be a significant threat to life and health and are the source of considerable long-term disability. The face, head, and neck are among the most highly valued body surface areas in terms of function, appearance, and the person’s sense of self. This region conveys the special senses as well as our most important means of communication. It is the portal for nourishment and plays an important role in core body temperature regulation. It contains and protects the central nervous system and conveys the exchange of respiratory gases, and thus deep burns to the head and neck are immediately life-threatening. Burns to the face, in particular, can produce profound acute and chronic disability.
Burns to the face and neck seldom occur in isolation. They are most often part of a larger burn involving adjacent scalp, torso, and upper extremities. A serious burn to the face is among the accepted criteria for transfer of care to a burn center, where multidisciplinary patient-specific care can be delivered.
The skin reacts to thermal injury in prototypical ways, irrespective of the body surface involved. The end common pathway of tissue loss in a deep burn is coagulation necrosis, followed by liquefaction as autolytic and bacterial enzymes separate non-viable tissue from the living margin of the wound. The depth of injury determines the ability of the skin to recover from it. However, skin varies considerably in thickness and density of epidermal appendages. The recovery of sensation and elasticity that is required to maintain full function of underlying motor units also varies according to burn location, so injuries of similar depth can have widely varying effects on the functional outcomes of different surfaces. The face, head, and neck contain several unique regions that confer a very complex set of functional demands on the skin. Skin thickness and elasticity vary widely, and some areas carry a high density of hair follicles. Motion of underlying bones, joints, and muscle units also varies widely. It follows that serious burns on the face, head, and neck exhibit a broad range of functional and cosmetic outcomes.
Etiopathogenesis and Causative Factors
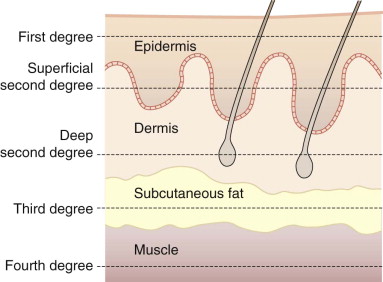
All thermal injuries can be classified in terms of injury mechanism, burn depth ( Fig. 5-1 ), and burn surface area. Hot water scalding mechanisms generally produce partial thickness burns, but may still lead to surgical skin replacement. Scalding with hot oil or other organic compounds often produces deeper burns requiring surgery.
Vapor flash incidents produce burns of varying depth ( Fig. 5-2 ), and many will heal without requiring surgery. Gasoline flash burns (see Fig. 5-2, B ) are generally deeper than other flash burns and often require skin grafting. Direct contact with flame (see Fig. 5-2, C ) commonly produces deep burns that will require surgical management. Chemical and electrical burns ( Fig. 5-3 ) vary widely in magnitude, depending on the specific agent and dosage of energy transfer to the tissue.




Appearance of burns varies widely and changes daily, making predictions of burn depth and behavior based on appearance hazardous. The mechanism of injury is more reliable in understanding the dosage of energy delivered. There are no widely accepted diagnostic imaging modalities that will improve on the accuracy of an experienced clinician who can synthesize injury mechanism, appearance, and host factors and then predict burn behavior and appropriate treatment.
The overriding factor that ultimately adversely affects the functional outcome of burn injuries on the head and neck is scar formation. All deeper burns heal with some degree of scarring. Thermal injuries have a unique capacity to produce proliferative, hypertrophic scars. Their formation is quite variable and influenced by inheritable predisposition, age, and burn depth. Additional complicating factors include infection, secondary breakdown of the healing wound, wound closure techniques, and other unknown influences. A hypertrophic scar confers much of the disability associated with burn injury, because it adversely affects durability, pliability, and appearance of the scar, and it prolongs pain and other discomforts.
Our innate inability to regenerate fully functional skin after a deep burn also results in reduced and altered sensation, leaving the host with impaired protective sensation. Loss of hair follicles affects appearance. Loss of sebaceous glands alters epidermal hydration and desquamation. Altered vasomotor control and the loss of sweat glands results in reduced local capacity to dissipate heat and regulate body temperature.
Partial thickness burns healing within 14 days will rarely leave significant functional or cosmetic impairment to the face. Burns healing between 14 and 21 days will often result in changes in texture and pigmentation, but generally do not produce significant scars. The deep partial thickness burn presents the most difficult dilemma to the surgeon. Burns requiring longer than 21 days to heal will always leave some degree of dermal scarring. The range of dysfunction can be very broad, ranging from subtle dermal tightening to horrific hypertrophic scarring resulting in gross functional and cosmetic impairments. Full thickness burns of any size affecting the face, head, and neck will require surgical management.
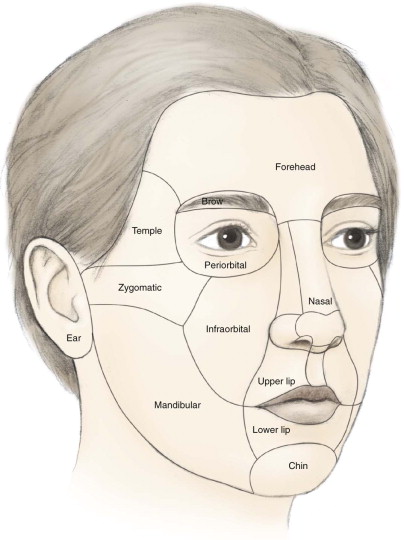
Burn surgeons generally agree that skin replacement on the face should follow facial cosmetic units ( Fig. 5-4 ). A general rule of thumb favors replacement of a complete cosmetic unit if greater than 50% of that cosmetic unit is involved with deep burn. The exact borders of the burn will be unique to each patient, and there is no substitute for experience in making appropriate decisions that minimize the consequences of both the burn and surgical intervention to close the burn.
The natural history of a shallow flash or scald burn on the face may be complete in as little as 1 week. But if the burn is deep and the scar requires maturation, this period may extend well beyond a year.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


