Total buccal crossbites are rare, but, when they occur, they can be extremely difficult to correct, even with surgery and orthodontics. In most patients with in-locking crossbites, the maxillary teeth erupt past their mandibular antagonists, creating severe occlusal difficulties. This article presents an adult patient with scissors-bite or partial telescoping bite bilaterally in the posterior region and an extracted mandibular first molar on the right side. She was treated with expansion of the mandibular arch, and the subsequent open bite was closed with the help of masticatory muscle exercises and high-pull headgear. The second and third molars were uprighted and moved mesially to close the extraction spaces.
Total buccal crossbite problems—ie, in-locking, Brodie bite, buccal nonocclusion, or telescoping bite—are rare, but, when they occur, they can be extremely difficult to correct, even with surgery and orthodontic treatment. In most patients with in-locking crossbites, the maxillary teeth erupt past their mandibular antagonists, creating severe occlusal difficulties and all but eliminating lateral excursions. Interestingly, a tendency toward maxillary buccal crossbite is found in Australian aborigines, who otherwise have ideal dentitions and perfect occlusions. Barrett called this “X” occlusion. Although it might initially be a transverse discrepancy with fault in the maxilla or the mandible, or in both jaws, it becomes a problem because the unopposed teeth in each arch supraerupt, creating a situation in which the elongated posterior teeth need to be intruded by several millimeters and repositioned laterally.
This rare situation of total buccal crossbite or total in-locking is due to a combination of excessive maxillary width and mandibular deficiency. The mandibular alveolar process might be narrow, but the width of the mandibular base is usually normal. Many clinicians have reported the potential effects on the health of the temporomandibular joints. Although the crossbite itself might not cause pathosis, compromised mastication could eventually lead to temporomandibular dysfunction. The extreme vertical overlap on the affected side makes it impossible to place orthodontic attachments on the facial surfaces of the mandibular teeth.
Loss of 1 tooth can have significant effects on the stability of both arches. With loss of a mandibular first molar, the mandibular second and third molars tip mesially, the mandibular second premolars move distally, and the opposing maxillary first molar is supraerupted. Mesial tipping of the mandibular second molar results in redundant edematous gingivae accumulating at the mesial surface, creating a defect that cannot be cleaned with routine home-care procedures. Mesial tipping places the distal cusps of the second molar into occlusal prominence, creating excursive deflective occlusal contacts that generate horizontal forces on the ipsilateral molars.
Case report
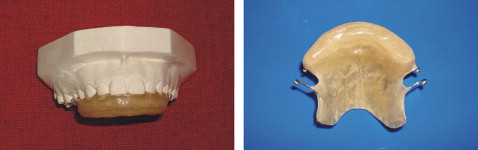
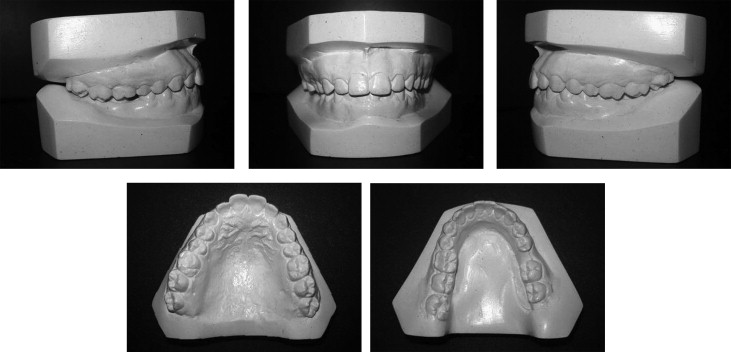
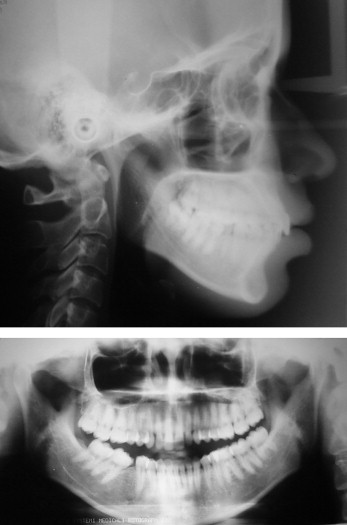
A 17-year-old girl came for treatment at the Department of Orthodontics and Dentofacial Orthopedics, King George’s University of Dental Sciences (now, CSM Medical University), Lucknow, Uttar Pradesh, India. Her chief complaint was inability to chew with her back teeth. The intraoral examination showed that her mandibular posterior teeth telescoped partially inside the maxillary teeth. She had a bilateral scissors-bite in the posterior region. Her mandibular right first molar had been extracted 4 years earlier because of a poor endodontic prognosis, resulting in mesial tipping and drifting of the second molar. This malocclusion developed partially because of lingual tipping of the mandibular buccal segments and partially because of loss of the first molar ( Figs 1 and 2 ). The maxillary right and left posterior teeth were extruded, and the labial surface of the first molar was worn, with the underlying dentin exposed. She had a Class I molar relationship on the left side and a Class II relationship on right side, because of mesial migration of the mandibular right second molar. The dental midline was deviated 1.5 mm toward the right side. Other than the Brodie bite and the mesial tipping and drifting of the mandibular second molar, almost everything else about her occlusion was within acceptable limits. Cephalometric analysis ( Table ) indicated that she was an average grower with a skeletal Class I pattern. The soft-tissue profile was convex with good frontal symmetry and facial proportions. The panoramic radiograph ( Fig 3 ) showed complete permanent dentition, except for the extracted mandibular right first molar, and the severe tipping and mesial drifting of the second molar into the extraction space.

| Variable | Pretreatment | Normal | Posttreatment | Change |
|---|---|---|---|---|
| SNA (°) | 82 | 82 ± 3 | 82 | 0 |
| SNB (°) | 79 | 79 ± 3 | 79 | 0 |
| ANB (°) | 3 | 3 ± 1 | 3 | 0 |
| Wits appraisal (mm) | –1 | 0 | –2.5 | –1.5 |
| Maxillary incisor to maxillary plane angle (°) | 118 | 108 ± 5 | 118 | 0 |
| Mandibular incisor to mandibular plane angle (°) | 95 | 92 ± 5 | 97 | 2 |
| Interincisal angle (°) | 124 | 133 ± 10 | 123 | –1 |
| Maxillomandibular plane angle (°) | 24 | 27 ± 5 | 24 | 0 |
| Upper anterior face height (mm) | 56 | 56 | 0 | |
| Lower anterior face height (mm) | 66 | 66 | 0 | |
| Face height ratio (%) | 54 | 55 | 54 | 0 |
| Mandibular incisor to APo line (mm) | 3 | 0-2 | 3.5 | 0.5 |
| Lower lip to Ricketts E-plane (mm) | 3 | –2 | 3 | 0 |
| Upper lip to E-line (mm) | 0 | −2- −3 | 0 | 0 |
Treatment options were limited for this patient. She refused to consider surgery, but, because the problem was caused mainly by buccolingual tipping of the dentition rather than an underlying skeletal problem, a nonsurgical approach was feasible. Therefore, the treatment plan called for dental correction with standard edgewise appliances, 0.022 × 0.028 in. The mandibular arch would be expanded, the maxillary arch constricted, and the mandibular molars uprighted. High-pull headgear with a force of 500 g per side would be used throughout the expansion period when cross elastics were used to aid in minimizing molar extrusion and to promote intrusion. Third molar extraction (except the mandibular right) would provide space for alignment.
Treatment progress
A maxillary removable plate ( Fig 4 ) was delivered to open the bite in the posterior region so that the mandibular posterior teeth could be banded. After 3 months of initial alignment and leveling, a 0.019 × 0.025-in stainless steel archwire was placed in the mandibular arch, and a 0.040-in stainless steel jockey arch ( Fig 5 ) expanded up to 1 cm was placed into the headgear tubes of the last banded molars. The jockey archwire was also tied to the stainless steel archwire at various regions to maintain the vertical level and stability of the jockey arch. Along with the jockey archwire, cross elastics (3/16-in, 4 oz, TP Orthodontics, LaPorte, Ind) or “through the bite elastics” were worn. Transverse expansion of the mandibular arch was continued along with cross elastics for 2.5 months, until the buccal segments began to upright to oppose the maxillary arch. High-pull headgear with a force of 500 g per side worn a minimum of 12 to 14 hours per day was used during the expansion period with the cross elastics. However, bite opening in the anterior region was inevitable, as vertical control of the mandibular molars could not be done while simultaneously uprighting them. As a consequence, 9 mm of bite opening was recorded at the incisor region ( Fig 6 ).