Alveolar bone that is insufficient to support implant placement due to lack of height or width may be augmented with grafting materials including bone morphogenic protein to create sites that are adequate for implant placement and long-term stability of implant-supported prosthesis. Bone morphogenic protein can be used alone or in concert with other bone graft materials as an alternative to invasive allograft bone harvesting procedures.
Key points
- •
Alveolar bone that is insufficient to support implant placement due to lack of height or width may be augmented with grafting materials including bone morphogenic protein (BMP) to create sites that are adequate for implant placement and long-term stability of an implant-supported prosthesis.
- •
BMP can be used alone or in concert with other bone graft materials as an alternative to invasive allograft bone-harvesting procedures.
- •
Patients who would otherwise not have been suitable candidates for major autologous bone grafting procedures can continue to benefit from implant reconstruction, with a less debilitating bone reconstructive procedure.
Introduction
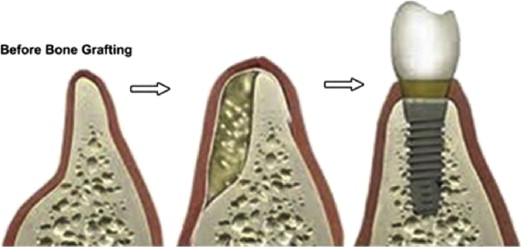
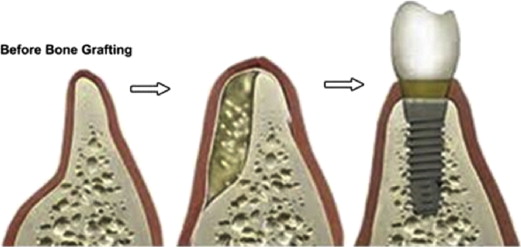
Implant-supported prostheses are currently widely accepted as the preferred treatment, by patients and doctors alike, for the partially and completely edentulous patient. Even though implant treatment is preferred, many patients present with insufficient alveolar bone to obtain implant osseointegration. Such a lack of quality alveolar bone ( Fig. 1 ), a contraindication of implant placement, is common in patients with long-standing or traumatic edentulism. Many treatments have been developed to prepare the site for implant placement and increase the likelihood of long-term implant stability.
Bone grafting, in particular the autogenous bone graft, has emerged as the treatment of choice of many dentists and oral surgeons. Autogenous bone grafts from the hip and tibia are considered to be the gold standard for large bony defects, but they can be less than ideal for a large number of patients. These procedures often require general anesthesia, hospitalization, and potentially serious postoperative complications at the donor site. Elderly patients, who often are the most in need of extensive preimplant grafting, are particularly susceptible to many postoperative complications including donor site morbidity, delayed wound healing, and gait disturbances. Given the potential complications and additional surgical sites, many patients are not good candidates for such grafting procedures, and additional patients may elect not to pursue what they view as such invasive treatment.
Given the large and growing patient population requiring nonautogenous bone grafting procedures, there is clearly a need in the general population for a nonautologous graft material that can be used to augment alveolar bone prior to implant placement. Many alloplastic materials and allografts ( Table 1 ) have been used. Most alloplastic materials are considered adequate but less than ideal. The ideal alloplastic material should not only be osteoconductive, but also osteoinductive ( Box 1 , Table 2 ).
| Graft Material | Characteristics | Examples |
|---|---|---|
| Allograft | A graft that is taken from a member of the same species as the host but is genetically dissimilar | Cadaver cortical/cancellous bone, FDBA, DFDBA |
| Xenograft | Graft derived from a genetically different species than the host | Bio-Oss, coralline HA, red algae |
| Alloplast (synthetic materials) | Fabricated graft materials | Calcium sulfate, bioactive glasses, HA, NiTi |
Osteogenesis
Osteogenesis refers to living cells, such as osteoblasts, that form new bone. The success of any bone grafting procedure depends on having enough bone-forming or osteogenic cells in the area. Iliac crest bone graft (ICBG), a type of autograft, is the only bone graft that contains enough cells to be considered osteogenic. Local bone from the primary surgical site generally contains cortical bone with much fewer cells. However, the presence of mesenchymal stem cells does not make a bone graft osteogenic. These stem cells require a signal, such as bone morphogenetic protein (BMP), to differentiate into osteoblasts.
Osteoconduction
Osteoconduction refers to the ability of some materials to serve as a scaffold onto which bone cells can attach, migrate, grow, and divide. In this way, the bone healing response is conducted through the graft site, just as a vine uses a trellis for support. Osteogenic cells generally work much better when they have a matrix or scaffold for attachment. Ceramics are strictly osteoconductive scaffolds and fall in the category of autograft extender or bone void filler.
Osteoinduction
Osteoinduction refers to the capacity of normal growth factors in the body to attract, proliferate, and differentiate primitive stem cells or immature bone cells to grow and mature, forming healthy bone tissue. Most of these signals are part of a group of protein molecules called BMPs, which are found in normal bone. Highly osteoinductive bone grafts have been evaluated as an autograft alternative in certain indications.
| Characteristic | Graft Material |
|---|---|
| Osteogenesis | Autograft |
| Osteoinduction | BMP, DFDBA, DBM |
| Osteoconduction | Bio-Oss, calcium phosphates, calcium sulfate, collagen, FDBA, glass ionomers HA, NiTi, BMP |
The search for such a material has led the dental community to bone morphogenic proteins (BMPs).
Introduction
Implant-supported prostheses are currently widely accepted as the preferred treatment, by patients and doctors alike, for the partially and completely edentulous patient. Even though implant treatment is preferred, many patients present with insufficient alveolar bone to obtain implant osseointegration. Such a lack of quality alveolar bone ( Fig. 1 ), a contraindication of implant placement, is common in patients with long-standing or traumatic edentulism. Many treatments have been developed to prepare the site for implant placement and increase the likelihood of long-term implant stability.
Bone grafting, in particular the autogenous bone graft, has emerged as the treatment of choice of many dentists and oral surgeons. Autogenous bone grafts from the hip and tibia are considered to be the gold standard for large bony defects, but they can be less than ideal for a large number of patients. These procedures often require general anesthesia, hospitalization, and potentially serious postoperative complications at the donor site. Elderly patients, who often are the most in need of extensive preimplant grafting, are particularly susceptible to many postoperative complications including donor site morbidity, delayed wound healing, and gait disturbances. Given the potential complications and additional surgical sites, many patients are not good candidates for such grafting procedures, and additional patients may elect not to pursue what they view as such invasive treatment.
Given the large and growing patient population requiring nonautogenous bone grafting procedures, there is clearly a need in the general population for a nonautologous graft material that can be used to augment alveolar bone prior to implant placement. Many alloplastic materials and allografts ( Table 1 ) have been used. Most alloplastic materials are considered adequate but less than ideal. The ideal alloplastic material should not only be osteoconductive, but also osteoinductive ( Box 1 , Table 2 ).
| Graft Material | Characteristics | Examples |
|---|---|---|
| Allograft | A graft that is taken from a member of the same species as the host but is genetically dissimilar | Cadaver cortical/cancellous bone, FDBA, DFDBA |
| Xenograft | Graft derived from a genetically different species than the host | Bio-Oss, coralline HA, red algae |
| Alloplast (synthetic materials) | Fabricated graft materials | Calcium sulfate, bioactive glasses, HA, NiTi |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


