The deficient alveolar ridge has been an impediment to the placement of dental implants in the past. A greater comprehension of bone biophysiology and biotechnology has greatly increased the surgical options available to rehabilitate these patients. Technology and regenerative science has also allowed clinicians to simplify some of the approaches to these patients. This article presents the authors’ perspective on the current surgical treatment methodologies that have been most beneficial in reconstructing atrophic alveolar bone.
Key points
- •
Optimum wound healing is achieved with gentle manipulation of the mucoperiosteal envelope.
- •
In vertical augmentation the inverted L shaped block graft is most suited.
- •
Appropriate vector control of the transport segment is critical.
- •
Correct surgical technique is enhanced by the use of adjuncts such as bone morphogenic protein.
Introduction
Remarkable advances in dentistry have occurred in the twenty-first century, and the achievements are many. However, partial and complete edentulism is still a significant health care problem today, and this has major negative ramifications, both for the individuals afflicted and the wider society. The situation is even worse in a large segment of the developing world, where public dental health care is grossly inadequate or nonexistent. Despite this, patients worldwide still expect the best solutions for their problems, hence the greater utilization of implant solutions in dental health care.
This development has been driven by several factors, the major ones being improvements in technology, cost reductions, increased simplicity of the procedure, and greater demand from patients. However, one of the major scientific factors that have contributed to this growth is our understanding and, by extension, use of bone-grafting techniques to provide implant options to patients who previously were not candidates for this treatment modality because of inadequate bone. This article seeks to explore this realm of implant surgery, and suggests guidelines in the management of patients with deficient alveolar bone.
Introduction
Remarkable advances in dentistry have occurred in the twenty-first century, and the achievements are many. However, partial and complete edentulism is still a significant health care problem today, and this has major negative ramifications, both for the individuals afflicted and the wider society. The situation is even worse in a large segment of the developing world, where public dental health care is grossly inadequate or nonexistent. Despite this, patients worldwide still expect the best solutions for their problems, hence the greater utilization of implant solutions in dental health care.
This development has been driven by several factors, the major ones being improvements in technology, cost reductions, increased simplicity of the procedure, and greater demand from patients. However, one of the major scientific factors that have contributed to this growth is our understanding and, by extension, use of bone-grafting techniques to provide implant options to patients who previously were not candidates for this treatment modality because of inadequate bone. This article seeks to explore this realm of implant surgery, and suggests guidelines in the management of patients with deficient alveolar bone.
Biological principles
To use bone grafts efficiently, it is important to have a complete understanding of the physiology underlying bone grafting. The biological principles of autogenous bone grafting are similar to those that apply to how long bone fractures heal. The sequence of events starts with the immediate phase, followed by the development of osteogenic tissue and, finally, remodeling.
During the immediate phase, hemostasis occurs with clot formation and inflammation. Following the immediate phase, with the appropriate chemical signals, osteogenic tissue then lays down new bone material that will eventually become remodeled. These events are not distinct but actually overlap.
Specific to bone grafting are 3 important terms: osteogenesis, osteoconduction, and osteoinduction.
When a graft is positioned in a donor site, it carries with it osteogenic cells, some of which survive and are able to contribute to osteoid formation. These osteogenic cells are believed to come from the periosteum (especially the cambium layer), endosteum, marrow, and intracortical structures of the graft.
As the bone graft sits in the recipient site, it is surrounded by an inflammatory milieu, and partial bone necrosis of the graft occurs via osteoclasts. The extent and duration of osteoclastic activity depends on the nature of the bone graft (cortical vs cancellous) and, by extension, the density of the graft. Once the graft has undergone some amount of necrosis and resorption, it then acts as a scaffold for neoangiogenesis to occur within the graft. This vessel penetration of the graft allows osteogenic cells to invade the graft and create new bone formation. This series of events is termed osteoconduction (creeping substitution). During the proliferative phase of the graft take, certain molecules induce significant amounts of mitosis of osteoprogenitor cells and then direct these cells to be committed into differentiated osteoblasts. This phenomenon is called osteoinduction, and of these molecules bone morphogenic protein (BMP) is one that has been extensively studied and has been shown to have significant impact on new bone formation, particularly BMP-2, BMP-4, and BMP-7.
Within autogenous bone grafts, the biological environment varies somewhat between cancellous and cortical graft. Cancellous grafts are less dense and, as such, the amount of necrosis and osteoclastic bone resorption necessary for vascular invasion is less. Osteoprogenitor cells are brought into and penetrate further into the graft, allowing for a more complete revascularization and replacement of bone. Owing to their dense organization, cortical grafts have to undergo more necrosis and osteoclastic activity for new vessels to permeate them. As a result of this, the extent of vascularization is less thorough, hence there is less new bone formation.
Other factors that affect bone graft survival include surgical and recipient site factors.
Surgical factors, such as graft orientation in the recipient site, are important. Having the graft’s cancellous portion abutting the recipient site’s cancellous segment is called orthotopic adaptation, and aids in increasing graft survival. The preservation of the periosteum of the graft is also crucial, as the cambium layer harbors significant amounts of osteoprogenitor cells.
Recipient site factors include presence of infection, previous irradiation, and whether the graft is fixed or not. Both infection and previous irradiation provide a hostile environment for the graft, which decreases the likelihood of graft take. Graft fixation is of greater importance when performing block grafting.
Types of bone grafts
Bone grafts are generally categorized into autogenous and nonautogenous grafts. These 2 broad categories can then be further subdivided. The difference between them is the actual source of graft material. Autogenous bone is obtained from the individual, whereas nonautogenous is either allogenic (ie, obtained from another human being) or xenogeneic (ie, from another species).
Autogenous bone grafts are considered the gold standard for bone grafting. However, there are several factors that have driven greater consideration for the use allogenic and xenogeneic bone grafts. These issues are primarily donor site morbidity, the quantity of graft material available, and the ease of procurement in an outpatient setting.
Bone grafts can be used in the form of blocks, which may be cortical or corticocancellous, or particulate, which also can be cortical, cancellous, or a mixture of both ( Table 1 ).
| Donor Site | Type |
|---|---|
| Mandibular symphysis | Corticocancellous |
| Mandibular ramus | Corticocancellous |
| Coronoid process | Cortical |
| Zygomatic buttress | Cortical |
| Maxillary tuberosity | Cancellocortical |
| Maxillary tori | Corticocancellous |
| Mandibular tori | Corticocancellous |
| Calvarium | Cortical |
| Clavicle | Cortical |
| Ilium | Corticocancellous |
| Tibia | Cancellocortical |
| Rib | Cancellocortical |
Block corticocancellous grafts have the advantage of bringing both cancellous and cortical bone into the recipient site. This combination gives rise to immediate structural support via its cortical component, and the cancellous part brings in tissue that allows for faster neoangiogenesis of the graft and results in a more complete revascularization, thus limiting the amount of graft resorption. Moreover, block grafts can be used to fill larger defects without requiring the use of membranes.
Cortical grafts, as mentioned earlier, provide immediate support to the recipient site without the need for a membrane to protect it. The shortcoming of cortical grafts is that they eventually undergo more resorption and tend to revascularize less thoroughly.
Cancellous and corticocancellous particulate grafts can act as fillers, but generally need a barrier membrane to hold the graft in situ. Cancellous grafts have the advantage, in the setting where there is already adequate stability, of bringing material that becomes rapidly revascularized and is almost fully ossified. Particulate grafts can represent several different types of grafts; mineralized and demineralized cortical bone and mineralized and demineralized corticocancellous bone are a few examples. These types of grafts require barrier membranes to be used during grafting. In autogenous and some allogenic particulate grafts, BMPs are retained and assist in bone formation via osteoinduction.
The use of allogenic bone grafts in implantology has been steadily increasing, and studies are demonstrating its consistent efficacious use. One of the major concerns about allogenic grafts is their antigenicity and the possibility of human immunodeficiency virus (HIV) transmission. One particular study demonstrated no significant antigenicity in an allograft transplantation present for 30 years. Some studies state that after processing an allogenic bone graft, because of better screening of donors, there is a 1 in 8,000,000 chance of the graft being infected with HIV and that the effective rate of transmission is approximately 1 in 1,600,000 grafts, rendering the risk extremely low.
Xenografts, like allografts, have been in use for some time and, like allografts, the main reasons for their use are to reduce donor site morbidity, increase the available quantity, and provide greater simplicity of procurement and use. The major type used to date is bovine bone. There has also been increased interest in the use of equine bone. Several studies are emerging to indicate that xenografts can be just as successful in grafting as autogenous grafts.
Alloplasts are natural or synthetic materials that consist of block or particulate forms of calcium-derived inorganic materials, primarily calcium phosphates, calcium sulfates, and bioactive glass. Alloplasts are used as fillers, most often combined with autogenous or allogenic bone. In more recent times, various growth factors and platelet-rich plasma (PRP) have been added to the proverbial soup. These materials provide a scaffold for the ingress of native bone-forming tissue and autogenous bone-forming cells to aid in bone production. At present their efficacy as stand-alone bone graft materials has not been proven.
Evaluation of alveolar bone and adjacent soft tissue
The magnitude and nature of the residual bone is the major determinant in deciding on the type of graft material used and from where it is obtained. The height and width of the ridge together with the inherent quality of the bone can be readily assessed with clinical examination and radiographic studies. More detailed information about the quantity and quality of the bone is readily available with the use of cone-beam computed tomography (CBCT) scanning technology. Gulsahi classified the different types of alveolar bone as types 1 to 4, with type 1 being the most compact and type 4 the least dense.
Choices of graft material
The decision on what type of graft material to use depends on several factors. Recipient-site defect location, the extent of the size of the defect, the medical status of the patient, the patient’s desires, and prosthodontic considerations are a few of the variables to consider. Autogenous donor-site harvesting can be from local, regional, or distant sites.
For small to moderate size defects, local donor sites include posterior mandibular ramus, mandibular symphysis, coronoid process, and zygomatic buttress, to name a few. Maxillary tuberosities and maxillary and mandibular tori can also be used. The advantages of using these local grafts are that they can be performed as office procedures and produce minimal morbidity. A list of donor graft sites are outlined in Table 2 . The main disadvantage of using these local sites is the limited supply (see Table 1 ; Table 2 ).
| Local | Regional | Distant |
|---|---|---|
| Symphysis | Clavicle | Rib |
| Mandibular ramus | Calvarium | Radius |
| Coronoid process | Tibia | |
| Maxillary tuberosity | Ilium | |
| Maxilla and mandibular tori | ||
| Zygoma buttress |
There are many distant donor sites. The selection depends on the type of graft that needs to be harvested (block or particulate, cortical, corticocancellous, or cancellous) and the amount required. When large blocks are needed, most surgeons prefer the ilium. Several studies have documented that harvesting bone from the anterior ilium has a lower morbidity than was previously thought. A significant amount of cancellous bone can also be obtained from the tibia with a limited amount of cortical bone and minimal side effects. It also does not require general anesthesia and can be obtained in an outpatient setting. The calvarium has been used to provide long strips of cortical bone when necessary. However, harvesting of cranial bone is usually performed under general anesthesia. Smaller amounts can be obtained as an office procedure with minimal morbidity. Other sites used for bone grafting include the rib and fibula.
As stated earlier, allografts and xenografts are now being used with increasing frequency, often combined with BMP and other bone growth–promoting factors. Many reports in the literature studying their use have documented their efficacy in a variety of clinical situations. Some actually show results comparable with those for autogenous grafts. Further ongoing evaluation of their antigenicity and the risk of disease transmission will help to dispel some of the fears of both patients and clinicians.
Surgical techniques
Suggested Bone-Grafting Protocol
There is a plethora of techniques currently used to address alveolar ridge deficiencies. The current gold standard for the type of graft material remains autogenous bone. However, other materials by themselves or in combination with autogenous bone are currently used with varying degrees of success. Several studies have even suggested that materials other than autogenous bone have a significantly greater implant success rate. Al-Nawas and Schiegnitz have suggested the same in a recent European-based retrospective analysis that compared autogenous bone grafts with other materials used in sinus grafting and alveolar ridge block grafting. The reality is that with the inclusion of BMP, PRP, and other growth-promoting factors, there is greater choice for graft materials that do not involve a second surgical site, which are especially appropriate for small defects.
Achieving bone formation in defects via the innate ability of local tissues such as periosteum and the schneiderian membrane without introduction of a graft has been documented since early 2000. Lundgren and colleagues described the formation of new bone in the sinus simply by doing a sinus lift. No graft material or exogenous bone growth–promoting factors were placed in the wound. A recent article by Altintas and colleagues, in which a double-blind prospective study was done comparing bone formation after sinus lift with and without grafting, showed no significant difference in the amount and quality of the bone 3 months after surgery. In fact, the 6-month follow-up evaluation showed greater density of bone in the nongrafted sinus. This finding is important, not just because of the implication that clinicians may induce bone formation now and in the future without the introduction of graft material or growth-promoting factors, but also because it reinforces the need to treat the adjacent tissues gently and to preserve the potential bone-inducing areas even when graft material is being placed, as this will improve success rates.
Some grafting methods may be site specific while others can be used in most situations. However, procedures such as guided bone regeneration and especially the ridge-splitting technique do not produce predictable results in vertical defects, and are therefore restricted to horizontal defects.
Vertical augmentation remains the most challenging scenario. Guided bone regeneration with a titanium-reinforced membrane or titanium mesh, vertical onlay block grafts, subnasal grafting, sinus lifts, LeFort I with horizontal interpositional grafts, and isolated horizontal interpositional grafts are all used to increase the height of the alveolar bone, with different degrees of success. Distraction osteogenesis however a more reliable and predictable technique to effectuate changes in the vertical dimension ( Table 3 ).
| Horizontal Defects | Horizontal/Vertical Defects | Vertical Defects |
|---|---|---|
| Guided bone regeneration (GBR) with graft | GBR with graft | GBR with graft and tented membrane |
| Horizontal onlay corticocancellous blocks with or without membrane | Horizontal/vertical onlay block bone graft | Onlay block bone grafts |
| Split vertical alveolar ridge with interpositional graft | Distraction osteogenesis | Distraction osteogenesis |
| Titanium mesh crib with particulate bone graft | Le Fort I with horizontal interpositional bone graft | |
| Titanium mesh crib with particulate bone graft |
The more common surgical methods used at the authors’ center are: guided bone regeneration with particulate matter; ridge splitting with interpositional bone graft; onlay block bone grafting; distraction osteogenesis; LeFort maxillary downfracture with interpositional graft; subnasal graft; and mandibular sandwich osteotomy ( Fig. 1 ).
The focus here is on the more frequently performed procedures. Radiographic studies, including a CBCT scan to assess the dimensions of the defect and to plan for possible donor sites, should be done. A thorough physical examination with a review of the medical history is also performed.
Implant therapy is restorative driven. Therefore, a thorough restorative workup by the restorative dentist is vital before surgery. This workup should include mounted study models and waxups of the desired location of the final restoration. This model will help in deciding the reconstructive method of choice and the graft materials to be used.
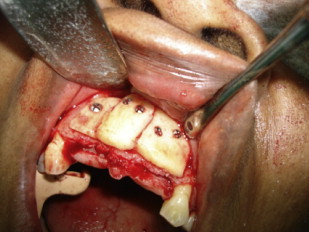
Guided bone regeneration
This technique consists of creating a mucoperiosteal envelope that will contain the graft material. A variety of incisional designs are used. The authors’ standard approach is to use a crestal incision with extension around the gingival sulcus where teeth are adjacent to the defect. The vertical leg of the incision is made 1 or 2 teeth away from the defect, depending on the quality and disease status of the gingiva. The incision is limited to 1 vertical leg if possible. Extensive mobilization of the flap is then done after periosteal release incisions are made ( Figs. 2 and 3 ).





