Upper and lower blepharoplasty is performed to treat prominent orbital fat, redundant skin and muscle, and other esthetic problems in the periocular region. Frequently, upper blepharoplasty is performed to remove excess skin that partially occludes the visual axis. Lower blepharoplasty is rarely indicated to treat a functional abnormality of the lower lids; rather, it is overwhelmingly cosmetic. Both procedures can have a dramatic impact on appearance and facial expression. Blepharoplasty can significantly alter the interaction, real or perceived, of patients within their social contexts; it can also disrupt specific ethnic features that are important in self-identity. When not performed carefully, blepharoplasty can lead to decreased vision, discomfort, deformity, and reoperation. Therefore, both careful patient selection and precise surgical technique are essential in the performance of upper and lower blepharoplasty.
Etiopathogenesis/Causative Factors
Many potential factors can lead to the real or perceived prominence of orbital fat and excessive periocular skin and muscle. Studies have shown that orbital fat volume may increase with age. This process of orbital fat expansion can also be observed in an exaggerated fashion in a subset of patients with thyroid ophthalmopathy. Involutional changes in the orbital septum may further enhance the prominence of the orbital fat compartments. Skin can lose fixation to the underlying tissues and be stretched by the expanding or prolapsing orbital fat compartments. The lateral and medial canthal tendons can become lax as a result of senile changes or excessive manipulation. Descent of the brows may occur and lead to the perception of excess skin between the brow and upper eyelashes. In addition, recurrent inflammatory or traumatic insults to the upper and lower eyelids can result in thinning of the tissues, redundancy of skin and muscle, loss of skin fixation, and laxity of the tendinous supporting structures of the upper and lower eyelids.
Pathologic Anatomy
The Upper Eyelid and Surrounding Tissue
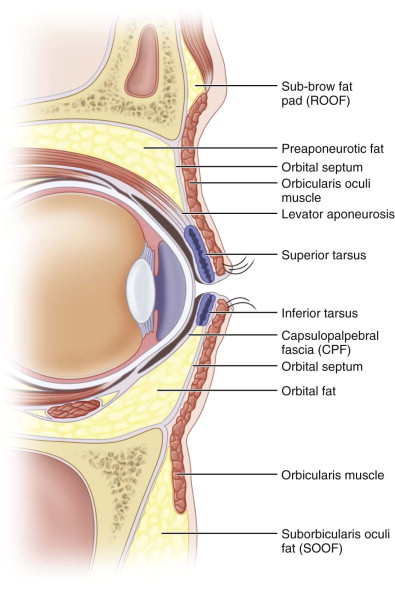
Many excellent publications have detailed the anatomy of the peri-ocular soft tissues. The upper eyelid crease and fold are essential elements of upper eyelid surface anatomy ( Fig. 108-1 ); inattention to these aspects of anatomy can foil the surgical goal of a youthful appearance or, worse, alter important ethnic features. The upper eyelid crease is formed by the anterior attachments of the levator aponeurosis that pass through the orbicularis and insert onto the dermis; it is modulated by the mass of pre-aponeurotic orbital fat. This fat is confined by the orbital septum, which inserts variably onto the levator aponeurosis or superior tarsus. In non-Asians, the crease usually adopts a semilunar shape; in Asians, the crease is generally much flatter in curvature.
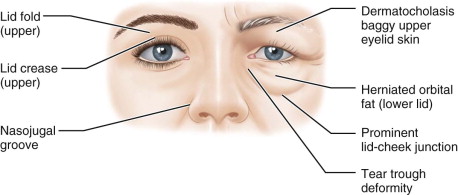
The eyelid fold is defined by the eyelid crease. It functions to provide tissue for recruitment when the eyelid closes, thereby preventing corneal exposure. Similar to the eyelid crease, it has significant ethnic variation. The eyelid fold is also modulated by the relative position of the brow; as the brow descends, the fold can become more prominent as the skin beneath the brow becomes redundant. Redundant upper eyelid skin is referred to as dermatochalasis. More subtly, there are patients with apparent excess skin who simply have lost deep fixation of the lid crease and consequently have a poorly defined lid-fold complex; not uncommonly, these patients have previously undergone eyelid surgery ( Fig. 108-2 ).

The lid fold may or may not join smoothly into an epicanthal fold, a redundant bridge of skin that joins the upper and lower eyelids medially. There are several variants of epicanthal folds; in general, alteration of the structure of these folds should be avoided unless that is the specific surgical goal.
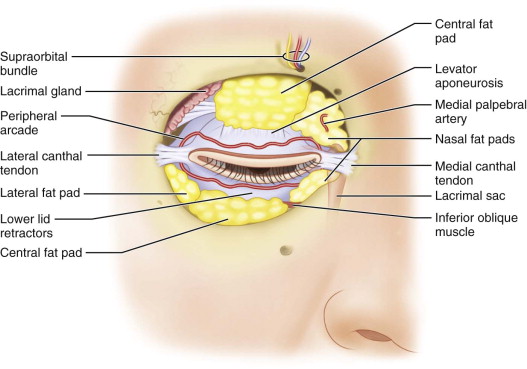
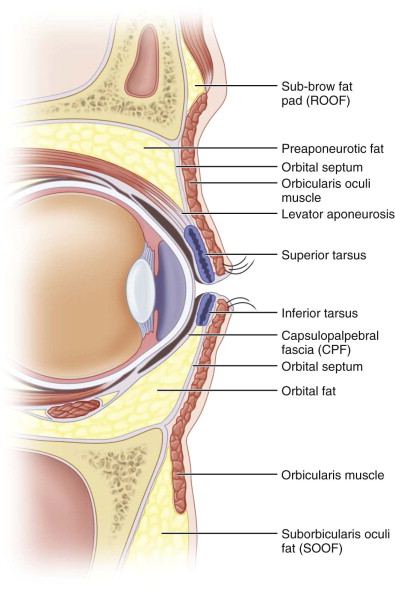
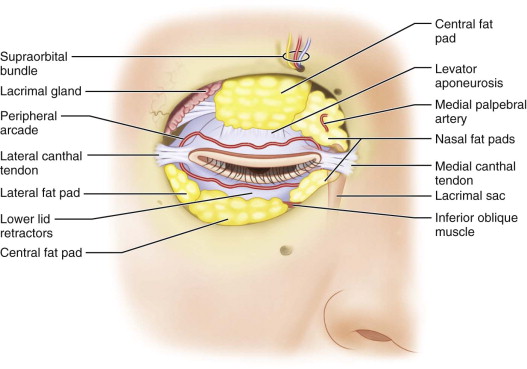
Contributing to the bulky appearance of the upper eyelid are the orbicularis oculi muscle, the pre-aponeurotic orbital fat, the lacrimal gland, and the retro–orbicularis oculi fat (ROOF). The pre-aponeurotic fat is composed of two distinct pockets, a larger central fat pocket and a smaller medial fat pocket. The medial pocket is deeper and whitish in appearance and contains the medial palpebral artery. Deeper structures that are easily avoided during upper blepharoplasty are the supraorbital bundle and the trochlea ( Fig. 108-3 ). The lacrimal gland, however, is often encountered and is easily dealt with. The ROOF is preseptal and is partially responsible for the appearance of “heaviness” of the sub-brow tissue in some patients ( Fig. 108-4 ). In Asians, the ROOF often extends inferiorly toward the pretarsal space.
The Lower Eyelid and Surrounding Tissue
The surface anatomy of the lower eyelid has several important cosmetic elements (see Fig. 108-1 ). The lid-cheek junction delineates the inferior orbital rim and is accentuated by the orbital septum, arcus marginalis, and orbitomalar ligament. A prominent nasojugal groove, known as a tear trough deformity, can be of cosmetic importance and is often the target for periocular injectable fillers or fat repositioning. Younger patients may also have lower eyelid folds. Nasally, an epicanthal fold may extend from the lower lid toward the upper lid.
There are three anterior orbital fat pockets in the lower lid. The medial and central fat pockets are separated by the inferior oblique muscle, which is frequently encountered during lower blepharoplasty and should be left untouched. The arcuate expansion of the inferior oblique separates the central and lateral pockets and can be violated without consequence. The lacrimal sac is deep and medial to the nasal fat pocket and is easily avoided. The medial palpebral artery is often encountered in the medial fat pocket and frequently requires attention (see Fig. 108-3 ).
Pathologic Anatomy
The Upper Eyelid and Surrounding Tissue
Many excellent publications have detailed the anatomy of the peri-ocular soft tissues. The upper eyelid crease and fold are essential elements of upper eyelid surface anatomy ( Fig. 108-1 ); inattention to these aspects of anatomy can foil the surgical goal of a youthful appearance or, worse, alter important ethnic features. The upper eyelid crease is formed by the anterior attachments of the levator aponeurosis that pass through the orbicularis and insert onto the dermis; it is modulated by the mass of pre-aponeurotic orbital fat. This fat is confined by the orbital septum, which inserts variably onto the levator aponeurosis or superior tarsus. In non-Asians, the crease usually adopts a semilunar shape; in Asians, the crease is generally much flatter in curvature.
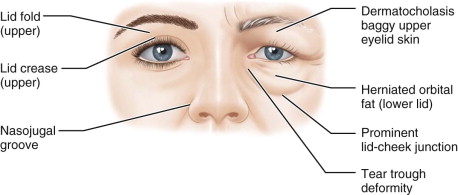
The eyelid fold is defined by the eyelid crease. It functions to provide tissue for recruitment when the eyelid closes, thereby preventing corneal exposure. Similar to the eyelid crease, it has significant ethnic variation. The eyelid fold is also modulated by the relative position of the brow; as the brow descends, the fold can become more prominent as the skin beneath the brow becomes redundant. Redundant upper eyelid skin is referred to as dermatochalasis. More subtly, there are patients with apparent excess skin who simply have lost deep fixation of the lid crease and consequently have a poorly defined lid-fold complex; not uncommonly, these patients have previously undergone eyelid surgery ( Fig. 108-2 ).

The lid fold may or may not join smoothly into an epicanthal fold, a redundant bridge of skin that joins the upper and lower eyelids medially. There are several variants of epicanthal folds; in general, alteration of the structure of these folds should be avoided unless that is the specific surgical goal.
Contributing to the bulky appearance of the upper eyelid are the orbicularis oculi muscle, the pre-aponeurotic orbital fat, the lacrimal gland, and the retro–orbicularis oculi fat (ROOF). The pre-aponeurotic fat is composed of two distinct pockets, a larger central fat pocket and a smaller medial fat pocket. The medial pocket is deeper and whitish in appearance and contains the medial palpebral artery. Deeper structures that are easily avoided during upper blepharoplasty are the supraorbital bundle and the trochlea ( Fig. 108-3 ). The lacrimal gland, however, is often encountered and is easily dealt with. The ROOF is preseptal and is partially responsible for the appearance of “heaviness” of the sub-brow tissue in some patients ( Fig. 108-4 ). In Asians, the ROOF often extends inferiorly toward the pretarsal space.
The Lower Eyelid and Surrounding Tissue
The surface anatomy of the lower eyelid has several important cosmetic elements (see Fig. 108-1 ). The lid-cheek junction delineates the inferior orbital rim and is accentuated by the orbital septum, arcus marginalis, and orbitomalar ligament. A prominent nasojugal groove, known as a tear trough deformity, can be of cosmetic importance and is often the target for periocular injectable fillers or fat repositioning. Younger patients may also have lower eyelid folds. Nasally, an epicanthal fold may extend from the lower lid toward the upper lid.
There are three anterior orbital fat pockets in the lower lid. The medial and central fat pockets are separated by the inferior oblique muscle, which is frequently encountered during lower blepharoplasty and should be left untouched. The arcuate expansion of the inferior oblique separates the central and lateral pockets and can be violated without consequence. The lacrimal sac is deep and medial to the nasal fat pocket and is easily avoided. The medial palpebral artery is often encountered in the medial fat pocket and frequently requires attention (see Fig. 108-3 ).
Diagnostic Studies
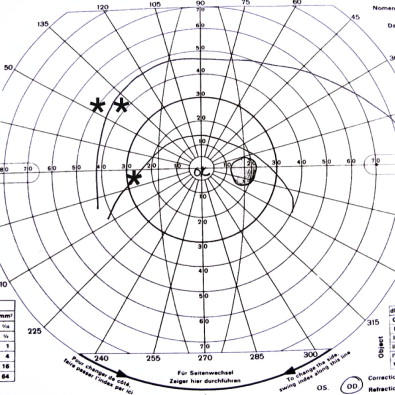
When upper blepharoplasty is performed for functional, vision-limiting purposes, visual field documentation is required for reimbursement by most insurers. A technician manually maps a patient’s visual field for each eye in the native state with the use of a Goldmann perimeter ( Fig. 108-5 ). The technician then tapes the redundant lid skin up and repeats the test to demonstrate the functional improvement achieved when tissue is withdrawn from the visual axis. This test can also be performed with an automated perimeter.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


