Introduction
Bisphosphonates are a class of drugs commonly prescribed to treat osteoporosis. They act by decreasing the resorption of bone. Since tooth movement depends on bone remodeling, these drugs can impact orthodontic treatment. The purpose of this study was to evaluate the extent to which bisphosphonate therapy is a risk factor for poor orthodontic outcomes.
Methods
Orthodontists were invited to participate in the study by performing case reviews of women over age 50 who were treated from 2002 through 2008. Women who used bisphosphonates were compared with women who did not have a history of bisphosphonate use. Outcomes assessed included treatment time, osteonecrosis of the jaws, incisor alignment, incomplete space closure, and root parallelism.
Results
The records for 20 subjects with bisphosphonate exposure were collected, as well as records for 93 subjects without bisphosphonate exposure. In patients undergoing extractions, treatment times were significantly longer if they had a history of bisphosphonate use. No occurrences of osteonecrosis of the jaws were reported, nor did patients end treatment with incisor alignment discrepancies greater than 1 mm, regardless of bisphosphonate exposure. Among patients with extractions or initial spacing, there were higher odds of incomplete space closure (odds ratio, 13) and poor root parallelism (odds ratio, 26) at the end of treatment for patients using bisphosphonates.
Conclusions
Bisphosphonate use is associated with longer treatment times among extraction patients, increased odds of poor space closure, and increased odds of poor root parallelism.
Bisphosphonates are a class of commonly prescribed drugs that primarily act to decrease the resorption of bone by inhibiting osteoclastic activity, thereby decreasing bone turnover. With the Food and Drug Administration’s approval of alendronate (Fosamax; Merck, Whitehouse Station, NJ) in 1995, they have become among the most prescribed drugs in the United States. Osteoporosis treatment is the most common application of bisphosphonate therapy, and the oral forms of medication that treat this condition account for over 99% of bisphosphonate prescriptions. Alendronate, ibandronate, and risedronate are oral agents used primarily to prevent or treat osteoporosis, although some are also used in the treatment of Paget’s disease and osteogenesis imperfecta. The more potent intravenously administered bisphosphonates—pamidronate and zoledronic acid—are the current standard of care for the reduction of bone pain, hypercalcemia of malignancy, and skeletal complications in patients with multiple myeloma and lung, breast, and other cancers.
Although the reduction in morbidity and mortality from the various conditions mentioned previously is desirable, osteoclast suppression has been linked to a severe adverse side effect: osteonecrosis of the jaws. In 2003, Marx alerted the dental community to the possible relationship between intravenous bisphosphonate therapy and necrosis of the jaws. He reported on 36 patients who were receiving intravenous bisphosphonates, all with cases of bone exposure that were unresponsive to surgical or medical treatments. His letter to the editor prompted others to review their records and report on similar findings; Ruggerio et al published a review of 56 patients with osteonecrosis of the jaws associated with bisphosphonate therapy, 7 of whom were receiving the oral bisphosphonate alendronate or risedronate for the treatment of osteoporosis. One year later, Migliorati et al presented 18 patients with osteonecrosis of the jaws, 17 of whom were receiving pamidronate or zoledronic acid as part of their cancer regimen; 1 patient was receiving alendronate for the treatment of osteopenia. Additional insight was provided by Marx et al in 2005, when they reviewed 119 cases of bisphosphonate-related bone exposure to determine the type, dosage, and duration of bisphosphonate therapy that the patients had received. They found that many osteonecrotic sites were related to extractions, periodontal diseases, periodontal surgeries, placement of dental implants, and apicoectomies, although spontaneous osteonecrosis occurred in 30 of the 119 patients. Most concerning were the 3 osteonecrotic cases related to the oral administration of alendronate for the treatment of osteoporosis. An estimated 18 million prescriptions for alendronate were written in 2005, and the half-life of the drug is estimated to be greater than 10 years, so there was concern that more patients with alendronate-associated necrosis of the jaw would surface. A systematic review in 2006 of all reports concerning bisphosphonates and osteonecrosis of the jaws uncovered a total of 368 cases. The authors noted that most cases involved intravenous bisphosphonates used to treat multiple myeloma or various metastatic diseases, although 15 cases of osteonecrosis were associated with the treatment of osteoporosis and oral bisphosphonates. The results of the systematic review should be viewed cautiously, however, since it was written before the establishment of the American Association of Oral and Maxillofacial Surgeons’ definition of osteonecrosis. Two nationwide studies in Japan showed an increased prevalence of osteonecrosis after improved awareness and monitoring.
Whereas the literature relating aspects of bisphosphonate use to osteonecrosis of the jaws is fairly well established, the research relating bisphosphonate use to orthodontic-specific complications has been largely anecdotal, relying heavily on biologic plausibility, animal studies, and scattered case reports. Decreased orthodontic tooth movement has been found in mice and rats that were administered bisphosphonates. Fujimura et al also used scanning electron micrographs and histologic stains to determine that bisphosphonates decrease osteoclast formation during orthodontic tooth movement in mice. A few case reports detailing the orthodontic treatment of patients who were taking bisphosphonates have been published. One report described 3 patients who underwent orthodontic treatment, with varying results. The first patient was a 60-year-old woman taking alendronate for osteoporosis. Her nonsurgical, nonextraction orthodontic treatment proceeded for 4.5 years before it was discontinued by the orthodontist because of decreased tooth movement and fear of osteonecrosis. The second patient was a 50-year-old woman who began taking alendronate before the extraction of a mandibular premolar and the start of orthodontic therapy to close the space. Despite discontinued bisphosphonate use within 6 months from the start of orthodontic bonding, slow tooth movement and poor root parallelism were observed throughout treatment. The third patient was a 74-year-old woman who had been taking alendronate for 3 years. In this case, the bisphosphonate was discontinued 3 months before the necessary incisor extraction and during the orthodontic treatment. Normal extraction healing, parallel roots, and space closure were achieved. Two case reports by Rinchuse et al offer additional insight. Their first patient was a 35-year-old woman taking oral bisphosphonates. She had extractions of the right first premolars, and the authors reported difficulty in closing these extraction spaces. In addition, treatment time was prolonged, and the finished results were less than ideal. The second patient reported on was 77 years old, and she was referred for space closure after removal of a mandibular incisor. Tooth movements and space closures were extremely difficult. After 11 more months, orthodontic treatment was discontinued because of a developing area of osteonecrosis in the posterior mandible. The spaces were incompletely closed, and the authors stated that any space closure that was achieved was the result of tipping, rather than bodily movement of the teeth.
Adults currently comprise over 20% of all orthodontic patients. Among this patient population are postmenopausal women, who are at an increased risk of developing osteoporosis due to decreased estrogen secretion and the complementary increase in osteoclastic activity. It is estimated that women comprise 80% of the approximately 12 million Americans older than age 50 who have osteoporosis and 80% of the approximately 40 million Americans over age 50 with osteopenia, contributing to the more than 24 million prescriptions for bisphosphonates issued in the United States during 2007. Although the American Dental Association has released updated dental management guidelines for specialists treating patients receiving oral bisphosphonate therapy, the orthodontic-specific guidelines are minimal. As a result of this lack of information and the perceived risks, many orthodontists are apprehensive about treating patients who take bisphosphonates.
With many postmenopausal women seeking orthodontic therapy, some of whom have been treated for osteoporosis with bisphosphonates, it is important to investigate the treatment outcomes and risks of osteonecrosis of the jaws in this population. The purposes of this retrospective study are to describe bisphosphonate use among an orthodontic population of older women and to determine the extent to which bisphosphonate therapy predisposes them to poor orthodontic outcomes, as measured by incomplete space closure, prolonged treatment time, nonparallel roots, incisor malalignment, and osteonecrosis of the jaws.
Material and methods
In this study, we used a retrospective cohort design, with orthodontist survey responses and data collected via chart reviews of women over age 50 who had received orthodontic treatment. The study was approved by the institutional review board at the University of Washington in Seattle.
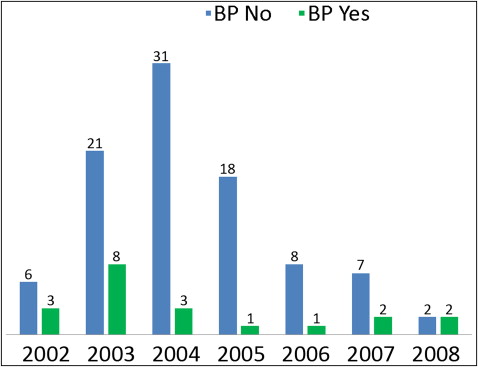
Using the 2010 American Association of Orthodontists member directory, we sent a letter of invitation by e-mail to all 249 orthodontists in Washington state with a valid e-mail address on file, requesting their participation in this project. They were informed of the nature of the study and asked to indicate approximately how many women over age 50 they start in a typical year (<3, 3-10, or >10) and to estimate the percentage of this patient group they believed were taking bisphosphonate medications (<10%, 10%-30%, or >30%). After 3 rounds of requests, responders were then asked whether they would be willing to participate in collecting specific data for female patients aged 50 and older who had started treatment in their offices from 2002 through 2008. The rationale for selecting this time frame was due to the findings of the Women’s Health Initiative in 2002, which prompted an increase in the rate of bisphosphonate use for the treatment of osteoporosis with a concurrent decrease in hormone replacement therapy. Similarly, selecting patients aged 50 and older targeted the mean onset age of menopause, when bisphosphonates are likely to be prescribed to address the increased risk of osteoporosis. Thus, the inclusion criterion for this study was female patients over age 50, treated from 2002 through 2008.
A questionnaire was designed to collect specific pretreatment information, treatment history, medical history, and defined outcome measures from the orthodontists for their patients ( Appendix 1 ). The pretreatment condition information included the patient’s age at the start of treatment, overbite, overjet, and molar classification. In addition to treatment start and end dates, pertinent treatment history information included the use of adjunct procedures such as extractions, surgery, temporary anchorage devicess, and removable aligners. Osteonecrosis of the jaws, defined as exposed bone in the maxillofacial region that has persisted for more than 8 weeks, was also queried. The medical history portion of the form asked for medications that the patient had taken, such as bisphosphonates, as well as their dosages and durations, if known. Finally, the questionnaire asked the orthodontist to evaluate the final records for incisor interproximal contact point discrepancies greater than 1 mm, open interproximal contacts, and roots adjacent to extraction sites that were angled greater than 20° from ideal. A transparent overlay was designed to facilitate assessment of the roots ( Appendix 2 ).
Hard-copy questionnaires were mailed to the orthodontists who agreed to participate. They were asked to begin with records from 2002 and search forward for all women over age 50 with a history of bisphosphonate use. A questionnaire was completed for each of these patients. The orthodontists were then asked to review consecutive female patients’ charts from the time of the first bisphosphonate patient who fulfilled the inclusion criteria until 20 total patients per office had been compiled, or the end of the study’s time frame was reached.
A priori power analyses based on 80% power were conducted with the assumption that approximately 10% of the patients enrolled would have a history of bisphosphonate use. Since experimental data were lacking to provide estimates of the prevalence of several parameters to be examined, it was estimated that 10% of the controls would have incomplete space closure, poor root parallelism, and poor incisor alignment, compared with 40% of the exposed group. By using these parameters, as well as a type I error equal to 0.05, it was determined that a sample size of 14 subjects was needed. Similarly, to detect an expected difference in treatment time of 6 months, a minimum of 10 subjects was required. Due to the rarity of bisphosphonate-related osteonecrosis of the jaws, we did not expect to achieve an adequate sample size to detect differences with respect to this condition.
Data were entered into an Excel spreadsheet (version 2007; Microsoft, Redmond, Wash) and then exported into SPSS software (version 19; IBM, Armonk, NY) for statistical analysis. Descriptive statistics for the patients with a history of bisphosphonate use and those without it were calculated for all variables. We used t tests to assess differences in treatment times after stratifying by bisphosphonate exposure. The chi-square test or the Fisher exact test was used to determine any difficulties in obtaining incisor alignment, space closure, and root parallelism, and whether the rates of extraction or osteonecrosis of the jaws were statistically different for those who had taken bisphosphonates vs those who did not. For measures that were statistically different, odds ratios were calculated to provide an estimate of the increased risk associated with bisphosphonate use.
Results
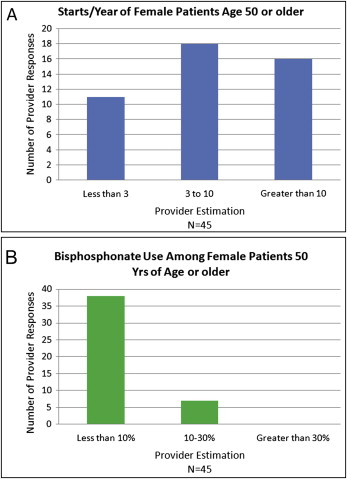
Forty-five orthodontists, of the 249 Washington state members of the American Association of Orthodontists who were contacted, responded to the initial invitation questions. When asked to estimate the number of women over age 50 they begin to treat each year, 24% of the responders answered “less than 3,” 40% replied “3 through 10,” and 36% indicated “greater than 10.” When asked to estimate the percentages of this group that have taken bisphosphonate medications, 82% of the responders answered “less than 10,” 18% replied “10 through 30,” and 0% indicated “greater than 30” ( Fig 1 ).
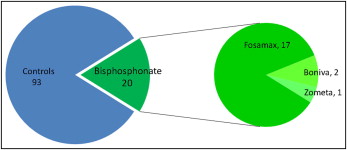
Twelve orthodontists, of the 45 who replied to the initial invitation questions, agreed to participate in the chart review process; 113 questionnaires were collected for women over 50 years of age, with 20 of these having a history of bisphosphonate use. Of these 20, 17 patients (85%) had used Fosamax, 2 (10%) had used Boniva (GlaxoSmithKline, London, United Kingdom), and 1 (5%) had used Zometa (Novartis, Basel, Switzerland). Zometa was prescribed as part of a cancer treatment regimen, whereas the remaining 19 patients took oral bisphosphonates to treat osteoporosis ( Figs 2 and 3 ). This proportion of oral vs intravenous bisphosphonate usage is similar to the proportion found is a previous large-scale study.
Pretreatment findings for the control and bisphosphonate groups were similar ( Tables I and II ). Average age for the bisphosphonate patients was 56.1 ± 4.1 years, and the average age for the control group was 55.6 ± 4.8 years. Similarly, measurements for overbite, overjet, and arch-length spacing or crowding showed no significant differences. Categorical findings—eg, proportions of Class I, Class II, and Class III patients, proportion with crossbites, and proportion of patients taking adjunct medications that might influence tooth movement—were also not significantly different between the bisphosphonate and control groups.
| Bisphosphonate use | P value | ||||
|---|---|---|---|---|---|
| No | Yes | ||||
| n | Subgroup (%) | n | Subgroup (%) | ||
| Mx arch length | |||||
| Deficient | 50 | 53.8% | 11 | 55.0% | 0.213 |
| Adequate | 32 | 34.4% | 4 | 20.0% | |
| Excess | 11 | 11.8% | 5 | 25.0% | |
| Mn arch length | |||||
| Deficient | 64 | 68.8% | 13 | 65.0% | 0.738 |
| Adequate | 24 | 25.8% | 5 | 25.0% | |
| Excess | 5 | 5.4% | 2 | 10.0% | |
| Right molar class | |||||
| Class I | 63 | 67.7% | 13 | 65.0% | 0.692 |
| Class II | 24 | 25.8% | 5 | 25.0% | |
| Class III | 5 | 5.4% | 1 | 5.0% | |
| Undeterminable | 1 | 1.1% | 1 | 5.0% | |
| Left molar class | |||||
| Class I | 61 | 65.6% | 11 | 55.0% | 0.779 |
| Class II | 26 | 28.0% | 7 | 35.0% | |
| Class III | 4 | 4.3% | 1 | 5.0% | |
| Undeterminable | 2 | 2.2% | 1 | 5.0% | |
| Crossbite | |||||
| None | 77 | 82.8% | 17 | 85.0% | 0.971 |
| Anterior | 5 | 5.4% | 1 | 5.0% | |
| Posterior | 10 | 10.8% | 2 | 10.0% | |
| Anterior and posterior | 1 | 1.1% | 0 | 0.0% | |
| NSAID use | |||||
| No | 92 | 98.9% | 20 | 100.0% | 0.641 |
| Yes | 1 | 1.1% | 0 | 0.0% | |
| Prednisone use | |||||
| No | 92 | 98.9% | 20 | 100.0% | 0.641 |
| Yes | 1 | 1.1% | 0 | 0.0% | |
| Estrogen replacement use | |||||
| No | 86 | 92.5% | 17 | 85.0% | 0.286 |
| Yes | 7 | 7.5% | 3 | 15.0% | |
| Parathyoid hormone | |||||
| No | 93 | 100.0% | 20 | 100.0% | |
| Yes | 0 | .0% | 0 | 0.0% | |
| Mx treatment type | |||||
| Comprehensive | 91 | 97.8% | 20 | 100.0% | 0.508 |
| Partial | 2 | 2.2% | 0 | 0.0% | |
| Mx appliance type | |||||
| Fixed appliances | 87 | 93.5% | 18 | 90.0% | 0.575 |
| Removable appliances | 6 | 6.5% | 2 | 10.0% | |
| Mn treatment type | |||||
| Comprehensive | 91 | 97.8% | 20 | 100.0% | 0.508 |
| Partial | 2 | 2.2% | 0 | 0.0% | |
| Mn appliance type | |||||
| Fixed appliances | 87 | 93.5% | 18 | 90.0% | 0.575 |
| Partial appliances | 6 | 6.5% | 2 | 10.0% | |
| Extractions | |||||
| No | 62 | 66.7% | 13 | 65.0% | 0.886 |
| Yes | 31 | 33.3% | 7 | 35.0% | |
| Invisalign | |||||
| No | 88 | 94.6% | 19 | 95.0% | 0.946 |
| Yes | 5 | 5.4% | 1 | 5.0% | |
| Periodontal surgery | |||||
| No | 89 | 95.7% | 20 | 100.0% | 0.345 |
| Yes | 4 | 4.3% | 0 | 0.0% | |
| TAD usage | |||||
| No | 89 | 95.7% | 18 | 90.0% | 0.302 |
| Yes | 4 | 4.3% | 2 | 10.0% | |
| Palatal expansion | |||||
| No | 92 | 98.9% | 20 | 100.0% | 0.641 |
| Yes | 1 | 1.1% | 0 | 0.0% | |
| Dental implants | |||||
| No | 88 | 94.6% | 20 | 100.0% | 0.289 |
| Yes | 5 | 5.4% | 0 | 0.0% | |
| Orthognathic surgery | |||||
| No | 85 | 91.4% | 19 | 95.0% | 0.589 |
| Yes | 8 | 8.6% | 1 | 5.0% | |
| Bisphosphonate use | P value | ||||
|---|---|---|---|---|---|
| No | Yes | ||||
| Mean | SD | Mean | SD | ||
| Patient age (y) | 55.6 | 4.8 | 56.1 | 4.1 | 0.663 |
| Overbite (mm) | 3.5 | 1.7 | 4.0 | 1.8 | 0.286 |
| Overjet (mm) | 3.1 | 1.5 | 3.2 | 1.7 | 0.865 |
| Mx ALD/E (mm) | −1.3 | 2.8 | −1.5 | 2.6 | 0.859 |
| Mn ALD/E (mm) | −2.4 | 2.2 | −2.1 | 2.3 | 0.521 |
| Predicted treatment length (mo) | 22.2 | 6.0 | 22.3 | 8.2 | 0.987 |
| Average extractions (for extraction patients) (n) | 2.70 | 1.3 | 2.4 | 1.4 | 0.626 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


