The patient was a 13-year-old Korean girl who had a displaced mandibular second premolar. She was reluctant to undergo a lengthy orthodontic treatment and opted instead for transplantation of the premolar to its usual site. On the basis of computed tomography, a replica tooth model was manufactured to shorten the extraoral time, and a root canal treatment was performed because root formation was complete. No negative signs or symptoms were found during a 3-year follow up. Autotransplantation for this patient obviated the need for orthodontic traction and prosthetic therapy.
Transposing submerged or ectopically positioned permanent teeth to their correct positions poses diagnostic as well as treatment-planning dilemmas. Although orthodontic solutions might seem to be the simplest and most successful remedies, they sometimes have unfavorable results.
After the third molars and the maxillary canines, the most commonly impacted tooth is the mandibular second premolar, with a reported impaction incidence of 2.1% to 2.7%. The frequency of intrabony distal migration for this tooth is 0.25%, and it occurs more often in females than in males. Distal displacement and intrabony migration of the mandibular second premolar are idiopathic and have been reported to occur only unilaterally. The mechanisms that cause migration of teeth are still obscure. A tooth is considered to have migrated only after its normal eruption has been prevented and it has left its normal site of development in the bone. Impaction can cause damage to the roots of neighboring teeth, and the damage can be so severe that these neighboring teeth are subsequently lost. Furthermore, the tissue around these impacted teeth might undergo cystic changes. The impaction of teeth can also lead to esthetic problems.
Orthodontic treatment options for impacted and migrated second premolars include open or closed surgical exposure and subsequent alignment, which aims to bring the tooth into occlusion. Management of this kind is both time-consuming and expensive. Attempts to rescue a deeply impacted and migrated second premolar can also cause substantial risks to the roots of adjacent teeth. Sometimes, interceptive extraction of the deciduous tooth is performed to encourage spontaneous eruption, although definitive evidence to support this procedure is still lacking. Observation and monitoring of these teeth are often performed in case they are grossly misplaced, and attempts to move or remove them could cause damage to adjacent structures. Needless to say, extraction of these teeth is often the treatment selected, whether by the recommendation of the clinician or the patient’s own choice.
On the other hand, autotransplantation, which was originally introduced in Scandinavian countries more than 40 years ago, involves atraumatic surgical removal of a tooth from its impacted or ectopic site, the creation of a socket at the donor site, and reimplantation of the tooth into the correct position in the alveolus. This procedure is generally indicated for a missing tooth with hopeless prognosis in a mouth where an appropriate donor tooth can be used without negative effects because of its loss from its position in the arch. The 3 main indications suggested by Zachrisson et al for autotransplantation of developing premolars are unevenly distributed multiple agenesis, agenesis of the mandibular second premolars in low-angle face types with normal or weak facial profiles, and accidentally lost or congenitally missing maxillary central and lateral incisors. The autotransplantation of developing premolars for replacement of missing teeth, especially the maxillary incisors, is a well-established procedure and has been demonstrated to have a high survival rate. Although the available information regarding the long-term stability of autotransplanted teeth with complete root formation is not adequate, autotransplantation is a treatment modality that has received increasing attention in recent years because of its innate advantages.
This clinical example presents the successful autotransplantation of the mandibular second premolar to its normal position by using computed tomography and a computer-aided rapid prototyping model, consequently obviating the need for orthodontic treatment.
Clinical example
The patient was a 13-year-old Korean girl with a chief complaint of an ectopic mandibular right second premolar. She was referred from a local orthodontic clinic to our hospital for interdisciplinary treatment planning. Originally, she was referred to the orthodontist from a local general dentist, who found the malpositioned permanent tooth during a routine dental examination of her retained deciduous molar with secondary caries and an apical lesion. The patient had no peculiar predental history except for the fillings in both maxillary first permanent molars. She had a retained second deciduous molar with secondary caries under a stainless steel crown. She had no orthodontic history but had good occlusion and a good facial profile. The initial panoramic radiographs ( Fig 1 ) showed that her right second permanent premolar was located deep under the root of the mandibular right first and second molars and could not be seen intraorally.

A treatment plan was established for the patient in thorough discussions between the Departments of Orthodontics, Oral and Maxillofacial Surgery, and Conservative Dentistry at Seoul National University in Korea. It was decided that the girl would not undergo orthodontic treatment for several reasons. First, her premolar was located so far from its original position and so deep in the buccal vestibule that it would be difficult to tract the tooth, although it was not impossible. In other words, traction of the premolar might harm the roots of the adjacent teeth, and the prolonged duration of the orthodontic treatment might cause considerable resorption of the tooth. Second, the patient and her parent were not enthusiastic about the potentially long duration of the orthodontic treatment since they thought that the patient already had a good profile.
For these reasons, autotransplantation was chosen for the patient as an alternative treatment plan. Because her displaced premolar showed almost complete root formation, the need for a root canal treatment and the possibility of failure for this procedure was described to the patient and her parent in detail before they gave consent.
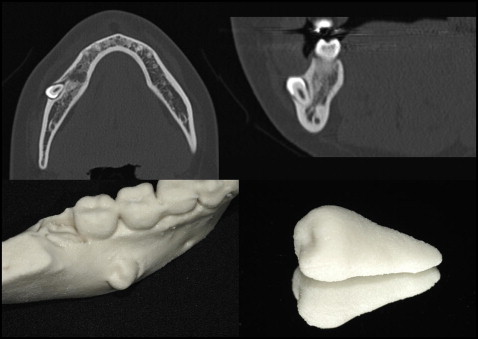
Three-dimensional computed tomography data were used to fabricate a replica graft tooth, which enhanced the preparation procedure and shortened the extraoral time of the transplant ( Fig 2 ). The computed tomography system, Somatom Sensation 10 (Siemens, Pforzheim, Germany), was used, and the 3-dimensional model was constructed by Vworks and OnDemand3D (Cybermed, Seoul, Korea). The computed tomography protocol used for this procedure involved a slit thickness of 0.5 mm. Before the autotransplantation, the deciduous second molar was extracted, and a healing period of 3 months was allowed because of the apical lesion.
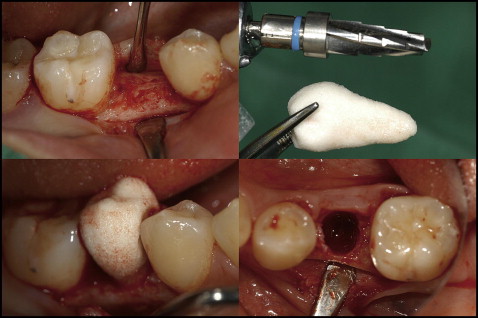
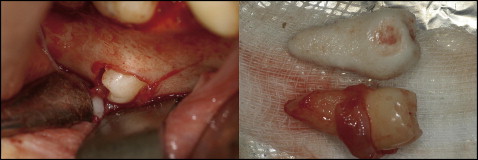
On the day of the surgery, the recipient socket was prepared with copious saline solution irrigation and surgical burs for the implant (Friadent; Dentsply, Mannheim, Germany), which was the approximate size of the replica tooth ( Fig 3 ). After confirming the recipient socket with the replica tooth, the displaced premolar was extracted carefully. The proximal surface of the extracted premolar was contoured slightly because there were interferences of the contact points of the adjacent teeth that tilted toward the extraction site. The premolar was fitted in the prepared transplantation site ( Figs 4 and 5 ). The external exposure time of the premolar was about 3 minutes. No additional bone graft was needed. Tight and close adaptation of the flaps was achieved by sutures. A surgical dressing was applied to protect the transplant against infection. The transplant was fixed with a wire and resin splint, and the occlusal interference was corrected.

Two weeks later, the root canal treatment was initiated. On the first day of the endodontic treatment, the canal was opened, cleaned, and filled with a creamy mix of calcium hydroxide spun into the canal with a lentulo spiral ( Fig 6 ). At the next visit, the canal was filled with gutta-percha and sealer after complete canal instrumentation ( Fig 7 ). Restorative treatment began 2 months after the root canal treatment. A definitive restoration was made of ceramic zirconia. During the treatment period, no specific symptoms were observed, except for pain on the day of surgery.





