This report introduces an innovative treatment approach of selecting atypical and unconventional teeth for orthodontic extraction without compromising the quality of treatment outcomes by using temporary skeletal anchorage devices in patients with bimaxillary protrusion. Both patients introduced in this report had solid Class I molar relationships with bimaxillary anterior protrusion without facial or dental midline asymmetry. Their chief concerns were significant facial convexity, which conventionally requires the extraction of all 4 first premolars. However, 3 second premolars and 1 first premolar were removed in the first patient, and 2 second premolars and 2 first premolars were removed in the second patient. All second premolars extracted had previously had root canal treatment and large prosthodontic restorations, which resulted in a compromised short lifespan of the teeth relative to the natural dentition. To manage these cases of asymmetric extraction space in a symmetric dental and skeletal environment, 2 mini-implants were placed in the posterior maxillary interradicular spaces, 1 on each side. Despite the unusual asymmetric extraction of teeth, superimposition of the pretreatment and posttreatment cephalometric tracings shows excellent treatment outcomes of facial convexity reduction by asymetric maximum retraction of the anterior teeth with no change in the molar relationships.
Extraction of teeth has been an effective method of creating space in preparation for orthodontic dental alignment and for improving intermaxillary relationships. The magnitude and vector of tooth movement as well as the biomechanical needs for anchorage preparation are primary factors to consider in the selection of teeth for extraction in various clinical situations.
Traditionally, the premolars are most frequently selected for orthodontic extraction because they are located at a site that can strategically dictate the types of anchorage preparation allowing the most efficient and effective treatment biomechanics to achieve the treatment goals. Briefly, conventional anchorage values are determined by the number of teeth or the total root surface surrounded by the alveolar bone in 1 unit pulling against another unit. Its values relative to the extraction site can affect the differential tooth movement during active orthodontic treatment, which determines the quality of the final treatment outcome. Therefore, the decision for orthodontic extraction between the first and second premolars can be critical in defining the most efficient biomechanics in conventional orthodontic treatment.
For example, the maxillary and mandibular first premolars are commonly extracted to reduce facial convexity while maintaining Class I molar and canine relationships in a Class I bimaxillary malocclusion. Unless there are preexisting conditions, such as severe dental midline deviation or asymmetric molar relationships, asymmetric extraction of premolars is often discouraged to avoid complex orthodontic biomechanics that might jeopardize the ideal treatment outcome in conventional orthodontic treatment. Therefore, the conventional orthodontic biomechanical concerns are often placed at the top of the list, rather than the general health or expected lifespan of the teeth when it comes to selection of the teeth to be extracted.
The advent of temporary skeletal anchorage devices (TSADs) such as mini-implants and mini-screws has, however, significantly simplified orthodontic biomechanics by providing independent absolute anchorage rather than the conventional active-reactive type of anchorage between dental units. Consequently, the concept of absolute anchorage has reduced the need for symmetric orthodontic extractions primarily based on the need to ease orthodontic tooth movements ( Fig 1 ). Hence, clinicians now have the freedom to determine extraction patterns not primarily based on the need for orthodontic biomechanics but on the general heath of the teeth without compromising the quality of the final treatment outcome or complicating the biomechanics during active treatment. Therefore, adverse preexisting dental conditions such as periapical lesions, root resorptions, abnormal tooth shapes, or poor periodontal conditions are important factors to consider in the selection of teeth for orthodontic extractions.
In this report, we present 2 patients with Class I bimaxillary anterior protrusion with no dental and facial asymmetry who were successfully and efficiently treated by asymmetric tooth extractions and asymmetric maximum retraction of the anterior teeth by using TSADs to obtain symmetric Class I molar and canine relationships with optimal overjet and overbite as the final treatment outcomes.
Patient 1
A 23-year-old woman’s chief complaint was severe facial convexity. Her clinical and radiographic examinations showed that she had a solid Class I molar relationship on both sides in a mild Class II skeletal pattern with no dental or facial asymmetry ( Figs 2 and 3 ). Not surprisingly, the primary treatment goal was maximum retraction of the anterior teeth to reduce lip protrusion, which traditionally requires orthodontic extraction of the 4 first premolars to create enough space for retraction of the anterior teeth.

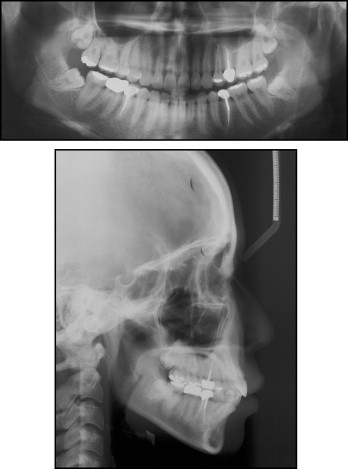
However, when a periapical radiolucency of the maxillary left second premolar raised a suspicion of a periapical lesion of the tooth ( Fig 3 , A ), an endodontist was consulted, who confirmed a recurrent periapical lesion of the tooth. Hence, we immediately adjusted the final treatment plan to extract the 3 second premolars that had endodontic treatment and 1 maxillary right first premolar to achieve better long-term stability of her general dental health.
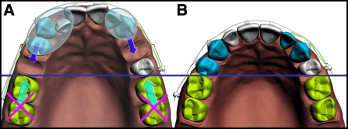
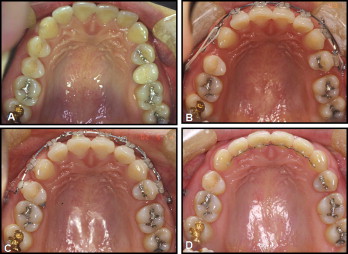
An orthodontic mini-implant (C-implant, Cimplant, Seoul, Korea) was placed on each side of the maxillary posterior interradicular space, and the patient was sent for extraction of the teeth mentioned above. Approximately 4 weeks after placement of the mini-implants, fixed orthodontic appliances were placed on all teeth except the maxillary molars to retain the pretreatment Class I molar relationship. Initially, to relieve maxillary anterior crowding, the maxillary right canine and left first premolar were retracted with a sliding jig and intra-arch rubber bands against the skeletal anchorage derived from the C-implants ( Fig 4 , A-C ). After leveling and aligning the maxillary anterior teeth, all 7 maxillary anterior teeth were retracted en-masse against the mini-implants ( Fig 4 , D-F ).
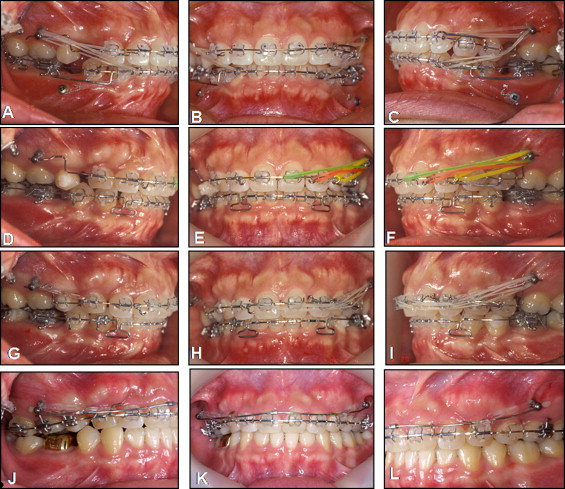
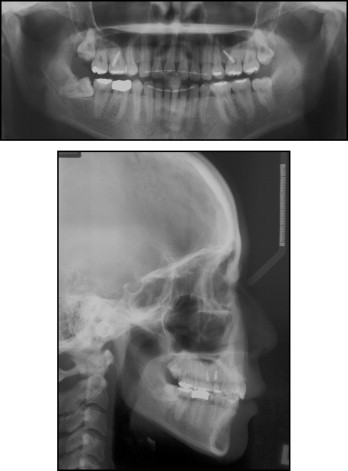
As expected, the maxillary dental midline started to shift to the right side during the early stages of treatment. This was immediately and efficiently corrected by using differential strengths of retraction on each side ( Fig 4 , G-I ). The maxillary molars were engaged with fixed orthodontic appliances only during the final stage of the treatment to fine-tune the maxillomandibular molar relationship ( Fig 4 , J-L ). Approximately 18 months into active treatment, the patient’s facial profile had significantly improved, and the dental occlusion was maintained as a symmetric Class I molar and canine relationship on both sides with optimal overjet and overbite ( Figs 5-7 ). Superimposition of the pretreatment and posttreatment cephalometric tracings also confirmed the maximum retraction of the anterior teeth in a manner of controlled tipping with no positional change of the maxillary molars in any direction ( Fig 8 , Table ).


| Average (female) ∗ | Patient1 | Patient 2 | |||
|---|---|---|---|---|---|
| PreTx | PostTx | PreTx | PostTx | ||
| SNA (°) | 81.6 | 82.0 | 81.9 | 82.0 | 81.8 |
| SNB (°) | 79.2 | 77.7 | 76.6 | 78.0 | 76.9 |
| ANB (°) | 2.4 | 4.3 | 5.3 | 4.1 | 4.9 |
| PFH/AFH (%) | 66.8 | 63.7 | 62.4 | 61.6 | 61.5 |
| SN-OP (°) | 17.9 | 23.7 | 24.6 | 22.2 | 25.8 |
| FH-U1 (°) | 116.0 | 108.6 | 90.3 | 104.2 | 94.2 |
| FMA (°) | 24.3 | 27.9 | 29.1 | 36.0 | 36.0 |
| IMPA (°) | 95.9 | 99.9 | 88.3 | 88.9 | 82.4 |
| FMIA (°) | 59.8 | 52.2 | 62.6 | 55.1 | 61.6 |
| UL-E plane (mm) | −0.9 | 2.7 | 1.4 | −0.4 | −0.6 |
| LL-E plane (mm) | 0.6 | 3.0 | −0.1 | 0.8 | 0.1 |
| Interincisal angle (°) | 123.8 | 123.6 | 152.4 | 130.8 | 147.4 |
| Mx 1 to NA (mm) | 7.3 | 3.5 | 1.8 | 3.6 | 0.7 |
| Mx 1 to NA (°) | 25.3 | 17.3 | −0.8 | 17.4 | 7.6 |
| Mn 1 to NB (mm) | 7.9 | 7.2 | 3.4 | 6.7 | 5.2 |
| Mn 1 to NB (°) | 28.4 | 34.8 | 23.2 | 27.7 | 20.1 |
| SN to PP (°) | 10.2 | 9.6 | 9.5 | 8.1 | 10.5 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


