Dentoalveolar ankylosis interferes with the vertical growth of the alveolar process, which can lead to an open bite, an unesthetic smile, and occlusal disharmony. This case report presents a new treatment protocol for an ankylosed tooth with severe root resorption using a combined surgical orthodontic management protocol involving a single-tooth dento-osseous osteotomy and vertical alveolar distraction osteogenesis with intraoral elastics and mini-implant anchorage. After distraction and active orthodontic treatment, the patient’s anterior open bite was corrected. A Class I dental relationship was achieved, overjet was decreased, and a normal incisor relationship was obtained.
Highlights
- •
A new treatment protocol for an ankylosed tooth with severe root resorption is presented.
- •
Distraction with elastics and mini-implant anchorage provided successful treatment results.
- •
The akylosed tooth with severe root resorption was kept in place during distraction.
- •
Ideal position of the ankylosed tooth in the arch was achieved.
- •
The patient’s esthetic needs were satisfied before adulthood.
Severe luxation injuries such as avulsion or intrusion can cause dentoalveolar ankylosis, which is a fusion of the alveolar bone and root surface. In experimental studies, resorption of the root with replacement by bone (replacement resorption) is elicited when the entire periodontal ligament is removed before replantation or after extensive drying of the tooth before replantation. The speed of resorption seems to depend on the patient’s metabolism.
The growth of the alveolar process depends on continuous eruption of the teeth. Dentoalveolar ankylosis interferes with the vertical growth of the alveolar process ; this can lead to an open bite, an unesthetic smile, and occlusal disharmony. To overcome the difficulties of ankylosed tooth treatment, surgical block osteotomies that allow rapid movement of a tooth or teeth in a block of bone followed by distraction osteogenesis have been reported.
Distraction osteogenesis is a method developed for newly formed bone tissue between 2 segments of a bone that is obtained by slow and gradual traction force followed by surgical osteotomy. Gradual and controlled displacement of a bone segment can be obtained with the use of force vectors in desired directions without extensive surgical interventions. In the distraction process, there are 3 fundamental sequential phases. The latency phase, during which soft callus is formed, is the period between the surgical osteotomy and the beginning of traction. It is expressed between 0 and 7 days and coincides with the initial events of the normal bone repair process. In the distraction phase, slow and gradual traction force is applied to the transport bone segment, and the formation of new immature woven and parallel-fibered bone commences. This phase usually lasts 1 to 2 weeks, and the traction modifies the normal development of the regeneration process. The consolidation phase begins after the desired correction has been achieved; this period allows for maturation of the regenerate and corticalization of the newly formed bone.
In 1996, Chin and Toth reported the first clinical application of vertical mandibular alveolar distraction osteogenesis. In 2001, Isaacson et al introduced an approach with surgical block osteotomy and distraction osteogenesis to reposition an ankylosed tooth at the proper vertical position in the arch. The advantage of this approach was that both the incisal edge and the gingival margin of the clinical crown of the ankylosed tooth could be repositioned at the proper height in the arch relative to adjacent teeth. After the clinical introduction of alveolar distraction, the use of the technique, as well as the number of available devices, has increased. These devices can be classified as tooth-borne, bone-borne, and hybrid based on their fixation points.
In some reports of treatment of an ankylosed tooth using distraction osteogenesis, distraction force was applied directly through the ankylosed tooth crown during alveolar distraction by tooth-borne distraction devices or brackets. However, if the root resorption of the ankylosed tooth is severe, then the distraction force applied can cause horizontal fracture through the cementoenamel junction. Bone-borne distractors, which are alternative devices for force application, provide successful treatment outcomes; however, these are expensive and bulky, and they require a second surgery for their removal, thus decreasing patient acceptance. To improve treatment results, satisfy patients’ esthetic needs, and overcome the difficulties of treatment of ankylosed teeth with severe tooth resorption, the use of new treatment protocols has increased. This case report describes a new treatment protocol for an ankylosed tooth with severe root resorption using a combined surgical orthodontic management protocol involving a single tooth dento-osseous osteotomy and vertical alveolar distraction osteogenesis with intraoral elastics and mini-implant anchorage.
Diagnosis and etiology
A 15-year-old boy was referred to the Department of Orthodontics at Süleyman Demirel University in Isparta, Turkey, with the complaint of an open bite and a gray malpositioned tooth of undesirable appearance. His trauma history showed that he had tripped over his own feet and fallen on his face 5 years previously. His maxillary right central incisor had been avulsed of its socket during the accident and reimplanted within 2 hours, after being kept in a dry condition. One month later, pulp necrosis had been diagnosed, and endodontic treatment was performed by a private dentist.
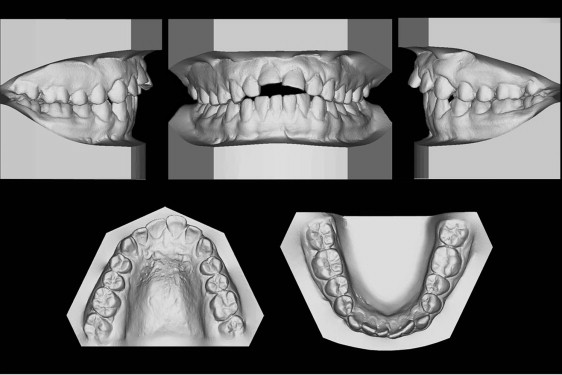
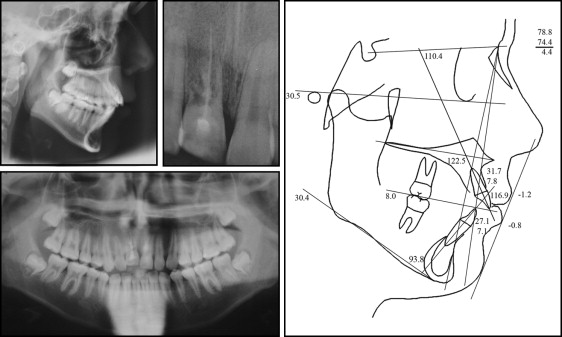
The intraoral examination showed a severely ankylosed maxillary right central incisor that was displaced 5 mm apically relative to the adjacent lateral incisor. Additionally, a Class I relationship in the molars and a Class II relationship in the canines, an increased overjet of 5 mm, and an open bite as a result of vertical alveolar growth failure, enamel fracture of the adjacent central incisor, and tilting of the adjacent teeth were diagnosed ( Figs 1 and 2 ). The ankylosed tooth was clinically asymptomatic and had no sensitivity to percussion and palpation. A metallic sound upon percussion, lack of normal mobility, and discoloration accompanying root resorption were noted. Upon radiographic examination, we found that root lengths and bone heights were normal, except around the ankylosed tooth. A periapical radiograph showed absence of the periodontal space and ongoing replacement resorption of the ankylosed tooth with external root resorption, which had been endodontically treated. External root resorption on the entire distal side of the root and around the root canal filling material was notable. Additional diagnosis included a skeletal Class I malocclusion with the following cephalometric values: SNA, 78.4°; SNB, 74.4°; and ANB, 4.4°. Vertical height was in the normal range (GoGn-SN, 30.4°) ( Fig 3 ).

Treatment objectives
Our treatment objectives were to (1) correct the anterior open bite by extrusion of the maxillary anterior teeth, (2) achieve a Class I dental relationship in the canines, (3) decrease the overjet, (4) obtain a normal incisor relationship, and (5) improve the anterior esthetics by correcting the alveolar, gingival, and incisal margins in the maxillary anterior region.
Treatment objectives
Our treatment objectives were to (1) correct the anterior open bite by extrusion of the maxillary anterior teeth, (2) achieve a Class I dental relationship in the canines, (3) decrease the overjet, (4) obtain a normal incisor relationship, and (5) improve the anterior esthetics by correcting the alveolar, gingival, and incisal margins in the maxillary anterior region.
Treatment alternatives
The 15-year-old patient’s chief complaint was an anterior open bite with a gray malpositioned tooth with a poor appearance. The advantages and disadvantages of alternative treatment methods for an ankylosed tooth were discussed with the patient.
In consideration of his age and continued vertical alveolar growth, the following alterative treatment methods were presented.
- 1.
Surgical resection of the ankylosed tooth and augmentation of the alveolar ridge followed by bridge restoration or dental implant replacement after growth were eliminated as options because of the patient’s esthetic expectations.
- 2.
Space closure through orthodontic tooth movement could have been a treatment choice; however, the patient had a good Class I dental relationship without crowding.
- 3.
Decoronation and esthetic space maintenance were rejected because of increased local arrest of alveolar bone development and possible surgical intervention related to age.
- 4.
Surgical luxation to attempt to break the fusion between the cementum and bone was not acceptable because of severe root resorption, since fracture through the cementoenamel junction of the ankylosed tooth during luxation would have been inevitable, and the tooth might have reankylosed during repair after application of an orthodontic force.
- 5.
Surgical block osteotomy to allow rapid movement of the tooth with a block of bone followed by distraction osteogenesis was preferred to provide long-lasting benefits, but distraction force applied through the crown of the ankylosed tooth during osteogenesis might have caused a fractured crown due to severe resorption of the ankylosed tooth, instead of increasing alveolar height. To modify the site of force application, placement of an orthodontic mini-implant in the center of the bone block was considered possible, and since the root resorption of the ankylosed tooth was so severe, there was adequate bone to place a mini-implant.
- 6.
A combined surgical-orthodontic management protocol involving single-tooth dento-osseous osteotomy and vertical alveolar distraction osteogenesis with intraoral elastics and mini-implant anchorage was presented as an alternative treatment method. The patient and his parents were forewarned of the potential risk of ankylosed tooth crown fracture during treatment. After discussing the treatment alternatives, the patient chose this option.
Treatment progress
During the first session, the root canal filling material was removed using K-files, and the canal was then gently irrigated with 2.5% sodium hypochlorite with a 27-gauge needle with simultaneous aspiration to prevent accidental injection of hypochlorite into the periodontal tissues. MTA (Gray Pro Root; Maillefer, Ballaigues, Switzerland) was placed in the root canal with slight pressure with the aid of an amalgam carrier, and Schilder Pluggers (Dentsply-Maillefer, Ballaigues, Switzerland) were used to seal the resorption area. After placement of the MTA, a cotton pellet soaked in saline solution was placed to stimulate material setting, and the cavity was sealed with temporary restorative material. MTA setting was checked after 24 hours, and the coronal opening on the palatal aspect was restored with light-cured resin ( Fig 4 ).

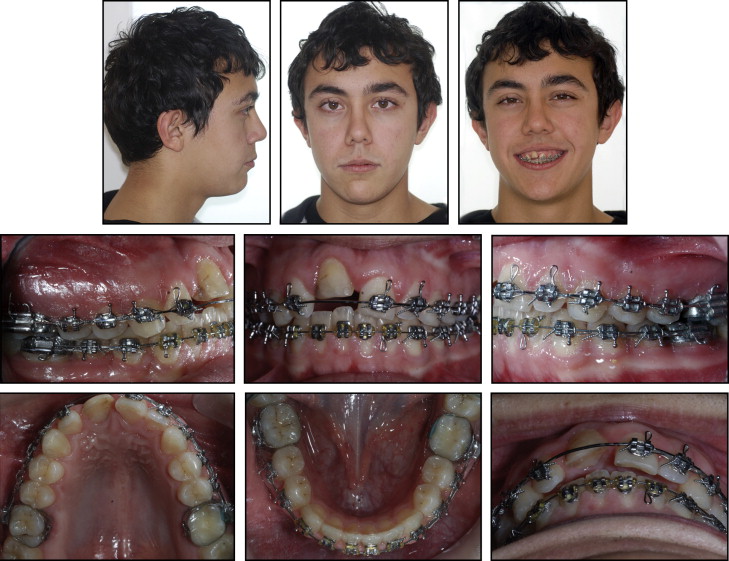
The orthodontic treatment of leveling and aligning the maxillary and mandibular dental arches was performed before surgery. Fixed preadjusted edgewise brackets with 0.018 × 0.025-in slots were applied to all maxillary and mandibular teeth except the maxillary right central incisor, with bands on the maxillary and mandibular first molars. Leveling was performed with 0.014-in and 0.016-in round nickel-titanium archwires, and then 0.018-in stainless steel round archwires. High-pull headgear was used for maxillary molar anchorage. Lace-back ligatures were used for space closure in the maxillary posterior segment. Therefore, the patient’s Class II canine relationship and increased overjet were eliminated. After alignment of both dental arches, an open-coil spring was used to create adequate space between the roots of the maxillary right lateral incisor and the right and left central incisors for interdental osteotomies. In the final stage, 0.016 × 0.022-in stainless steel rectangular archwires bypassing the maxillary right central incisor were applied. A force vector that would allow the desired vertical movement of the bone block during the distraction process was planned. The mandibular anterior segment teeth and a mini-implant to be placed between the mandibular right lateral incisor and the right canine were selected as beneficial locations for intermaxillary elastic applications. Because of the increased stability of the mandibular arch during distraction, the mandibular dental arch was strengthened by using a figure-8 ligature on and cinching back the 0.016 × 0.022-in stainless steel rectangular archwire. To identify the ideal vertical level of the central incisors, the fractured maxillary left central incisor was restored with composite resin before surgery. After ensuring sufficient space for surgery, presurgery radiographs, photographs, and dental casts were collected. ( Figs 5-7 ).
A single-tooth osteotomy was performed under local anesthesia ( Fig 8 ). A full-thickness mucoperiosteal flap was reflected to expose the alveolar bone around the ankylosed tooth. A subapical osteotomy line was positioned horizontally, 4 mm above the virtual root apex. Two vertical interdental osteotomies (diverged coronally) were placed, one between the maxillary left lateral and left central incisors, and one between the left central and right central incisors. After guide groove drilling by a 0.7-mm-diameter carbide dental bur (ELA, Engelskirchen, Germany), osteotomy cuts were deepened with a microsagittal saw (Micro-Saw System; ACE Surgical Supply, Brockton, Mass) and completed with medium osteotomes. Next, the bone-block unit containing the ankylosed incisor was controlled and mobilized. During the cutting procedure, great care was taken not to injure the palatal mucosa, periosteum, and adjacent teeth. A self-tapping mini-implant (diameter, 2 mm; length, 8 mm) (Dual-top Anchor System 20-G2-010; Guro-Gu, Seoul, Korea) was placed in the center of the ankylosed tooth-supporting bone with predrilling after mobilization. During insertion, the tooth-supporting bone-block unit was supported manually from the palatal side. The mucoperiosteal flap was then closed and sutured with 3/0 silk (Doğsan, Istanbul, Turkey) ( Fig 8 ). Mini-implant placement was performed under radiographic control.




