This article describes a multidisciplinary approach to a functional and aesthetic rehabilitation. In this case study, we successfully corrected an anterior open bite and an exaggerated curve of Spee using restorative modalities while still maintaining a highly aesthetic outcome. The maxillary anterior teeth no longer appear to have a disproportional width/length ratio and are now in harmony with the mandibular veneers. Posterior function was re-established, mostly with implant-retained crowns. Occlusal harmony and stability are maintained through cuspid guidance and anterior disclusion. Proper selection of final restorative materials is imperative for the long-term survival of the restorations.
Key points
- •
Gain an appreciation for the complexity of multidisciplinary treatment.
- •
Realize the indispensable utility of the New York University Smile Evaluation Form.
- •
Appreciate that an understanding of material properties is critical for long-term success.
Patient background and chief concern
A 48-year-old male owner of a hair salon presented with the chief concern of long, thin, and unaesthetic anterior crowns that hindered his ability to comfortably chew, as a result of several missing posterior teeth. The patient’s expectations were to receive a smile makeover and posterior implants that would allow him to function better. He requested a treatment that avoided any orthodontic solutions.
His medical history was unremarkable and noncontributory; thorough extraoral and intraoral examination ruled out any abnormalities of the temporomandibular joint and its associated muscles as well as occlusal disharmonies and parafunctional habits. He had significant dental history that included extensive past fixed prosthodontic and restorative/endodontic therapy.
Clinical examination revealed general failure of restorations throughout the dentition. Teeth numbers 6 to 11 were previously restored with all-ceramic full-coverage restorations.
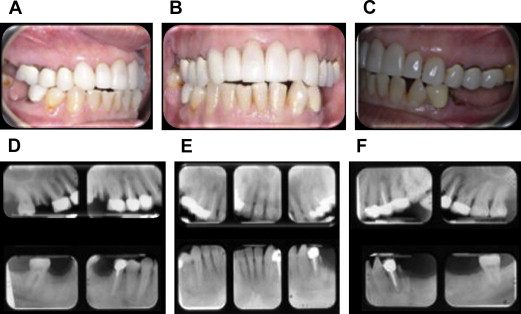
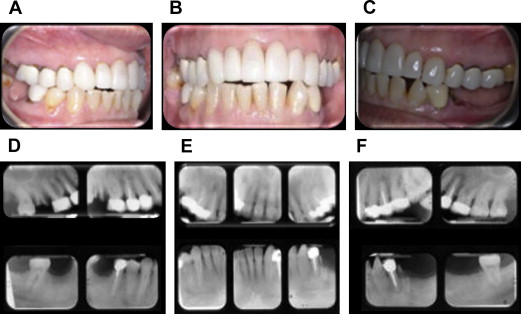
Teeth numbers 3, 4, 5, 12, 13, 14, 21, and 29 had existing porcelain fused to metal (PFM) crowns. The natural dentition of the mandibular anterior region showed rotation and unevenness with a diastema between teeth numbers 22 and 27. On full smile, there was a significant shade difference between the lower and upper arches. The periodontal condition was satisfactory, with probing depths ranging from 1 to 4 mm throughout the maxilla and mandible. Radiographic analysis showed generalized mild horizontal bone loss. No vertical defects, mobility, or fremitus were noted ( Fig. 1 ).
A clinical diagnosis was formulated for this patient that included:
- •
Caries
- •
Missing and broken teeth with some loss of function
- •
Generalized mild periodontal disease accompanied by posterior tooth loss
- •
Right canine class II malocclusion with an anterior open bite
- •
Moderate crowding in the mandible
- •
Recurrent lesions around previously endodontically treated teeth with symptomatic apical periodontitis
- •
Unaesthetic, failing crowns with a significant shade discrepancy from the remaining natural dentition
The goals of the treatment were to control the factors that caused the disease and to restore the deformities that the disease process caused, while achieving an aesthetic outcome acceptable to the patient. A multidisciplinary approach involving fixed prosthetic, periodontal restorative and endodontic therapies was essential to achieving the desired outcome ( Fig. 2 A–F).
Patient background and chief concern
A 48-year-old male owner of a hair salon presented with the chief concern of long, thin, and unaesthetic anterior crowns that hindered his ability to comfortably chew, as a result of several missing posterior teeth. The patient’s expectations were to receive a smile makeover and posterior implants that would allow him to function better. He requested a treatment that avoided any orthodontic solutions.
His medical history was unremarkable and noncontributory; thorough extraoral and intraoral examination ruled out any abnormalities of the temporomandibular joint and its associated muscles as well as occlusal disharmonies and parafunctional habits. He had significant dental history that included extensive past fixed prosthodontic and restorative/endodontic therapy.
Clinical examination revealed general failure of restorations throughout the dentition. Teeth numbers 6 to 11 were previously restored with all-ceramic full-coverage restorations.
Teeth numbers 3, 4, 5, 12, 13, 14, 21, and 29 had existing porcelain fused to metal (PFM) crowns. The natural dentition of the mandibular anterior region showed rotation and unevenness with a diastema between teeth numbers 22 and 27. On full smile, there was a significant shade difference between the lower and upper arches. The periodontal condition was satisfactory, with probing depths ranging from 1 to 4 mm throughout the maxilla and mandible. Radiographic analysis showed generalized mild horizontal bone loss. No vertical defects, mobility, or fremitus were noted ( Fig. 1 ).
A clinical diagnosis was formulated for this patient that included:
- •
Caries
- •
Missing and broken teeth with some loss of function
- •
Generalized mild periodontal disease accompanied by posterior tooth loss
- •
Right canine class II malocclusion with an anterior open bite
- •
Moderate crowding in the mandible
- •
Recurrent lesions around previously endodontically treated teeth with symptomatic apical periodontitis
- •
Unaesthetic, failing crowns with a significant shade discrepancy from the remaining natural dentition
The goals of the treatment were to control the factors that caused the disease and to restore the deformities that the disease process caused, while achieving an aesthetic outcome acceptable to the patient. A multidisciplinary approach involving fixed prosthetic, periodontal restorative and endodontic therapies was essential to achieving the desired outcome ( Fig. 2 A–F).
Smile evaluation
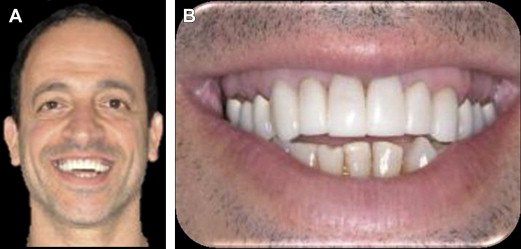
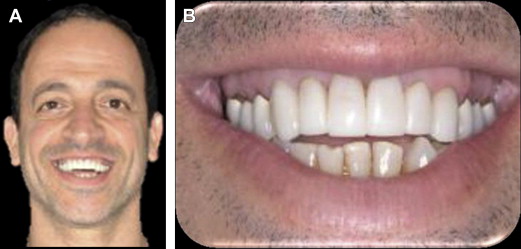
Pretreatment smile analysis is even more important in patients who have already undergone treatment within the aesthetic zone ( Fig. 3 ).


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


