(1)
Department of Pathology, Radboud University Nijmegen Medical Center, Nijmegen, The Netherlands
Abstract
Tooth alterations occurring after eruption in the oral cavity are manifold. They may be due to a large variety of causes. Their effect may be gross form alterations or subtle changes being only visible on histologic examination.
Tooth alterations occurring after eruption in the oral cavity are manifold. They may be due to a large variety of causes. Their effect may be gross form alterations or subtle changes being only visible on histologic examination.
Caries
Tooth decay (dental caries) starts with the destruction of the enamel cap by microorganisms present in the oral cavity and adherent to the tooth surface. This leads to exposure of the underlying dentin to the oral environment and to its destruction by bacterial proteolytic enzymes. Enamel caries will not be visible in routinely prepared histologic sections as this tissue dissolves completely during decalcification. In ground sections made from undecalcified teeth, microscopic examination under transmitted light will reveal optical alterations related with decreased mineral content of a still intact crystalline structure. These alterations tend to occur over a cone-shaped area having its base on the surface and its point towards the amelo-dentinal junction (Fig. 6.1). With increasing loss of minerals from the enamel structure, this tissue will disintegrate. Sometimes, this destroyed enamel will contain so much organic material that it is still present in decalcified sections where it is visible as a basophilic amorphous mass.
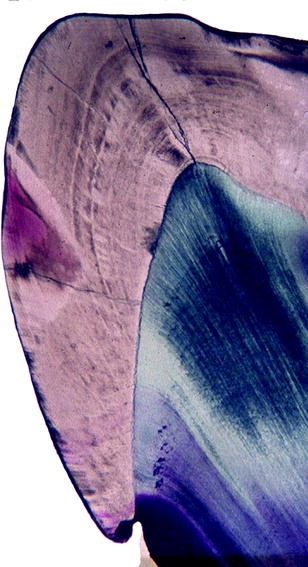
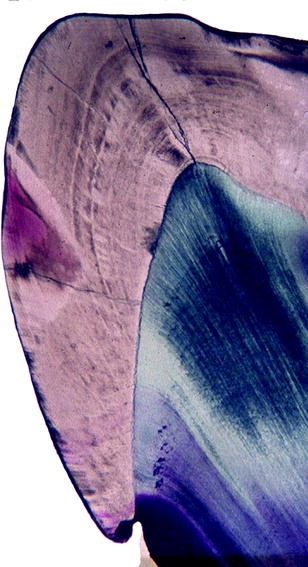
Fig. 6.1
Ground section showing wedge-shaped discoloration in enamel due to alterations in optical properties of enamel as a result of loss of calcium while still preserving the crystalline scaffold
The initial carious lesion in dentin afflicts the tubuli that serve as a highway for bacteria to spread into the dentin. As the tubules of the carious dentin become more distended due to breakdown of their walls by the proteolytic enzymes excreted by the invading bacteria, they may fuse and form spindle-shaped cavities perpendicular to the tubules. Fusion of afflicted tubules over a longer distance may also create spindle-shaped cavities in the same direction as the tubuli run. Through the continued loss of dentin between the tubules, its inner structure crumbles away (Fig. 6.2a–d). When caries is not halted by dental treatment, bacteria and their toxic products will reach the soft inner part of the tooth, the dental pulp, and evoke an inflammatory response, pulpitis, to be discussed later on (see Sect. “Pulpitis”). Subsequently, the pulp dies and toxic substances from the pulp space diffuse through the apical foramen into the adjacent periapical part of the periodontal ligament and surrounding jaw bone. Periapical disease will now ensue. If the root surface of a tooth is exposed due to periodontal disease (see Chap. 9), the root covering caries may also be the victim of carious decay. At this site, the bacteria penetrate into the cementum using the collagen fibres that once anchored the tooth in its tooth socket as pathways.
Fig. 6.2
Caries induced alterations in dentin and dental pulp. (a) Low-power view showing area of discoloration and disintegration. (b) Higher magnification showing also deposition of reparative dentin in the dental pulp. (c) Area of disintegration and dentin tubuli filled with bacteria extending towards the dental pulp. (d) In more advanced disintegration, transverse splits connect the widened tubuli
Attrition
Attrition is the gradual loss of dental hard tissue as a result of chewing [1]. Therefore, it only affects the tooth surfaces used in or shearing against each other during mastication: incisal for incisors and cuspids, occlusal for premolars and molars and approximal (surfaces where adjacent teeth touch each other). When the enamel cap is worn away, the underlying dentin becomes exposed. Usually this shows a dark-brown discoloration (Fig. 6.3). The dental pulp compensates for the loss of dental hard tissues by the deposition of tertiairy dentin.


Fig. 6.3
Attrition: mandibular incisor teeth with enamel worn away, thus exposing the brown discoloured dentin
Abrasion
Abrasion is due to wearing away of dental hard tissue by other causes than mastication [1]. It may be due to improper use of the dentition such as holding items between the teeth such as pipes, hairpins or other objects. The most common cause of abrasion is too vigorous toothbrushing that may cause defects at the necks of the teeth.
Erosion
Dental erosion is defined as loss of dental hard tissues due to chemical injuries other than those occurring in tooth caries [1]. Excessive intake of acid beverages or gastric reflux may cause this type of tooth damage as any solution of low pH may dissolve the enamel. In contrast to caries that causes subsurface demineralisation, erosion is a surface phenomenon. The affected teeth show smoothly outlined defects that may involve not only enamel but also the underlying dentin at areas where the enamel has disappeared (Fig. 6.4).


Fig. 6.4
Erosion: buccal surfaces of right maxillary cuspid and first premolar tooth showing loss of enamel. Both central and right lateral incisor teeth show white areas at their labial surfaces indicating incipient decalcification but still maintaining their crystalline structure
Hypercementosis
During the lifetime of the teeth, continuous apposition of cementum on the root surface causes a gradual increase of its thickness. This gradual increase in cementum may compensate for loss of tooth tissue at the occlusal surface due to physiological tooth wear, thus maintaining the length of the tooth. Sometimes, this apposition of cementum is excessive, leading to a very thick cementum layer. This condition is termed hypercementosis (Fig. 6.5). This cementum usually is of the acellular type although sometimes cellular cementum resembling bone may also occur. Hypercementosis may occur without any recognisable cause, but it can also be seen in relationship with chronic periapical inflammation. Moreover, it occurs in patients with Paget’s disease (Fig. 6.6) [2].


Fig. 6.5
Ground section showing molar tooth with carious decay and pronounced hypercementosis. Both roots are covered with a thick cementum layer, most pronounced in the apical area
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



