Introduction
The purposes of this study were to evaluate the accuracy of cone-beam computed tomography (CBCT) for detecting naturally occurring alveolar bone dehiscences and fenestrations and to find a better method to diagnose them.
Methods
The sample consisted of 122 anterior teeth in 14 patients with Class III malocclusion who accepted accelerated osteogenic orthodontic surgery in the anterior tooth region. Dehiscences and fenestrations were measured both directly, with a gauge during surgery, and indirectly, by CBCT scans collected before treatment. A Bland-Altman plot for calculating agreement between the 2 methods was used. Direct data were regarded as the gold standard, and indirect data were analyzed to evaluate the accuracy of CBCT for detecting dehiscences and fenestrations by sensitivity, specificity, positive predictive value, negative predictive value, Youden index, positive likelihood ratio, and negative likelihood ratio. Receiver operator characteristic curves were also used to determine the area under curve and the best critical points of CBCT for detecting dehiscences and fenestrations.
Results
Both the sensitivity and specificity of CBCT for dehiscences and fenestrations were over 0.7. The negative predictive values were high (dehiscence, 0.82; fenestration, 0.98), whereas the positive predictive values were relatively low (dehiscence, 0.75; fenestration, 0.16). Areas under the curve were 0.873 for dehiscences and 0.766 for fenestrations. The best critical points for detecting both dehiscences and fenestrations were 2.2 mm.
Conclusions
Our study showed that the CBCT method has some diagnostic value for detecting naturally occurring alveolar bone dehiscences and fenestrations. However, this method might overestimate the actual measurements.
Highlights
- •
Cone-beam computed tomography (CBCT) can be used to detect dehiscences.
- •
Dehiscence measurements were systematically overestimated when the vertical diameter was >3 mm.
- •
Fenestrations were also systematically overestimated.
- •
We recommend setting the critical point for fenestration on the CBCT (CPFC) at 2.2 mm and the critical point for dehiscence on the CBCT (CPDC) at 2 mm.
- •
CBCT has diagnostic value for naturally occurring alveolar bone dehiscences and fenestrations.
When the tooth root is denuded of bone and the root surface is covered only by the periosteum and the gingiva, it is called fenestration ; the denuded areas involving the alveolar margin are called dehiscences. Studies have shown that alveolar dehiscence and fenestration are common in different types of malocclusions, possibly leading to gingival recession and additional bone loss during orthodontic treatment. Therefore, it is important to detect these defects before treatment.
Since cone-beam computed tomography (CBCT) can be used to evaluate alveolar bone morphology, some studies have been conducted to examine dehiscences and fenestrations with CBCT. These studies showed a much higher prevalence than did previous skull studies (dehiscence, 0.99% to 13.4%; fenestration, 0.23% to 16.9%). However, the accuracy of a CBCT scan for detecting alveolar bone dehiscence and fenestration is doubtful.
Many authors have studied the accuracy of computed tomography and CBCT in detecting alveolar defects, but most of the defects were created by the operators. In 2010, when Leung et al evaluated the accuracy of CBCT for detection of naturally occurring alveolar dehiscences and fenestrations in human skulls, they concluded that indirect assessment of buccal alveolar bone defects overlying roots was not as accurate as was previously reported. Compared with CBCT of alveolar bone in vivo, direct assessment of dry skulls lacks the image of the paradentium; thus, it may result in system errors. Therefore, these studies might not provide sufficiently accurate CBCT images for detecting the alveolar bone defects in a living person. As yet, however, no studies have been conducted to determine the accuracy of CBCT in detecting dehiscences and fenestrations in vivo.
One aim of this study was to evaluate the accuracy of CBCT in diagnosing naturally occurring alveolar dehiscences and fenestrations in vivo. The other aim was to find a better method of diagnosing these defects by CBCT. The first hypothesis was that there is no difference in the detection of dehiscences and fenestrations with a CBCT method compared with direct assessments during accelerated osteogenic orthodontic (AOO) surgery. The second hypothesis was that some critical points of our CBCT method are more accurate than others in detecting alveolar dehiscences and fenestrations.
Material and methods
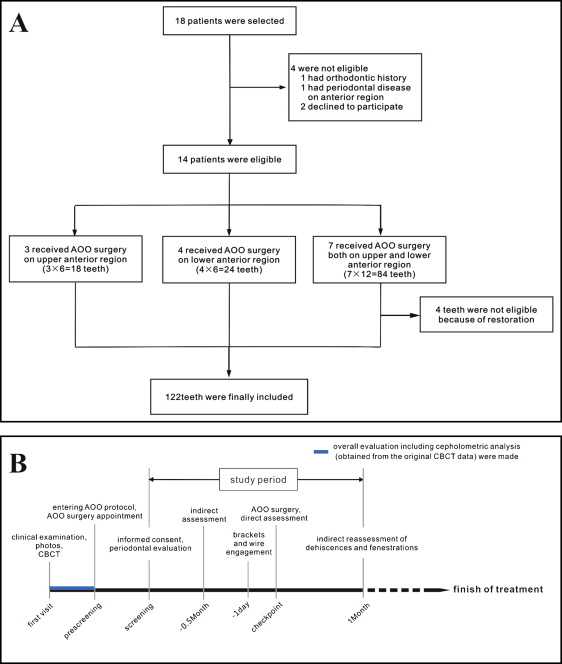
In consideration of the common existence of dehiscences and fenestrations and the large amount of decompensation during presurgical orthodontics in the anterior region of skeletal Class III patients, both orthodontists and oral surgeons made overall evaluations from CBCT images and clinical examination to determine whether AOO surgery should be used. Class III patients who were to undergo AOO surgery in the anterior region (maxillary, mandibular, or both) from June to August 2013 were selected from the Department of Oral & Cranio-Maxillofacial Science, Ninth People’s Hospital, College of Stomatology, Shanghai Jiao Tong University in Shanghai, China. Eighteen patients were selected according to the following inclusion criteria: (1) adult, (2) prepared to undergo AOO surgery, and (3) anterior crossbite. After the exclusion criteria—(1) obvious pathology (cyst or tumor in the alveolar process), (2) history of orthodontic treatment, (3) periodontal disease in the anterior region, (4) restorations on anterior teeth, and (5) defective dentition or supernumerary teeth in the anterior region—were applied, the final sample of 14 patients with 122 anterior teeth was selected ( Fig 1 , A ). The distribution of these teeth is shown in Table I . Cephalometric characteristics of the subjects are shown in Table II . Digital tracings of lateral cephalograms were performed using Nemotec Imaging software (version 6.0, Dental Studio NX 2006; Nemotec, Madrid, Spain). At the first visit, a CBCT examination was recommended if there were clinical indications such as root prominence or severe compensatory torque in the anterior region. After an overall evaluation, the AOO surgery was scheduled within a month of the first visit. Permission was obtained from all patients who participated in the study. This study was approved by the independent ethics committee of Shanghai Ninth People’s Hospital affiliated with Shanghai Jiao Tong University, School of Medicine. The timeline of events for the study is shown in Figure 1 , B .
| Male subjects | Female subjects | Total | |
|---|---|---|---|
| Maxillary central incisor | 4 | 16 | 20 |
| Maxillary lateral incisor | 3 | 16 | 19 |
| Maxillary canine | 4 | 16 | 20 |
| Mandibular central incisor | 4 | 16 | 20 |
| Mandibular lateral incisor | 3 | 18 | 21 |
| Mandibular canine | 4 | 18 | 22 |
| Total | 22 | 100 | 122 |
| Measurement | Mean ± SD |
|---|---|
| SNA (°) | 81.6 ± 4.6 |
| SNB (°) | 86.5 ± 4.5 |
| ANB (°) | −4.9 ± 3.1 |
| Wits appraisal (mm) | −12.3 ± 4.2 |
| Overbite (mm) | 0.8 ± 2.2 |
| Overjet (mm) | −2.6 ± 2.1 |
To acquire the CBCT data, each subject was scanned using a commercially available CBCT scanner (VG; NewTom, Verona, Italy) during his or her first visit. After the machine’s calibration was ascertained to be correct, the patient’s head was oriented by locating the Frankfort plane parallel to the horizontal plane and in centric occlusion. The scanning parameters for imaging were 110 kV, 0-20 mA (achieved automatically by setting the gray values at 16 bits), exposure time of 5.4 seconds, and a 12-in field of view (F mode). These settings produced a voxel size of 0.125 mm. All subjects were informed that a 0.125-mm voxel size scan might produce more radiation than a larger one (eg, 0.4-mm voxel size) and that, to reduce radiation and cost, the panoramic radiographs and lateral cephalograms were all captured from the original CBCT data. The settings were the same as those used for orthodontic diagnosis and treatment planning in the Department of Oral & Cranio-Maxillofacial Science of Shanghai Ninth People’s Hospital in China.
Raw data were reconstructed into 3-dimensional volumes and saved as DICOM files using the software from the manufacturer. Then the DICOM files were imported into integrated image-processing software (version 2.4, Kodak Dental Imaging Software 3D Module; Eastman Kodak, Rochester, NY) ( Fig 2 ).
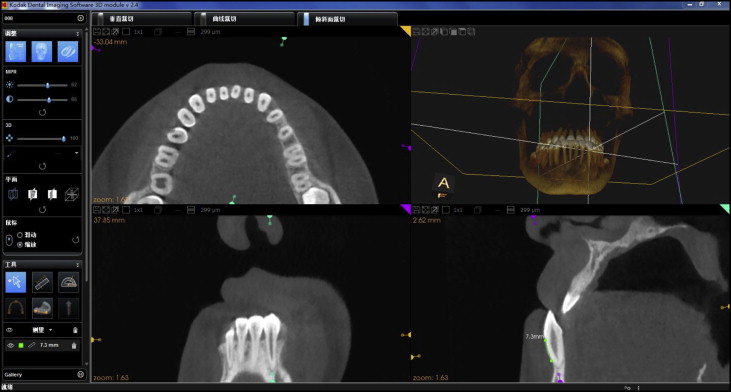
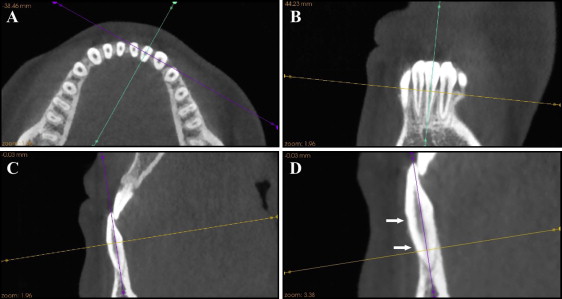
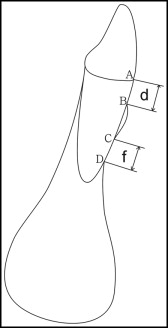
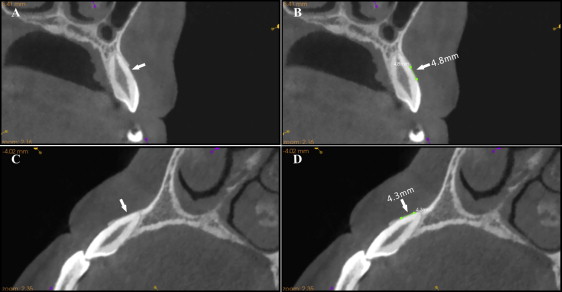
Anterior teeth that fit our criteria were chosen as the study samples, and the largest labiolingual section was defined as the measurement plane. Figure 3 illustrates the detailed procedure of locating the measurement plane. Table III gives the definitions of reference points and variables, and Figure 4 illustrates the measuring technique for the CBCT images. According to the studies of Evangelista et al and Yagci et al, we set the critical point (d C ) for dehiscence on the CBCT (CPDC) at 2 mm and the critical point (f C ) for fenestration on the CBCT (CPFC) at 0 mm. This means that when d C was more than 2 mm on the CBCT, the defect was classified as a dehiscence ( Fig 5 , A and B ); when f C was more than 0 mm on the CBCT, it was classified as a fenestration ( Fig 5 , C and D ). To limit experimental bias, dehiscences and fenestrations were reexamined on the CBCT image, the d C and the f C of all teeth were remeasured 4 weeks after the AOO surgery ( Fig 1 , B ), and the resulting mean values were used. All measurements were made by the same operator (L.S.).
| Reference points and variables | Definition |
|---|---|
| Dehiscence | Alveolar bone defect involving an alveolar margin 2 mm or greater and concurrent with a v-shaped bone margin of the alveolar crest |
| Fenestration | A circumscribed defect on the alveolar bone exposing the root, not involving the alveolar crest |
| A | CEJ at the labial side |
| B | Alveolar crest at the labial side |
| C | Coronal border of a fenestration |
| D | Apical border of a fenestration |
| d (mm) | Distance between A and B |
| d C (mm) | Distance between A and B measured by the CBCT method |
| d D (mm) | Distance between A and B measured by the caliper |
| f (mm) | Distance between C and D |
| f C (mm) | Distance between C and D measured by the CBCT method |
| f D (mm) | Distance between C and D measured by the caliper |
| CPDC (mm) | Critical point of d C for dehiscence on CBCT, the value of d C more than which the tooth was classified as dehiscence; otherwise it was considered healthy |
| CPFC (mm) | Critical point of f C for fenestration on CBCT, the value of f C more than which the tooth was classified as fenestration; otherwise it was considered healthy |
| Best CPDC | CPDC with the highest YI under which the accuracy to detect dehiscence is the highest comprehensively |
| Best CPFC | CPFC with the highest YI under which the accuracy to detect fenestration is the highest comprehensively |
To acquire the direct data, our AOO surgical procedure included bone activation and guided bone regeneration, and it was performed 1 day after the brackets and tubes were bonded. After full-thickness flaps were reflected during the surgery, the dehiscences and fenestrations were counted, and the vertical diameter parallel to the long axis of the teeth (d D and f D in Table III ) having these defects was measured directly with a vernier caliper (042-751-00; Dentaurum, Ispringen, Germany) calibrated to the nearest 0.1 mm. If d D was greater than 2 mm, it was classified as a dehiscence; if f D was greater than 0 mm, it was classified as a fenestration. All direct measurements were done twice by the same operator (L.S.), and the mean of the 2 values was used.
Statistical analysis
All statistical analyses were performed with the Statistical Package for the Social Sciences (version 16.0; SPSS, Chicago, Ill). The means, standard deviations, medians, and minimum and maximum values of d C , d D , f C , and f D were calculated. The Shapiro-Wilk test was performed to test the normality of d C , d D , f C , and f D of our sample. Bland-Altman plot analysis was applied to assess agreement between the direct and indirect methods. Categorical data (presence or absence of fenestrations and dehiscences) were analyzed using 2 × 2 tables, and the sensitivity (Se = a/[a + c]), specificity (Sp = d/[b + d]), positive and negative predictive values (PV+ = a/[a + b] and PV− = d/[c + d]), Youden index (YI = Se + Sp−1), and positive and negative likelihood ratio (LR+ = Se/[1−Sp] and LR− = [1−Se]/Sp) were calculated for both the direct and the indirect (CBCT) methods. The direct method was used as the gold standard for comparison, and the diagnostic criteria of the direct method for both dehiscences and fenestration were kept unchanged in our study. Receiver operator characteristic (ROC) curves of our CBCT method for detecting alveolar dehiscences and fenestrations were generated by paired measurements (direct and indirect). The area under curves (AUC) was calculated to evaluate the diagnostic value of the CBCT method, and the best CPDC and CPFC were determined at the highest YI (sum of Se and Sp) by considering Se and Sp as equal. The accuracy of CBCT in detecting dehiscences and fenestrations was reevaluated using the best CPDC and CPFC.
Intraoperator reliability was assessed by calculating the intraclass correlation coefficient (ICC) between measurements collected at both times. The significance level was set at a 2-tailed P value of 0.05.
Results
Table IV shows the ICC values for the vertical diameters of both dehiscences and fenestrations (4 continuous variables: d C , d D , f C , and f D ). It indicates that both the direct and the CBCT methods have excellent reliability.
| Direct | CBCT | |||||
|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | |||
| Mean ± SD (mm) | Mean ± SD (mm) | ICC | Mean ± SD (mm) | Mean ± SD (mm) | ICC | |
| d | 2.83 ± 1.84 | 2.84 ± 1.86 | 1.000 | 3.49 ± 2.80 | 3.55 ± 2.83 | 0.996 |
| f | 0.12 ± 0.52 | 0.12 ± 0.52 | 1.000 | 0.74 ± 1.41 | 0.77 ± 1.45 | 0.994 |
Table V shows the means, standard deviations, medians, and minimum and maximum values of d C , d D , f C , and f D . According to the test of normality, the d C , d D , f C , and f D of our sample were not normally distributed ( P <0.01).
| Mean ± SD (mm) | Median (mm) | Min (mm) | Max (mm) | P | |
|---|---|---|---|---|---|
| d D | 2.83 ± 1.85 | 2.0 | 0.6 | 10.0 | 0.00 ∗ |
| d C | 3.52 ± 2.81 | 2.2 | 0.6 | 12.8 | 0.00 ∗ |
| f D | 0.12 ± 0.52 | 0 | 0 | 4.0 | 0.00 ∗ |
| f C | 0.75 ± 1.43 | 0 | 0 | 5.3 | 0.00 ∗ |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


