Ridge-Pontic Relationship
Claude R. Rufenacht
In areas where missing teeth have to be replaced with fixed prosthodontics, the clinician has to face the task not only of fabricating pontics that fulfill the requirements in form, function, and esthetics of a normal tooth but also of maintaining the health of the adjacent periodontium. These requirements are usually conflicting.
The relationship of the pontic to the underlying ridge is more than complex because of the various deformities that this ridge may exhibit. The ultimate physical and anatomic form of the pontic’s recipient site results directly from the periodontal and dental state prior to the extraction and the maneuvers exerted during this procedure. Periapical and periodontal pathology, trauma, and the healing potentialities of the body are important factors in determining the future design of the pontic recipient site.
If we assume that the edentulous ridge may retain the general shape and mass of bone that existed prior to the extraction of the tooth, we will be confronted with an adequate or normal ridge. Even classified as normal, the ridge may not be normal in many respects. The eminences that existed in the bone over the root in a prominent arch position usually disappear as bone remodels during healing. The interdental papilla and the scalloped form of the marginal gingiva no longer exist and the smooth tissue surface of the edentulous ridge does not mimic the preexisting “orange peel” appearance of the gingiva.
In fixed prosthodontics a correctly placed pon’tic tooth rests on the top of a smooth tissue, lacks root prominence and marginal and interdental papillae, and does not fool a critical or simply discerning eye.
If one wishes to restore the tooth and tissue contour that existed prior to extraction, it will be impossible, even if the edentulous area is considered normal (Figs 9-1 and 9-2). Consequently, one must compromise with these restrictions and modify the environment in adopting modalities of treatment that will help to restore the previous situation.
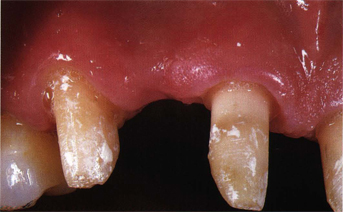
Fig 9-1 An edentulous area barely maintains the mass of bone that existed prior to the extraction.
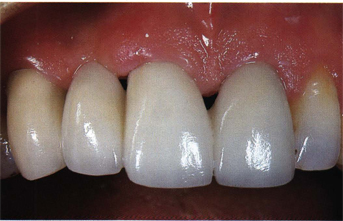
Fig 9-2 The pontic rests on a tissue from which prominences and the usual particularities marking gingival tooth relationships have disappeared. From this point a “gingivabrasion” would improve tissue color blending.
Ridge collapse consecutive to extraction may be considered inevitable. The attempt to maintain the edentulous alveolar ridge is an old concept that was applied in the last century.1 The retention of endodontically treated roots2,3 was recommended together with the submerging of vital roots.
Implants that act as fillers after extractions provide mechanical support, prevent the collapse of both labial and lingual plates of bone, and delay or diminish bone loss.1–9
Once the tooth is extracted, the soft granulation tissue, properly removed with curettes, synthetic graft material (hydroxyapatite, HA) in granules is introduced in the socket with a sterile amalgam carrier. Excess of hemorrhage is carefully sponged from the extraction site opening and the socket is filled to a level approximating the free gingival margin. If the graft material is a solid HA root, it should be placed 2 to 3 mm below the marginal crest of bone, and attention must be paid to carefully rounding its occlusal surface. At this moment the superficial part of the socket should be sealed by means of three procedures:
1. A gelatine or collagen material is applied, compressed on the area and maintained with surgical dressing.
2. Freeze-dried cadaver skin is placed over the graft and sutured. Sutures and the cadaver skin are removed 10 days postoperatively. The results of this approach seem to be stable.
3. A free gingival graft or partial-thickness flap prepared from the palatal side of the socket is placed over the implant material to assure initial healing.
Maximal preservation of the alveolar requires immediate placement of HA implants after tooth extraction. Both animal and clinical studies have proved HA to be safe and capable of retarding postextraction bone resorption.10 Control sockets after 1 year are significantly smaller than the roots or particle-filled sockets. Based on a 31-month follow-up study, it has been demonstrated that with HA implants twice as much alveolar bone was maintained than in the unimplanted control sites.11,12
Predictability of the procedure is best assured when implant material is placed into a socket provided with adequate bone support. When we respect this basic clinical principle and assure the seal of the socket over the implant, no evidence of rejective phenomenon, such as inflammation, ulceration, fistula and pain, has been stated. However, a loss of the cortical plate following extraction or periodontal disease constitutes a contraindication.
Indeed, the difficulty of preventing the possible migration of HA particles into the alveolar mucosa is coupled with the risk of tear that, affecting the thin remaining alveolar gingiva, may compromise the healing process. When facing this type of situation, the socket is best left for normal healing in the knowledge that a surgical corrective procedure can be easily carried out later.
The correction of an edentulous ridge has to be performed prior to the construction of the fixed prosthesis and is aimed at making the ridge accept the pontic rather than making the pontic fit and adapt into the edentulous area. The modification of an undesirable contour and the creation of the adequate space are the most frequent problems that have to be treated.
Two types of situations have to be faced: (1) a reduced available space, and (2) an increased available space with the subsequent problem created by the location of the mucogingival junction and the width of the attached gingiva.
Width of the attached gingiva and location of the mucogingival junction in the edentulous ridge
The amount of attached gingiva, the location of the mucogingival junction in edentulous areas, and the presence of frenula should be carefully evaluated. Should they interfere with the placement of the apicobuccal margin of the pontic, proper management of this problem should be undertaken. In chapter 4 we gave the description of the usual and natural width and position of the attached gingiva. In this respect the edentulous area should be approached, considered, and treated the same way as dentulous areas because they have to fulfill the same requirements. Usually, this factor is either ignored or neglected by practitioners. Furthermore, one has to consider that conflicts in therapeutic modalities and goals inevitably exist between specialists and more precisely between the extractionist and the prosthodontist.
The coaption and suturing of buccal and lingual flaps to control hemorrhage and add to the patient’s postoperative comfort leave such an edentulous area covered with a reduced amount of gingiva that correct pontic placement is only possible if a subsequent mucogingival procedure is carried out (Fig 9-3).

Fig 9-3 The surgical coaptation of buccal and oral flaps most often leads to the necessity of restoring the edentulous area with an adequate width of attached gingiva.
Correction of a reduced available pontic space
The correction of reduced available pontic space, which requires the reduction of the thickness of connective tissue overlying the bone or the reduction of the osseous support, is a procedure that can be performed within the range of activity of a general practice.
These minor surgical corrective procedures permit the creation of an adequate vertical space for the pontic element and of an edentulous ridge that is similar in width and height to the adjacent ridge and, assuming that the mucogingival junction is in continuity with that of the adjacent teeth, we find ourselves in the presence of what we called a normal edentulous ridge.
Correction of an increased available space
Prosthodontic approach
From clinical and scientific observation it can be stated that the residual ridge that forms after the extraction of teeth is usually characterized by a loss of substance compared with the dentulous ridge. The rate of loss can vary in different sites within the same individual, is dependent upon biologic, anatomic, and mechanical factors, and may result in a deformed or collapsed type of ridge.
It was long believed that these deformities could only be compensated by prosthodontic means. Consequently, the shape of the pontic was modified and oversized to fit in the concavity of the residual ridge and its base modeled to be a precise mirror image of the tissue surface it contacted. This created a situation that was unacceptable esthetically and biologically because we assume that access for oral hygiene should be at all times respected. Most patients feel frustrated by the situation created by the elongated and nonanatomic pontic element and express justified complaints.
In an attempt to create some kind of harmony and give a visual perception of continuity with the remaining dentition, a pink gingival color, such as acrylic or porcelain flange, has been designed at the cervical end of the pontic to simulate normal tooth length. Unfortunately, this approach never responds fully to the esthetic expectations because of the difficulties of matching the gingival color and texture.
Another concept used in large defects has been to build up a false removable gingival flange, which can be adapted and locked in the interdental areas. Techniques have been described using rigid or soft acrylic resins. The addition of this flange aids in making the prosthesis look more lifelike by filling the dark triangle between elongated teeth, giving the illusion of papilla and marginal gingiva. At the same time, phonetics and air flow can be improved. This removable flange is indicated in all situations in which surgical procedures for one reason or another have failed or have not been used.
It seems that, with the increased use and success of osseointegrated implants, the poor esthetic appearance of emergence connecting devices, and the amount of vertical ridge collapse that most of these cases exhibit, this type of device will have to be improved (Figs 9-4 to 9-9). However, one should be realistic enough to admit that, at the present time, the majority of edentulous patients requiring implants are technically, functionally, economically, and esthetically better provided for with a removable denture base than with fixed prosthodontics when osseous ridge collapse has proceeded too far. This statement, based only on observation, should not prevent the implantologist, whose attention has been focused on the biologic success of the procedure, from providing systems with emergence devices that mimic dental roots in color and approximate diameter.

Fig 9-4 This edentulous maxillary has received six endosseous implants (IMZ) in an area going from the right to the left second premolar.

Fig 9-5 A primary suprastructure is connected to each implant by means of a long screw.

Fig 9-6 A precise insertion over this primary suprastructure of two ceramometallic fixed partial dentures interlocked by a precision attachment has been realized. Maintenance on the primary suprastructure is ensured by means of four micro-screws.
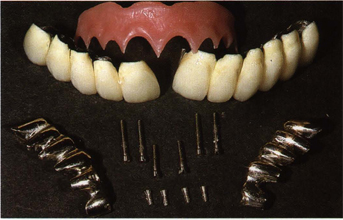
Fig 9-7 An overview of the elements of the puzzle that require an average of 20 minutes either for insertion or desinsertion.

Fig 9-8 Patient desire and insistence to receive a fixed restoration could not be totally satisfied because a removable gingival flange locked in the interdental spaces had to be proposed to hide the anesthetic metallic emergence of the implants as well as tooth length reaching 18 mm.

Fig 9-9 Gingival acrylic resin movable flange, or when old concepts come to help updated technology.
One should see that the correction of an increased pontic space in height and width by means of a fixed or removable prosthesis will be progressively abandoned in favor of surgical procedures, the developments of which present a challenge for our profession. Esthetic goals require providing the patient with a prosthesis that restores function and natural appearance.

Fig 9-10 Postextraction horizontal or buccolingual bone loss.
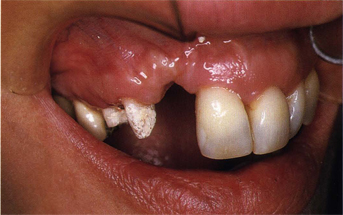
Fig 9-11 Postextraction vertical or coronoapical bone loss.
Surgical approach
The topographic observation of a residual ridge that has to be restored to its normal dimension through surgical procedures can be classified in three categories13:
1. Horizontal buccolingual loss of tissue with normal apicocoronal dimension (Fig 9-10).
2. Vertical apicocoronal loss of tissue with normal horizontal dimension (Fig 9-11).
3. A combination of buccolingual and apicocoronal defects resulting from the loss of tissue in height and width.
In addition, another classification was proposed in which the ridge deformities are classified by assessing the depth of the defect in relation to the adjacent ridge14: mild, less than 3 mm; moderate, from 3 to 6 mm; and severe, greater than 6 mm.
The second classification probably constitutes the best warning of possible complications and multiplication of the procedures necessary to achieve the desired result. This can ease the dentist-patient relationship in the sense that subsequent surgical procedures will be considered as foreseen and not the result of the failure of the first one.
Protocol for ridge augmentation
The basic requirements for success in the reconstruction of the collapsed ridge depend upon the following factors:
1. Understanding of the various types of defects.
2. Evaluation of the quantity and quality of soft tissue in the edentulous area to allow elevation of a flap and avoid perforation.
3. Evaluation of the blood supply in the area.
4. Absence of periodontal pockets on the adjacent teeth.
5. Preservation of the marginal papillae of the adjacent teeth.
6. Proper evaluation of the quantity and quality of grafting material from the donor site or choice of the implant material.
7. Evaluation of the number of surgical procedures necessary to achieve an optimal result.
Autogenous subepithelial connective tissue graft
The sources of the dense connective tissue autograft may be one of the several areas of the patient’s oral cavity. The most readily available sources of donor tissue are found in the lateral aspect of the palate and in the tuberosity region. Any edentulous posterior area presenting an adequate thickness of tissue may be used as well as gingivectomy tissue. The best area in the palate is located on the ridge near the teeth, posterior to the most distal ruga, away from the opening of the anterior palatinal foramen. The length of the horizontal incision is dependent upon the concavity to be filled.
Sequence
A split-thickness flap is dissected, elevated, and separated from the underlying bone15 to be used as donor material. The epithelialized superficial flap is placed over the denuded bone and coapted to the gingiva. The procedure can only be executed by hand dissection and is far from easy. As an alternative, one can proceed to the initial deepithelialization of the donor site with a rotary coarse diamond instrument and the elevation of the donor material with a hand scalpel or motor mucotom. The palatal area that is used as a preferential donor site for epithelial connective tissue graft most often does not provide subepithelial connective tissue grafts of a sufficient thickness. On the tuberosity region, the graft may be removed as part of a maxillary periodontal procedure or as an individual procedure. Several methods have been described to reduce the tuberosity and retromolar tabs. Whenever possible, the selection of the retromolar area should be favored because it aids in normalizing the sulcus depth and the accessibility to oral hygiene and provides, depending on the technique used, epithelial or subepithelial tissue graft of sufficient thickness for reconstructive goals.16,17 Postoperative discomfort is minimized when graft material is dissected from the retromolar area.
The availability of autogenous subepithelial tissue may sometimes be limited to the anatomic specificities of the oral cavity or the amount of tissue needed for the reconstruction of the ridge. Autogenous bone graft material taken from the iliac crest and rib have been utilized for the past three decades in edentulous ridge augmentation, but this procedure encountered the problem of the progressive loss of bone in the grafted areas.18,19 Various technical modifications have decreased the amount of bone resorption, but no really satisfactory results have been obtained, whatever the technique used. As a result, this material was never taken into consideration in partially edentulous ridge reconstruction.20,21 This problem stimulated research for a synthetic inorganic product available to support repair, both for periodontal defects and for ridge augmentation. To perform successful ridge augmentation, any biomaterial should satisfy the following criteria22:
1. Easily carved and molded.
2. Biocompatible and stable.
3. Firmly bond with bone and soft tissue.
4. Soft tissue healing after implant exposure.
5. Resistant to infection.
6. Acceptance for subsequent vestibuloplasty when necessary.
7. No adverse effect on adjacent bone.
Existing information has shown calcium phosphate ceramics to be safe and effective for clinical applications.23–25 They differ from previous hard tissue implant materials by their basic biocompatibility, which includes a lack of toxicity and inflammatory response.26–28 Calcium phosphate ceramics present the ability to become apparently bonded to bone by natural bond cementary mechanisms,21 but the nature of this bonding is still under investigation. The material is well tolerated by soft tissue25–27 and no really significant difference in the inflammatory response from different shapes of particles has been evidenced.21,29,30 Phosphate ceramics do not induce bone formation in soft tissue and therefore are not osteogenic, but they can be considered osteoconductive because they provide a physical matrix suitable for deposition of new bone.31 Investigators and clinicians have limited their attention to the performance of non-resorbable, high-density HA and porous HA and a potentially bioresorbable form of beta-tricalcium phosphate (TCP). The investigations on TCP with reference to animal and clinical studies concluded that the material provides a biocompatible matrix but has a tendency to resorb in an unpredictable fashion. Whereas some particles resorb, others remain as biologic foreign bodies or “fillers.” No mention is made of the use of this material in ridge augmentation, and investigations have been limited to the repair of periodontal defects.32
Hydroxyapatite
HA is a dense calcium phosphate ceramic material possessing considerable compressive strength and consequently limited mechanical properties. To minimize the problem of brittleness that was observed in HA tooth implants, dense calcium phosphate ceramic particles were produced. The reparative matrix of bone invasion surrounding the particles provided strength to the implant. Particles are available in different forms: irregular and multifaceted, smooth and rounded. Although highly biocompatible, HA undergoes some degradation in the tissue. The degradation rate depends on variations in the formation of ceramic, crystallographic structures and the rate of cooling and />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


