9
Restorative Dentistry
Case 1
Resin Restoration of Incipient Decay (Primary or Permanent Molar)
A. Presenting Patient
- 6-year-, 8-month-old Hispanic female
- Presents for a restorative visit
B. Chief Complaint
- Patient has presented previously for a comprehensive exam; this is her first restorative visit. Mother reports that “child has some small cavities”
C. Social History
- Patient is in kindergarten
- Involved in swimming and summer camps
- Parents both work as research assistants
- Socio-economic status is mid-level
- Patient is an only child
D. Medical History
- Mild intermittent asthma with symptoms related to specific allergens (see Fundamental Point 1).
- American Society of Anesthesiologists (ASA) 2
- Medications: Singulair for seasonal allergies
- Patient has never been hospitalized; has never gone to the emergency room for asthma treatments
- Obtain a thorough understanding on the severity and control of the asthma. See Chapter 1 Case 7 for a complete presentation of the clinical issues related to asthma
- Question on (Graham 2006):
- Medications used for asthma control and frequency
- Frequency and severity of the episodes
- Any visits to the emergency room for the asthma
- Symptoms experienced by the patient
- Limitations or restrictions on any activities
- Quick relief medications, including short-acting beta agonists (e.g., albuterol) are taken as needed to promptly reverse acute airflow obstruction and relieve accompanying symptoms. Increased use of asthma medication and time of the day that the asthma medication is used could lead to xerostomia. This could be associated with increase in caries experience in the primary dentition. (Redding and Stoloff 2004, Milano et al. 2006)
E. Medical Consult
- Not necessary at this time
F. Dental History
- Child had her first dental visit one month ago
- Positive behavior for all care given
- Optimal water fluoridation
- High cariogenic diet
- Toothbrushing with supervision twice a day
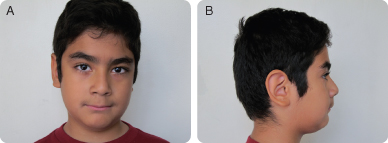
G. Extra-oral Exam (Figures 9.1.1 a–b)
- Patient is slightly overweight for height and age
- Mild deviation at opening and closing
Figure 9.1.1a–b. Facial photographs
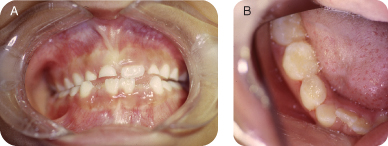
H. Intra-oral Exam
- Early mixed dentition
- Retained primary maxillary right central incisor with slight mobility
- Occlusion: 2 mm of overjet, 5% overbite (secondary to tooth emerging in mouth); mild crowding of the lower arch; bilateral class I molars, bilateral class I canines
- Soft tissue: Within normal limits
- Moderate plaque accumulation
- Oral hygiene is poor
- Visible interproximal caries on tooth S
- Tooth T has stained occlusal groves and possible cavitation. Cavitation noted on the buccal groove.
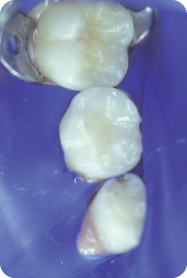
Figure 9.1.2a–b. Pre-operative intra-oral photos
I. Diagnostic Tools
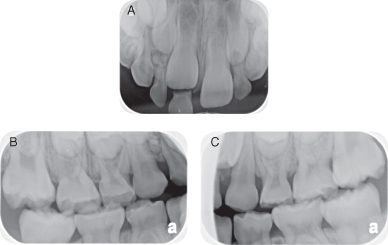
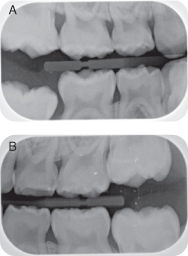
- Two bitewing radiographs and one maxillary anterior periapical radiograph show interproximal caries, a retained primary tooth, and a radio-opaque area apical to tooth D. (Figures 9.1.3 a–c)
- No other radiographs were taken at this time due to the mother’s concern for radiation exposure and no other pathology suspected
- The patient will have a panoramic film taken at a future recall and a maxillary anterior periapical radiograph as indicated to monitor emergence of tooth number 8 (see Fundamental Point 3).
Figure 9.1.3a–c. Pre-operative radiographs
- The American Academy of Pediatric Dentistry (AAPD) recommends that a new patient with a transitional dentition should have a radiographic exam that includes posterior bitewings (if contacts between the teeth are present) and a panoramic radiograph or selective periapical radiographs. See the AAPD radiography guidelines: http://www.aapd.org/media/Policies_Guidelines/E_Radiographs.pdf (AAPD 2011–2012a)
- The American Dental Association (ADA) also has radiography guidelines similar to the AAPD. See the ADA Radiography guidelines: http://www.ada.org/sections/professionalResources/pdfs/topics_radiography_examinations.pdf
- In comparison, the European Academy of Pediatric Dentistry (EAPD) states that baseline radiographs should start at the age of 5 or based on individual risk assessment. They also state that a panoramic radiograph is not required on healthy, asymptomatic children. See the EAPD radiography guidelines: http://www.eapd.gr/dat/590A99C0/file.pdf
J. Differential Diagnosis
- N/A
K. Diagnosis and Problem List (see Fundamental Point 2)
Diagnosis
- Mild asthma
- Overweight
- Dental caries
- Pathology apical to tooth D
Problem List
- High caries risk secondary to asthma, cariogenic diet
- Moderate plaque accumulation and lack of dental home prior to 6 years of age (determined using American Academy of Pediatric Dentistry caries assessment tool, AAPD [2011–2012b])
- Dental caries
- Over-retained tooth E with delayed eruption of tooth number 8
- Pathology apical to tooth D
- Possible intra- and extra-oral concerns with asthmatic patients (Steinbacher and Glick 2001):
- Patients tend to be mouth breathers
- Reduction in salivary flow and dry mouth may increase caries risk
- Throat irritation
- Dryness of mouth
- Candidiasis
- Gingivitis
- Overweight children can be susceptible to secondary problems including hypertension, diabetes mellitus, and increased caries rate. Appropriate diet and patient referral should be considered when necessary (Willerhausen et al. 2007)
L. Comprehensive Treatment Plan
- Establish a dental home
- Patient referred to oral surgeon to evaluate possible supernumerary tooth or odontoma apical to tooth D
- Preventive treatment
- Dental prophylaxis
- Fluoride treatment
- Review of oral hygiene (with parent and child) at the beginning of treatment and at subsequent visits
- Sealant on first permanent molars: numbers 3 (OL) and 14(OL)
- Restorative treatment
- Number 19 (0) resin restoration
- A (OL) resin restoration
- K (MO) resin restoration
- S (DO) resin restoration
- T (OB) resin restoration
- Number 30 (O) resin restoration
- Monitoring of growth and development with special attention to exfoliation of E and subsequent emergence of number 8. Consider an orthodontic consultation. Patient will have a panoramic radiograph later for monitoring growth and development
- Recall at six months and every six months thereafter
M. Treatment
- Local anesthesia: 36 mg of Lidocaine with 1:100,000 epinephrine was administered via mandibular nerve block on the right side. (Maximum recommended dosage [MR] of Lidocaine = 4.4 mg/kg. This patient weights 35.6 kg, therefore MRD = 156.64 mg Lidocaine)
- Rubber dam isolation: A W8A Ivory clamp was placed on tooth number 30 to achieve isolation for the resin restoration to be performed in tooth T (Figure 9.1.4).
- Cavity preparation: Cavity preparations for this conservative resin restoration eliminate the need for extension for prevention (see Background Information 1 and Fundamental Point 4). The cavity preparation is limited to the small areas of carious enamel or dentin. As seen in figure 9.1.5, the carious lesion was confined to three separate areas: the buccal pit and two areas in the occlusal surface. (Simonsen 1978a, Simonsen 1978b, Simonsen 2005)
- Filling of cavity preparation: Conventional etching with 37% phosphoric acid was done. Filling of the cavity preparation was performed using a hybrid composite resin. A partially filled sealant material was placed on the uncavitated areas of the tooth (Figure 9.1.6).
Figure 9.1.4. Tooth T, pre-operative isolation

Figure 9.1.5. Tooth T, cavity preparation. Note how the cavity preparations (arrows) do not involve unaffected fissures. There is no extension for prevention
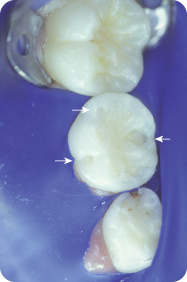
Figure 9.1.6. Tooth T, post-operative completed restoration
- Minimally invasive resin restorations are indicated for teeth with cavitated carious lesions in which the remaining grooves are sound but considered to be at high caries risk
- Their advantages include:
- Conservative preparation design
- Ability to isolate tooth
- Sealant for prevention
Simonsen (1978a), Simonsen (1978b), Simonsen (1980), Simonsen (1982), Simonsen (2005)
- Traditionally, amalgam was the restorative material of choice for posterior restorations. The early resin-based composites had large silica particles as fillers and they were not silinated to bond to the resin within the restorative material. These properties led to breakdown of the resin-based composite when placed in areas where significant wear occurred (Bayne et al. 1988). Although amalgam has been an effective restorative material for more than a century (Fuks 2002), extension for prevention was recommended so that all susceptible pits and fissures were included in the cavity preparation
- Minimally invasive resin restorations offer conservation of non-carious tooth structure (Donly and García-Godoy 2002). Being able to bond to dentin and enamel allows for only carious tooth structures to be removed, with bonded resin-based composite replacing tooth structure that was removed due to decay. A sealant is then placed over the entire occlusal surface, filling in any surface imperfections in the filled resin-based composite restoration that may have been created during finishing, and covering all caries-susceptible pit and fissures on the occlusal surface that were not included in the tooth cavity preparation (Simonsen 1980). The sealant provides prevention to future occlusal decay
N. Prognosis and Discussion
- The prognosis for caries is questionable because of the patient’s past experience of dental caries, as a predictor of future caries (Powell 1998)
- However, education in the form of anticipatory guidance and the establishment of a dental home could improve the patient’s oral health habits and reduce her caries risk
O. Complications and Alternative Treatment Plan
- How would management differ if the patient had severe, uncontrolled asthma?
- What is the proper protocol for managing an asthmatic episode during dental treatment?
- How would management differ if the patient lived in a non-fluoridated community?
- How would the approach to sedation change if a severely overweight patient requires moderate oral conscious sedation (Baker and Yagiela 2006)?
- Would a restoration be needed for this patient if tooth T presented with only stained grooves and no cavitation upon clinical examination?
Self-study Questions
1. What will be helpful to identify overweight and/or obesity in children older than two years of age?
2. What is the purpose of the sealant placement in a preventive resin restoration (PRR)?
3. What is a contraindication to placing a resin restoration?
4. Is the wear of resin-based composite a significant concern when placing a resin restoration?
Answers are located at the end of the case.
Bibliography
American Academy of Pediatric Dentistry. 2011–2012a. Prescribing Dental Radiographs, Reference Manual. Pediatr Dent 33(6):289–91.
American Academy of Pediatric Dentistry. 2011–2012b. Guideline on Caries-risk Assessment and Management for Infants, Children, and Adolescents, Reference Manual. Pediatr Dent 33(6):110–15.
Baker S, Yagiela JA. 2006. Obesity: a complicating factor for sedation in children. Pediatr Dent 28(6):487–93.
Barlow SE, Bobra SR, et al. 2007. Recognition of childhood overweight during health supervision visits: Does BMI help pediatricians? Obesity (Silver Spring) 15(1):225–32.
Bayne SC, Taylor DF, Roberson TM, Sturdevant JR, Wilder AD, Heymann HO, et al. 1988. Posterior composite wear factors. Trans Acad of Dent Mater 1:20–1.
Chinn S. 2006. Definitions of childhood obesity: current practice. Eur J Clin Nutr 60(10):1189–94.
Donly KJ, García-Godoy F. 2002. The use of resin-based composite in children. Pediatr Dent 24(5):480–8.
Fuks AB. 2002. The use of amalgam in pediatric dentistry. Pediatr Dent 24(5):448–55.
Graham L M. 2006. Classifying asthma. Chest 130(1 Suppl):13S-20S.
Milano M, Lee J Y, et al. 2006. A cross-sectional study of medication-related factors and caries experience in asthmatic children. Pediatr Dent 28(5):15–9.
Powell L V 1998. Caries prediction: a review of the literature. Community Dent Oral Epidemiol 26(6):361–71.
Redding GJ, Stoloff S W. 2004.”Changes in recommended treatments for mild and moderate asthma. J Fam Pract 53(9):692–700.
Simonsen RJ 1978a. Preventive resin restorations (I). Quintessence Int Dent Dig 9(1):69–76.
Simonsen RJ. 1978b. Preventive resin restorations (II). Quintessence Int Dent Dig 9(2):95–102.
Simonsen RJ. 1980. Preventive resin restorations: three-year results. J Am Dent Assoc 100(4):535–9.
Simonsen RJ. 1982. Preventive resin restoration. Innovative use of sealants in restorative dentistry. Clin Prev Dent 4(4):27–9.
Simonsen RJ. 2005. Preventive resin restorations and sealants in light of current evidence. Dent Clin North Am 49(4):815–23, vii.
Steinbacher DM, Glick M. 2001. The dental patient with asthma. An update and oral health considerations. J Am Dent Assoc 132(9):1229–39.
Willerhausen B, Blettner M, et al. 2007. Association between body mass index and dental health in 1,290 children of elementary schools in a German city. Clin Oral Investig 11(3):195–200.
SELF-STUDY ANSWERS
1. Body mass index (BMI) calculation (Chinn 2006, Barlow and Bobra 2007)
2. Eliminate the need to extend the preparation to prevent future decay and to fill any voids in the surface of the hybrid resin-based composite created during finishing
3. Inability to isolate the tooth; known allergy to resin-based composite material
4. No. Current materials have biomechanical properties that can reduce the risk of excessive wear
Case 2
Class II Glass Ionomer
Figure 9.2.1a–b. Facial photographs

A. Presenting Patient
- 5-year-, 6-month-old Caucasian female
- New patient visit
B. Chief Complaint
- Mom states, “My daughter needs to see a dentist”
C. Social History
- Patient is in kindergarten
- Patient and 7-year-old brother live with mother
- Mother is the primary caregiver and has a full-time job
- Socio-economic status is lower level
D. Medical History
- Patient has no cardiovascular, pulmonary, gastro-intestinal, hepatic, renal, or genito-urinary disease or abnormality
- No medications
- No known disease or abnormality and no history of allergies (American Society of Anesthesiologists [ASA] I)
E. Medical Consult
- Not necessary at this time
F. Dental History
- Patient has never been to a dentist
- Optimal water fluoridation levels
- Moderate cariogenic diet including carbonated soda
- Toothbrushing without supervision, once daily
G. Extra-oral Exam
- No significant findings
Figure 9.2.2a–e. Pre-operative photos

H. Intra-oral Exam
- Primary dentition
- Occlusion: 2-mm overjet, 75% overbite; closed contacts in anterior and posterior
- Mesial step primary molars, class I canines
- Soft tissue: Within normal limits
- Moderate plaque accumulation
- Oral hygiene is poor
- Staining on occlusal surfaces, but no visible demineralization or cavitations
I. Diagnostic Tools
- Two bitewing radiographs show interproximal decay, B-do, I-do, J-mo, L-do (see Figures 9.2.3 a-b and Fundamental Point 1)
Figure 9.2.3a–b. Pre-operative bitewing radiographs
- The American Academy of Pediatric Dentistry (AAPD) recommends that a new patient with a transitional dentition should have a radiographic examination that includes posterior bitewings (if contacts between the teeth are present) and a panoramic radiograph or selective periapical radiographs. See the AAPD radiography guidelines: http://www.aapd.org/media/Policies_Guidelines/E_Radiographs.pdf (AAPD 2011–2012a)
- The American Dental Association (ADA) also has radiographic guidelines similar to the AAPD. See the ADA radiography guidelines:
http://www.ada.org/sections/professionalResources/pdfs/topics_radiography_examinations.pdf
J. Differential Diagnosis
- N/A
K. Diagnosis and Problem List
Diagnosis
- Caries
- Need for oral hygiene improvement
Problem List
- Moderate caries risk due to diet, oral hygiene, and presence of decay (per American Academy of Pediatric Dentistry caries risk tool [AAPD 2011–2012b])
- Generalized plaque accumulation
- Lacks a dental home
- The mesio-occlusal lesion in this patient was restored with a class II resin-modified glass ionomer cement restoration. Due to difficulty in isolating the tooth and the moderate caries risk status of the child, resin-modified glass ionomer cement was chosen rather than resin-based composite. Saliva contamination causes the tooth/resin interface bond to be compromised, with subsequent restoration failure with resin-based composite restorations. Glass ionomer cement can still chemically cure in the presence of minimal contamination. The fluoride release from the glass ionomer cement can aid in inhibiting tooth demineralization at restoration margins in this moderate-caries-risk patient. According to the Pediatric Restorative Dentistry Consensus Conference, primary teeth can be effectively restored with resin-modified glass ionomer cement Class II restorations (AAPD 2002)
L. Comprehensive Treatment Plan
- Establish a dental home
- Dental prophylaxis
- Fluoride treatment (5% fluoride varnish placed)
- Review of oral hygiene (with parent and child)
- Recommend use of floss
- Restore decayed teeth, B-do, I-do, J-mo, L-do
- J-mesio-occlusal decay: To be restored with a resin-modified glass ionomer cement restoration
- I-disto-occlusal decay: To be restored with a resin-modified glass ionomer cement restoration
- Prevention Plan
- Three-month recall, re-evaluate oral hygiene status and caries risk
- Prescribe a remineralizing product such as those containing amorphous calcium phosphate
- A class II resin-modified glass ionomer cement restoration can be very effective. Caries is removed with a 330 bur, creating a rectangular box preparation with the axial wall placed in dentin as far as caries extends. The preparation buccal and lingual walls slightly converge occlusally. A dovetail is placed from the proximal box of the preparation onto the occlusal surface. This provides a bulk of glass ionomer cement which is less susceptible to fracture than just a slot preparation, in which only the proximal box is prepared and restored with restorative material. It is important to place butt cavosurface margins due to the brittleness and compressive strength of resin-modified glass ionomer cement
- A resin primer can be placed prior to the resin-modified glass ionomer cement to improve bond strength to tooth structure. Following placement of the glass ionomer cement restoration, the tooth should be isolated as best as possible so that saliva does not wash away aluminum during the acid-base chemical cure. This allows for maximum uptake of aluminum, which maximizes compressive strength
- After the restoration is finished and polished, a resin adhesive should be placed over the restoration surface. Again, this allows the aluminum that has not been uptaken into the glass ionomer setting reaction to remain at the restoration surface for uptake as the reaction continues over 24 hours
American Academy of Pediatric Dentistry (2002), Burgess et al. (2002), Donly and García-Godoy (2002), Waggoner (2005)
M. Treatment (Figures 9.2.4–9.2.7)
Figure 9.2.4. Isolated tooth J with mesio-occlusal preparation, including occlusal dovetail

Figure 9.2.5. Primer applied

Figure 9.2.6. Resin-modified glass ionomer cement applied
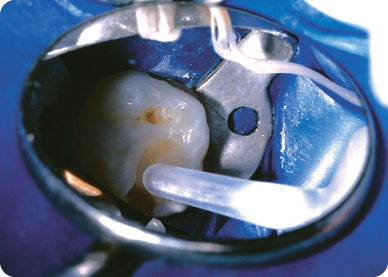
Figure 9.2.7. Final restoration

N. Prognosis and Discussion
- Prognosis for caries is moderate due to the patient’s moderate cariogenic diet and non-ideal oral hygiene. Prognosis could be improved with reduction in soda frequency and improved oral hygiene maintenance. Survival of the class II restoration is good due to the low to moderate caries risk and receptive acceptance of oral hygiene instructions
O. Complications and Alternative Treatment Plan
- If the patient had been classified as high risk, a stainless steel crown would be considered more appropriate. Likewise, if caries had extended to the pulp, requiring pulp therapy, a stainless steel crown would be the treatment of choice. Conversely, if the patient had excellent oral hygiene maintenance and the tooth could be isolated well, a resin-based composite could be considered as a restorative material
Self-study Questions
1. A resin-modified restoration would not be appropriate for:
2. The proximal walls of a class II preparation in a primary molar should:
3. The cavosurface margin of a class II preparation in a primary molar should:
4. Placing a primer adhesive prior to the placement of a resin-modified glass ionomer cement:
5. A glass ionomer cement setting reaction occurs over:
Answers are located at the end of the case.
Bibliography
American Academy of Pediatric Dentistry. 2011–2012a. Prescribing Dental Radiographs Reference Manual. Pediatr Dent 33(6):289–91.
American Academy of Pediatric Dentistry. 2011–2012b. Guideline on Caries-risk Assessment and Management for Infants, Children, and Adolescents, Reference Manual. Pediatr Dent 33(6):110–15.
American Academy of Pediatric Dentistry. 2002. Pediatric restorative dentistry consensus conference. Pediatr Dent 24(5):374–6.
Burgess JO, Walker R, Davidson JM. 2002. Posterior resin-based composite: review of the literature. Pediatr Dent 24(5):465–79.
Donly KJ, García-Godoy F. 2002. The use of resin-based composite in children. Pediatr Dent 24(5):480–8.
Waggoner W. 2005. Restorative dentistry for the primary dentition. In: Pediatric Dentistry Infancy through Adolescence, Fourth edition. Elsevier: St. Louis.
SELF-STUDY ANSWERS
1. c, A high-caries-risk child
2. a, Converge
3. d, Not be beveled
4. b, Increases the bond strength to tooth structure
5. d, Twenty-four hours
Case 3
Class II Resin Restoration
Figure 9.3.1a–b. Facial photographs
A. Presenting Patient
- 7-year-, 6-month-old Hispanic male
- Presenting for a recall examination
B. Chief Complaint
- Mom stated, “He is here for his check-up and he has some cavities”
C. Social History
- Patient is in first grade
- Patient is only child
- Parents are married
- The father owns his own plumbing company; the mother helps out with the business
- Socio-economic status is mid-level
D. Medical History
- Past history of rotovirus in December 2004. Patient was hospitalized for two days due to dehydration. No further complications
- Non-contributory medical history
- American Society of Anesthesiologists (ASA) I classification
E. Medical Consult
- Not necessary
F. Dental History
- Fair oral hygiene (brushes twice a day; supervised brushing, flossing)
- Tap water is fluoridated, uses fluoridated toothpaste
- High cariogenic diet
- Previous treatment was unable to be completed six months ago due to uncooperative behavior. Parents opted to defer treatment at that time
G. Extra-oral Exam
- Within normal limits
H. Intra-oral Exam
- Soft tissues are within normal limits
- Moderate plaque accumulation
- Oral hygiene is fair
- Early mixed dentition
- Tooth number 10 erupting; all permanent first molars present
- Occlusion: Bilateral class I molar relationship; bilateral class I canines; good spacing; overjet 1 mm, overbite 10%
I. Diagnostic Tools
- Two bitewing radiographs and a periapical radiograph of the mandibular right side (to evaluate possible pulpal or furcation involvement in tooth S) showed multiple carious lesions (Figu/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


