9 Oral Neoplastic Disease
9.0 INTRODUCTION
Both benign and malignant neoplastic conditions can be encountered in the oral cavity, potentially making oral health care specialists primarily responsible for initial detection of such lesions. Similarly, oral health care providers play an important role in surveillance of patients who have previously been treated for head and neck cancer given the high risk of local recurrence and new primary tumors. Importantly, earlier diagnosis of neoplastic disease can have a significant impact on improving treatment outcomes and therefore reducing a patient’s morbidity and mortality. Tumors can arise from any tissue component of the oral cavity, including squamous mucosa, salivary glands, bone and cartilage, teeth, muscle, fibrous tissue, vascular tissue, neural tissue, and fat (Table 9.1). In addition to primary diseases arising within the oral cavity, metastatic tumors and hematologic malignancies can present with oral signs and symptoms, and these findings may represent the initial clinical manifestation or may indicate recurrent/relapsed disease.
Oral neoplastic disease can present with a range of signs and symptoms that generally correspond to the size, location, and extent of disease, as well as specific clinical features that are unique to certain conditions (Alert Box 9.1). Pain is generally caused by nerve involvement and may be encountered at any stage of disease. Jaw asymmetry, limited mouth opening (trismus), shifting and/or loosening of teeth, a change in the fit of a removable prosthesis, and paresthesia or other neurosensory changes can all be signs of benign or malignant tumors. When present, symptoms may be constant or episodic and may be provoked by functional movements such as speaking, chewing, or swallowing. Paresthesia or anesthesia is generally an ominous sign suggestive of invasive disease, and neurosensory changes in the cranial and/or cervical nerve distribution should be considered highly suspicious for a primary tumor or metastasis to the head and/or neck. Of particular note, metastasis to the mandible should be considered if neurosensory changes present in the mental nerve distribution, especially in a patient with a known history of a solid cancer (e.g., breast, lung, prostate), with or without a known history of metastases (Figure 9.1). Loss of motor function, manifested by difficulty speaking, chewing, or swallowing, is another important potential sign of malignancy that can be observed in the context of both local/intraoral (e.g., squamous cell carcinoma of the tongue) and central (e.g., metastatic disease to the brain; Figure 9.2) lesions. Soft tissue changes that should be considered suspicious include focal areas of thickening and/or mass-like changes, non-healing ulcerations, and induration. Periapical and panoramic radiographic features of neoplastic disease include focal areas of radiolucency and radiopacity, focal destruction of cortical bone, and the appearance of “floating” teeth (Figure 9.3).
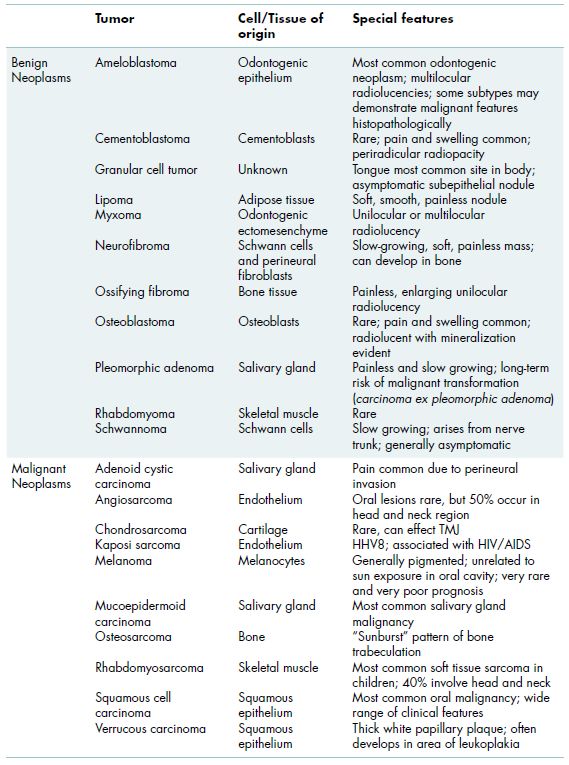
Table 9.1 Benign and malignant tumors of the head and neck.
| Clinical signs | Clinical symptoms |
| White and red changes (erythroleukoplakia) Ulceration Induration Exophytic/endophytic growth Change in fit of oral prosthesis Unexplained mobility of teeth Neurologic abnormalities |
Pain Paresthesia/sensory changes Bleeding Motor changes Dysphagia |
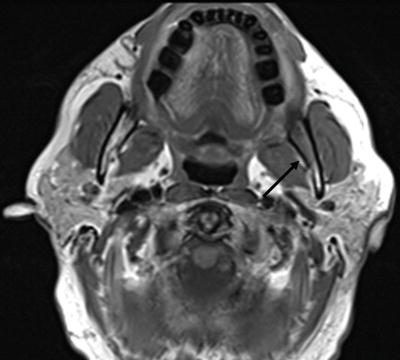
Figure 9.1 57-year-old male with diffuse large B-cell lymphoma with acute onset of pain and paresthesia of the left posterior mandible and ramus. Axial T1-weighted MRI of the brain demonstrated unusual appearance of the marrow in the left mandible near the area of the inferior alveolar nerve foramen, with prolonged T1 and T2 signal, consistent with marrow infiltration of his underlying lymphoma.
Nearly 95% of all oral malignancies are squamous cell carcinomas (SCCs) that arise from the mucosal lining of the oral cavity. Lymphoma, salivary gland cancers, and other less common malignancies, as well as distant metastases to the oral cavity, account for the remainder. Relative to many of the other conditions discussed in this book, cancer is a very rare disease; however, the consequences of a delay in diagnosis or misdiagnosis can be devastating. Therefore, it is imperative for oral health care specialists to recognize signs and symptoms and to provide appropriate and timely referral for diagnosis and comprehensive management.
More challenging is the diagnosis and management of pre-malignant or what are often more appropriately termed potentially malignant oral lesions, defined as lesions that have the potential to undergo malignant transformation. The goal of the oral health care provider should be to facilitate diagnosis and to reduce as much as possible any lag time between detection of clinical abnormalities and referral to a specialist for close monitoring, diagnosis, and/or further management.
Figure 9.2 62-year-old male with metastatic prostate cancer with progressive right-sided tongue and constrictor muscle weakness (patient is moving the tongue as far to the right as possible) and difficulty speaking and swallowing (a). Sagittal MRI (b) demonstrates the extent of the metastatic lesion in the area of the clivus. Axial images demonstrate narrowing of the outlet of the right cranial nerve XII (computed tomography; c), and cranial nerve IX (MRI; d).

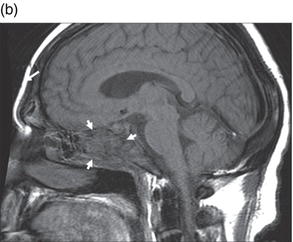

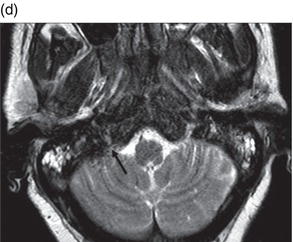
Figure 9.3 Axial CT scan of a patient with advanced relapsed squamous cell carcinoma of the right mandible with destruction of the cortical bone.
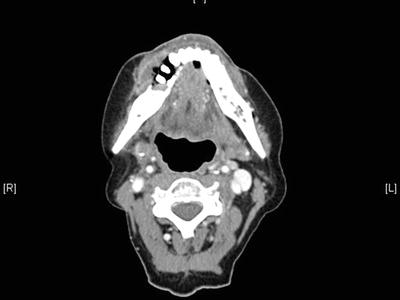
Figure 9.4 Proliferative verrucous leukoplakia of the left retromolar pad, mylohyoid ridge, and lateral tongue.

9.1 Benign neoplasms of the oral cavity
Benign neoplasms can arise from any tissue type and have unlimited growth potential. Despite being “benign,” such lesions may be associated with significant morbidity, depending on the size and location of the lesion and the approach for management. Many neoplasms will present asymptomatically, being detected during routine clinical or radiographic examination. Regardless of clinical features, all suspicious lesions require biopsy for definitive diagnosis, and further testing may be warranted to determine the most appropriate management.
9.2 Oral potentially malignant lesions
Oral potentially malignant lesions include leukoplakia, erythroleukoplakia, and erythroplakia. Leukoplakia is defined as a white mucosal plaque that cannot be removed and cannot be diagnosed as any other condition (e.g., lichen planus, pseudomembranous candidiasis). The risk that leukoplakia will undergo malignant transformation over a patient’s lifetime ranges from less than 5% to as high as 40%; however, no reliable indicators have been identified that can actually predict this risk. Proliferative verrucous leukoplakia is a unique clinical entity seen primarily in older women, characterized by one or more areas of folded/wrinkled-appearing leukoplakia (Figure 9.4) that extend slowly with time; it is associated with a high rate of malignant transformation to verrucous carcinoma (a low-grade variant of SCC with low risk of metastasis) or SCC. Erythroplakia is defined as a red oral mucosal plaque that, like leukoplakia, cannot be defined as any other clinical entity (e.g., lichen planus, erythematous candidiasis). Erythroplakia and erythroleukoplakia (mixed red and white lesion) are associated with a very high risk of malignancy (much higher than leukoplakia), with as many as 90–100% of cases ultimately demonstrating severe dysplasia (carcinoma in situ) or transformation to invasive carcinoma.
The actual histopathologic diagnosis of any given potentially malignant lesion must also be considered to determine an overall assessment of cancer risk; therefore, biopsy of any suspicious lesion is essential. Microscopic findings can include normal-appearing epithelium, acanthosis (an orderly increase in thickness of the epithelium), hyperkeratosis, hyperplasia, dysplasia (disorderly cellular architecture with malignant features, including mitotic figures and pleomorphism), and SCC (same cellular changes as dysplasia with evidence of invasion through the basement membr/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


