Chapter 9
Communication, Stress and Improved Patient Care
Aim
To outline the basis of self-care for dental health professionals to enable them to function optimally and deliver high-quality oral health care provision.
Outcome
After reading this chapter readers should better understand what factors, external and internal to their workplace, influence their psychological well-being and be able to apply recommended ways of assessing and coping with occupational pressures, in the short and long term. In addition, on a broader level, readers should understand the benefits of introducing applied psychological principles to maintain a satisfactory level of physical health and mental well-being and, in turn, sustain the standard of care for their patients. Occupational psychologists, such as Cary Cooper, have studied the relationship between stress, ill health and changes in clinical dental practice. The widespread belief that dentistry is the most stressful of all health professions is not without some foundation, although there is considerable variation among individuals and practices. Dentists are, for instance, more likely to have problems with dependency on alcohol and drugs, suffer from coronary heart disease, commit suicide and be divorced compared with members of the general population. Recent evidence suggests that the claim that dentists score less favourably on these health-related indices is unconvincing when compared to other professional groups, including accountants and lawyers.
Stress has a multifaceted definition – ‘results from an imbalance between the demands made of individuals and their perceived ability to cope’. Stress can be considered as an affective response to significant life events, such as a road traffic accident, bereavement or divorce. Any of these events can trigger a stress reaction. Stress can also be construed as a physical response with the well-known physiological reactions of flight or fight. The recognition of the potential sources of occupational stress enables practitioners to possess the means to reduce stress and thereby prevent the condition of burnout.
Sources of Occupational Dental Stress
Wilson’s study highlighted the stressors for over 1,000 general dental practitioners in England and Wales, the large majority of whom were working in NHS practices. Respondents indicated the degree of pressure from over 30 occupational stressors within dental practice. The use of identical questions enabled comparison with an earlier study by Cooper and his research team. Results are summarised in Table 9-1.
| Stressor | Percent considerably stressed or more | Rank order | Rank order UK compar son study (1986)* |
| Running behind schedule | 62 | 1 | 3 |
| Working constraints set by the NHS | 58 | 2 | – |
| Coping with difficult or uncooperative patients | 57 | 3 | 2 |
| Working quickly to see as many patients as possible | 51 | 4 | – |
| Working under constant time pressures | 51 | 5 | 4 |
| Patient having a medical emergency in surgery | 51 | 6 | 1 |
| Seeing more patients than you want to for income reasons | 50 | 7 | – |
* study by Cooper et al British Dental Journal 1987; 184:499–502
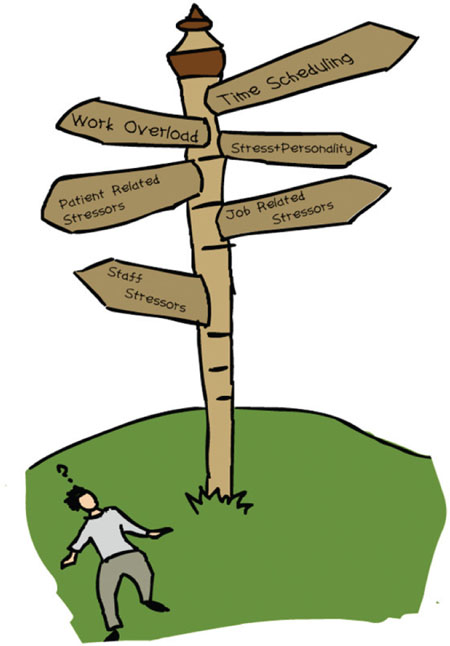
Wilson’s study showed that workload and time pressures were the most frequently rated pressures. Associated with these were stressors summarising income-related issues (for instance, managing financial demands, balancing the accounts and so on) and difficult patients. These stressors can be grouped into five areas (see Table 9-2). The following sections describe some of the factors in more detail under each heading.
| Stressor group | Mean score |
| Time-related | 3.49 |
| Income-related | 3.24 |
| Patient-related | 3.23 |
| Job-related | 2.64 |
| Staff/technical-related | 2.51 |
Workload
Excessive workload has been described as simply having too much work to do or, from a qualitative perspective, work being too difficult for the individual. Quantitatively, dental occupational stress can be experienced through the pressure of time in treating patients. The NHS system of payment – fee per item, or piecework – significantly increases dentists’ work overload as the tendency to see more patients and undertake more procedures to cover practice overheads is high. Qualitatively, work overload is associated with dentists having to compromise their working practices from an ideal that they learnt in dental school to what can be delivered under the constraints of a system of remuneration. The longer-term outcome is poor assessment of the patient’s previous dental experiences, dental anxiety status, expressed or felt needs. This may eventually lead to difficulties with patients. Dentists, because of their own life experiences and personalities, will either be able or not to cope with criticisms of their professional integrity. Dentists who are anxious will react with hostility to patients with high dental anxiety status. Dentists whose work is criticised by patients will react with disappointment and anger. Such experiences are perceived as being stressful by both dentist and patient.
Work underload is associated with boring and repetitive work observed in occupations such as dentistry. Dentists who are not sufficiently challenged intellectually by their work can experience occupational stress. Paradoxically, work underload can therefore be a stressor.

Time-Scheduling
Dentists seek to become more efficient and consider fitting more patients into their diaries. Among recently qualified dentists the competition for dental patients is strong. The new dentist in general practice must cover the costs of setting up and running a dental practice and so must encourage a full appointment book. An appointment missed, let alone time off due to sickness or other reason, will in effect be lost income. Cooper et al (1987) demonstrated that ‘running behind schedule’ and ‘constant time pressures’ ranked third and fourth, respectively, out of over 30 potential stressors by dentists in general dental practice. Wilson et al (1998) showed that time-related stressors were the most highly rated. Sixty-two percent reported that ‘running behind schedule’ was ‘considerably stressful’.
Job-Related Stressors
In general, being knowledgeable about new technologies, attending meetings, reading journals and keeping up with new materials and clinical techniques have all been recognised as vital tasks for dentists. Continuing professional development has become mandatory in many countries. There may be wide variation in response to these demands. Attendance at meetings can provide a necessary break from routine and a time to gain support from peers in general discussion periods. Some dentists may regard such activities as interrupting the business of their practice.
Changes in work regimes (fee for item to insurance schemes,) together with new technologies, are additional stressors for the dentist. Further examples of changes to working practices that are increasing demands are time taken up with completing paperwork, being on call, continuous care and capitation, and longer working hours.
Sources of dental occupational stress in the surgery environment may include:
-
time taken for materials to set and radiographs to develop
-
the noise from both high and low-speed handpieces
-
equipment that fails to operate optimally
-
constant attention to small detail
-
manual dexterity and close working
-
procedures and devices not working properly
-
the persistent glare of the operating lights
-
the smells of dental materials.
Beyond the immediate environment of the dental chair, the design and layout of the surgery and other factors, such as the ventilation or air conditioning system, can all either reduce or exacerbate stress. Communication networks will be influenced by the layout and design of the dental surgery, waiting room and staff areas. The nature of dental treatment with its concentration on fine detail and close work can cause eyestrain and headaches. The changes in levels and frequency of noise more than a constant pitch can act as an irritant. Concerns about close contact with certain materials such as mercury, nitrous oxide, anaesthetic gases and more importantly fears of contamination infection with diseases such as HIV, hepatitis and tuberculosis may all contribute to staff anxiety in />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


