Advancement Flaps
Introduction
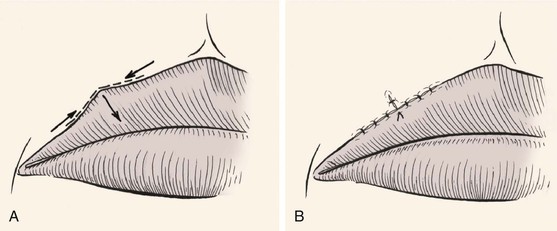
Most local cutaneous flaps used in the head and neck have some component of advancement during movement of the flap to the recipient site. An example is the paramedian interpolated forehead flap. Although this flap is classified as pivotal, it frequently is necessary to undermine the pedicle in the brow area to gain additional mobility and length to the flap. Thus the pedicle is advanced inferiorly below the bony orbital rim, adding some advancement to the main pivotal movement of the flap. The rhombic flap is another example in which both pivotal and advancement movements are important in transferring the flap to the recipient site. Most rotation flaps are also facilitated by advancement of their pivotal point. True advancement flaps have a linear configuration and are moved by sliding toward the defect. This involves stretching the skin of the flap. Thus, advancement flaps work best in areas of greater skin elasticity. The most basic advancement flap is the simple linear layered closure, which involves undermining and direct advancement of tissue side to side to close the defect primarily. This closure does not create a secondary defect, and additional incisions are made only for the removal of standing cutaneous deformities. However, the term advancement flap usually refers to a flap created by incisions that allow a “sliding” movement of the tissue. Tissue transfer is achieved by moving the flap and its pedicle in a single vector. The greatest wound closure tension is perpendicular to the distal border of the flap. Advancement flaps may be categorized as unipedicle, bipedicle, V-Y, Y-V, and subcutaneous tissue pedicled island flap (Table 9-1). By necessity, all advancement flaps must be designed so that the advancing border of the flap also represents a margin of the cutaneous defect that the flap is designed to repair. When an advancement flap is transferred to a defect, the motion of the flap is considered the primary tissue movement of the repair. Secondary tissue movement is the displacement of skin surrounding the defect toward the center of the primary defect (Fig. 9-1). Secondary movement always assists in wound closure by reducing wound closure tension. However, at times, secondary tissue movement may be detrimental if the defect is located near a mobile margin of a facial structure. Facial structures that are likely to be distorted if secondary tissue movement is excessive include the vermilion, nostril margin, lower and upper eyelids, and eyebrows. The stronger the attachments of facial structures to the underlying bone, the less propensity for distortion or displacement of these structures from secondary tissue movement. Complete undermining of advancement flaps as well as of the skin and soft tissue around the flap is likely to reduce wound closure tension and thus limit secondary tissue movement. If secondary movement could be beneficial in reducing wound closure tension and does not cause excessive distortion of facial landmarks, then wide undermining of the skin and mobilization of the tissue surrounding the defect are also indicated. At times it is preferable to allow movement only of the flap, in which case there should be limited or no undermining of the margins of the defect.
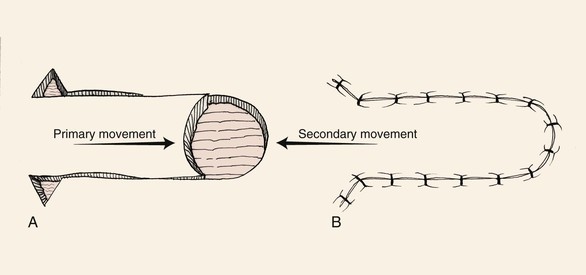
FIGURE 9-1 Unipedicle advancement flap. Primary and secondary skin movement occurs with wound repair.
All local flaps have inherent advantages and disadvantages, and these are often related to the flap design and the location where the flap is used. Certain cutaneous flaps work best in certain anatomic locations (see discussion of preferred flaps in Chapter 6). Advancement flaps are used for reconstruction of many surgical defects of the face. In considering the use of an advancement flap, it is important to consider the location of the vectors of wound closure tension and the location of incision lines and whether they respect relaxed skin tension lines (RSTLs) and aesthetic boundaries. The location where standing cutaneous deformities are likely to form and how they will be managed should be considered.1 Table 9-2 lists common locations on the face where advancement flaps are effective in repairing skin defects. As with all local flaps, it is important to evaluate the adjacent skin for matching qualities of texture, color, consistency, and hair growth.
Unipedicle Advancement Flaps
As the name implies, unipedicle advancement flaps have a single cutaneous pedicle. The flap is created by parallel incisions that allow a sliding movement of tissue in a single vector toward a defect. The movement is in one direction and flap advancement is directly over the defect. This form of wound repair is sometimes referred to as U-plasty. Complete undermining of the advancement flap as well as of the skin and soft tissue around the pedicle is important to enhance tissue movement. In contrast to pivotal flaps, which form a single standing cutaneous deformity, two deformities are created with all unipedicle advancement flaps. Unlike with pivotal flaps, in which the standing cutaneous deformity must be dealt with at the base of the flap, the deformities that develop from advancement can be excised anywhere along the length of the flap and not necessarily juxtaposed to the base. This is because of the mechanism of tissue movement.
Unipedicle advancement flaps and rotation flaps have one characteristic that is inherent only in these two flap designs. Owing to their specific design, the use of either type of flap creates a situation in which there exists an unequal length of the borders of the wound once the flaps are transferred to their respective recipient sites. This is because the peripheral border of the wound (flap incision plus defect width) is longer than the length of the flap. Triangular skin excisions along the periphery of the wound (equalizing or Burow triangles) in essence have the effect of shortening the peripheral border of the wound so that its length matches the length of the flap (see discussion in Chapter 7). In the case of rotation flaps, a single Burow triangle excision is required, whereas unipedicle advancement flaps require two excisions, one on either side of the flap. Excision of standing cutaneous deformities of advancement flaps is predicated on the most optimal site for excision. Typical excisions are placed in RSTLs or borders between aesthetic regions of the face. Sometimes the discrepancies in the length of the borders of the wound may be eliminated by a halving suture technique. The technique involves dividing in half the length of the wound repair with each consecutive suture. This evenly distributes the redundant tissue of the standing cutaneous deformities as small puckers along the entire length of the wound. Thus the redundancy is “sewn out” without the need for excision of skin.
Unipedicle advancement flaps are useful for repair of defects on the forehead. The flap is designed so that incisions are placed in or parallel to horizontal creases and, when possible, along the border of the eyebrow or anterior hairline. The unipedicle advancement flap should be conceptualized as rectangular in shape. Most cutaneous defects are round or oval, and a rectangular flap does not always precisely conform to a round defect. It may be necessary to modify the shape of the distal flap or the defect itself to minimize tissue distortion. It is usually preferable to “square off” the defect than to “round off” the flap. This is because angular incisions produce straight scars that have fewer propensities to develop trap-door deformities compared with curvilinear scars. Regardless of which option is selected, it is helpful to delay this modification until the flap has been elevated and has demonstrated its ability to cover the defect completely. Unipedicle advancement flaps are usually designed with parallel incisions extending from one border of the defect. However, these incisions are sometimes designed to diverge from each other when a greater width to the pedicle is desired or divergence can allow placement of incisions in facial aesthetic borders. Typically, unipedicle advancement flaps are designed with a ratio of defect width to flap length of 1 : 3.1,2 Therefore, large defects are more easily repaired with bilateral opposing flaps.
Bilateral Unipedicle Advancement Flaps
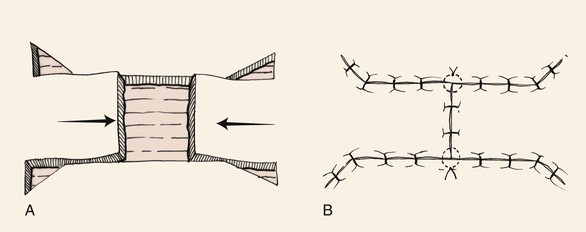
Bilateral unipedicle advancement flaps are commonly combined to close various defects, resulting in H- or T-shaped repairs, depending on the configuration of the defect and the number of incisions used. Repair in this manner is often referred to as H-plasty (Fig. 9-2) or T-plasty. In both cases, advancement flaps are incised on opposite sides of the defect and advance toward each other. Each flap is responsible for covering a portion of the defect. When standing cutaneous deformities require excision, they are excised either in the area of the defect or along the borders of the flaps. The two flaps do not necessarily have to be of the same length. Flap length is determined primarily by the elasticity and redundancy of tissue at the donor site. The basic principles of tissue movement and wound closure are identical to those for single unipedicle advancement flaps. When designing and dissecting the flaps, it is wise to first incise and elevate only one flap. On occasion, sufficient skin movement is achieved with a single flap so that the second flap is not necessary or can be designed with less length. Like single unipedicle advancement flaps, bilateral flaps are useful for repairing skin defects of the forehead, eyebrow, and ear. Bilateral advancement flaps are particularly helpful for repair of defects of the central lips and chin. The advantage of bilateral flaps over a single flap for repair of these midline structures is that equal “pull” from the two opposing flaps lessens tissue distortion and the propensity toward deviation of midline structures toward one side. Similar to single advancement flaps, bilateral flaps will create wounds of unequal length often requiring removal of Burow triangles. These triangles may vary in size and location, depending on the location of the flaps and the elasticity of the tissues (Fig. 9-3).2 For instance, Figure 9-3 shows Burow triangles removed at different locations above and below the two flaps. In theory, these locations correspond to areas that result in the best scar camouflage. Figure 9-3B shows half-buried mattress sutures placed at the site of the Burow triangle excisions. Inferiorly, a four-point corner stitch is used.
T-Plasty
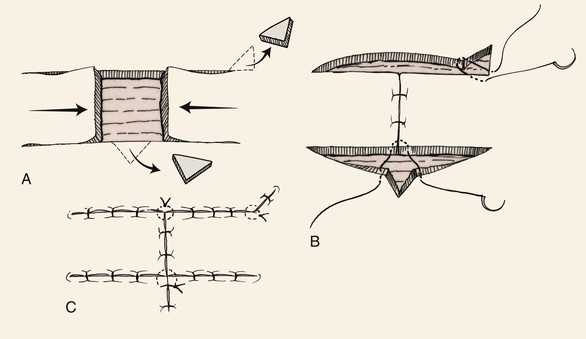
The A-T and O-T wound repair are so named because these methods transform a triangular (A-shaped) or round (O-shaped) defect into a T-shaped scar (Fig. 9-4). The T-plasty involves two flaps that are advanced in opposite directions toward each other. The standing cutaneous deformity that occurs to some degree with all advancement flaps is excised as the vertical limb of the T. If the horizontal limbs of the T-plasty are curved, flap movement is not solely advancement but a combination of rotation (pivotal movement) and advancement. T-plasty represents a modification of bilateral unipedicle advancement flaps. Instead of making two parallel incisions to create the flap, only one incision on opposing sides of the defect is made. The two flaps are advanced and slightly pivoted toward each other to repair the defect. A standing cutaneous deformity develops at the defect site opposite the position of the two incisions. This deformity is excised and the wound repaired, giving the final suture line a T configuration. The vertical limb of the T represents the excision of the standing cutaneous deformity. In addition, depending on the length of the incisions necessary to create the advancement flaps, standing cutaneous deformities may also form and require excision somewhere along the incision lines. An advantage of T-plasty repair is that the technique divides the defect in half by using two flaps for closure. Thus two smaller flaps can be used for repair instead of a single larger flap, which may be more difficult to harvest in areas where skin redundancy is limited. Another advantage of T-plasty is that only one incision is required to create each flap; thus fewer scars are created by not making parallel incisions to create the flaps as required for standard bilateral unipedicle advancement flaps. The horizontal limbs of the T-plasty can usually be positioned in natural creases or at junctions of aesthetic regions. T-plasty works very well for defects of the central forehead, where the vertical limb can be placed in the midline. The technique may also be used just above the eyebrow or on the temple adjacent to the hairline. In such cases, the horizontal component of the T is positioned along the lateral eyebrow or the anterior hairline. T-plasty is also an effective method of repairing cutaneous defects of the lateral lip adjacent to the vermilion (Fig. 9-5), the chin, and the preauricular and postauricular areas.3 When T-plasty is used to repair skin defects of the lips, excision of standing cutaneous deformities of the vermilion are not always necessary or can be made very small. In contrast, if primary repair is attempted, an excision of a large standing cutaneous deformity of redundant vermilion is required. T-plasty repair often eliminates this requirement and maintains the majority of incision lines on the cutaneous portion of the lip. Bilateral incisions are made along the vermilion margin at the base of the defect, thus creating two horizontal limbs of the T-plasty. The border of the defect opposite the vermilion is excised in a fusiform manner to remove a triangle of tissue. This triangle represents the standing cutaneous deformity that will form from advancement of the two flaps. The excision converts a round defect into a triangular defect (Fig. 9-5A). Wide undermining of adjacent skin is important to lessen wound closure tension, which in turn minimizes the risk of distortion of the philtrum. A four-point suture is placed in the midline of the base of the defect to precisely align the wound margins (Fig. 9-5B). When necessary, Burow triangles are removed along the border of the two flaps only after they have been advanced and secured. Schematically, small Burow triangles are removed at the most medial and lateral aspects of the horizontal limbs of the flaps (Fig. 9-5A). At times, because of the elasticity of lip skin, such triangles do not require excision. Instead, the triangles are sewn out by the principle of using halving sutures.3
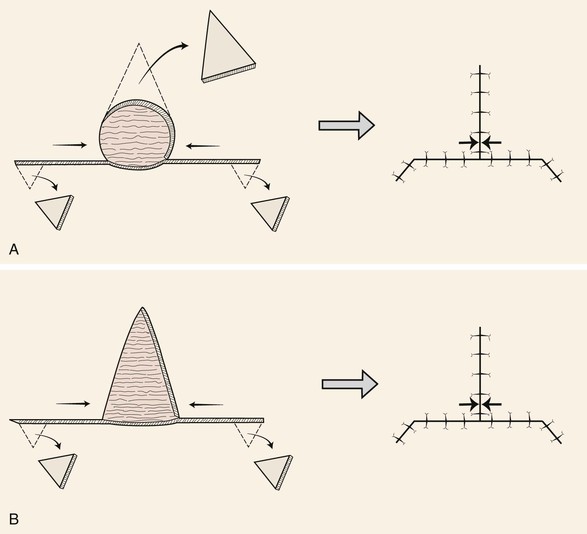
FIGURE 9-4 A, O-T (T-plasty) repair of circular (O-shaped) wound. T-plasty requires two flaps advanced in opposite directions toward each other. The standing cutaneous deformity forming superiorly from advancement is excised at vertical limb of T. B, A-T (T-plasty) repair of triangular (A-shaped) wound. Wound closure suture line has T-shaped configuration. Opposing arrows indicate point of greatest wound closure tension.
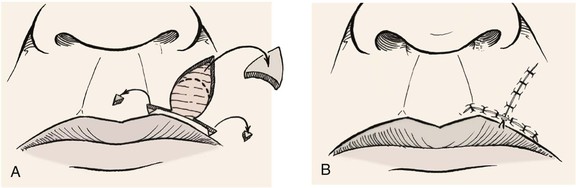
FIGURE 9-5 A, O-T (T-plasty) repair of circular defect of upper lip near vermilion-cutaneous border. B, T-shaped wound closure avoiding incisions into vermilion.
Figure 9-6A shows a typical round surgical defect above the left eyebrow, an area where the T-plasty repair works well. First, it is helpful to mentally superimpose a triangle over the circular defect. In reality, the circle is converted to a triangle by removal of wedges of tissue at the perimeter of the circle at three points equally separated from each other. In Figure 9-6A, note that the superior wedge is in the form of an M-plasty, which helps to minimize the length of the vertical limb of the scar. Two horizontal incisions are made perpendicular to the vertical limb to create advancement flaps. These incisions may be varied in length and may curve, allowing proper placement in RSTLs, such as the horizontal crease lines of the forehead. The flaps are then elevated and advanced into the primary defect, with the key suture being placed at the central advancing borders of the two flaps. Undermining should be sufficient to allow minimal wound closure tension. It is preferred not to excise the Burow triangles until complete undermining is accomplished and the flaps are advanced into the primary defect. Burow triangles are usually removed near the base of the flaps but, in actuality, can be removed from any area along the incision line if it hides well in RSTLs. A four-point suture is used to approximate the opposing distal tips of the two flaps and adjacent skin (Fig. 9-6B). The tip of the M-plasty is closed with a similar half-buried horizontal mattress tip suture. Repair is completed by suturing the flaps together by layered closure (Fig. 9-6C).
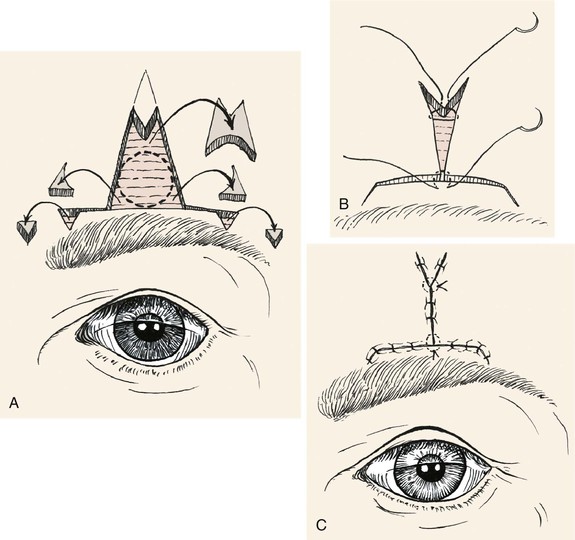
FIGURE 9-6 A, O-T (T-plasty) repair of circular skin defect near eyebrow. Wedges of skin removed from perimeter of circle. Superiorly, M-plasty limits vertical scar length. The Burow triangles are removed at end of horizontal limb of flaps. B, Half-buried horizontal mattress tip sutures. C, Wound closure with M-plasty avoids distortion of eyebrow.
Modified T-Plasty
The greatest problem with T-plasty repair of large (2 cm or greater) circular cutaneous defects of the lip is ectropion of the vermilion as the wound heals. This is due to the contracture of the vertical portion of the T-shaped scar. In addition, T-plasty flaps are not pure advancement flaps. Some pivotal movement occurs, and this causes a small reduction in effective flap length. This in turn causes shortening of the vertical wound closure line. To avoid vermilion ectropion, a modified T-plasty can be performed. Instead of excision of the standing cutaneous deformity that develops opposite the incision lines for the two opposing flaps, the tissue of the deformity is preserved and used to lengthen the vertical component of the T-plasty scar (Fig. 9-7). The two opposing borders of the flaps are first approximated at the vermilion line. The resulting standing cutaneous deformity that forms opposite the flap incisions is marked. Only half of the typical incision to excise the deformity is made. This creates a flap of skin that is pivoted and advanced into a second horizontally oriented incision made in the opposing lip segment. The orientation and length of the second incision are designed after the first incision creating the flap of skin has been performed. The flap is positioned over the adjacent lip segment, and the distal end of the overlapping flap is marked on the lip segment. A line is drawn from this point to the lip segment wound border. The line is angled so it is centered beneath the linear axis of the overlapping flap. An incision is then made along this line. The borders of the incision are undermined. The flap is then sutured into the recipient site created by the second incision. On occasion, a small portion of the flap must be trimmed to allow it to fit perfectly within the opposing lip segment. This technique in essence is a modified Z-plasty, which has the effect of lengthening the otherwise straight vertical component of the T-plasty scar. The vertical scar resulting from the modified T-plasty has an irregular Z-shaped configuration (Fig. 9-8).
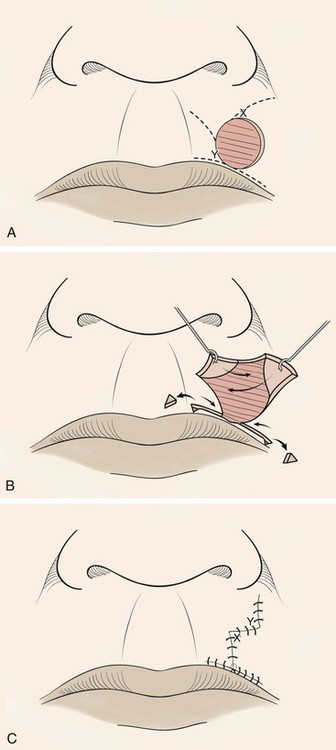
FIGURE 9-7 A, Modified O-T (T-plasty) repair of circular cutaneous defect of upper lip. Inferior broken lines indicate incisions to create advancement flaps as part of classic T-plasty repair. Superior broken lines indicate incisions to create transposition flaps for modified Z-plasty, which eliminates need to excise standing cutaneous deformity superiorly. B, Flaps incised and dissected, small standing cutaneous deformities excised from vermilion border if necessary. C, Wound repaired. Vertical component of scar has Z configuration.
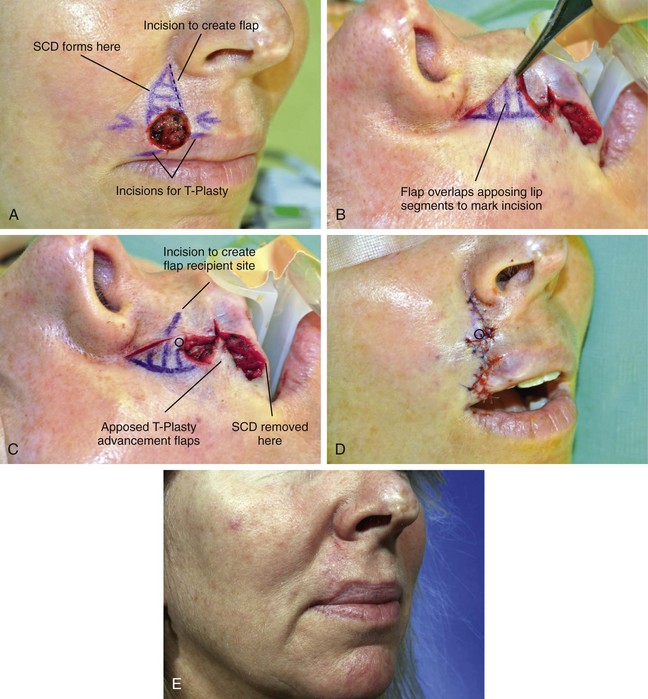
FIGURE 9-8 A, A 1.5 × 1.2-cm circular cutaneous defect. Modified T-plasty designed for wound repair. Broken line indicates planned incision along border of anticipated standing cutaneous deformity (SCD). B, Flap created by incision marked by broken line in A overlaps medial lip segment to mark incision for recipient site. C, Incision marked to create recipient site for flap. Distal tip of flap marked with circle. D, Flap transposed to create modified Z-plasty vertical wound repair. Circle marks distal end of flap. E, Postoperative view at 2 months.
V-Y and Y-V Advancement Flaps
Like the T-plasty, V-Y and Y-V advancement flaps do not require two parallel incisions to create the flap (see discussion of these flaps in Chapter 6). The V-Y advancement flap is unique in that the V-shaped flap is not stretched or pulled toward the recipient site but rather achieves its advancement by recoil or by being pushed forward. Thus the flap is allowed to move into the recipient site in a nearly tension-free fashion. The secondary triangular donor defect is then repaired with wound closure tension by advancing the two borders of the remaining wound toward each other. In so doing, the wound closure suture line assumes a Y configuration, with the common limb of the Y representing the suture line resulting from closure of the secondary defect. The flap is optimally designed so that the common limb of the Y falls in the boundary of neighboring aesthetic regions or within a natural crease, fold, or wrinkle.
V-Y advancement is useful in situations in which a structure or region requires lengthening or release from a contracted state. The technique is particularly effective in lengthening the columella during the repair of cleft lip nasal deformities in which a portion or all of the columella is underdeveloped. A V-Y advancement flap is elevated recruiting skin from the midportion of the lip between the philtral ridges. The length of the columella is augmented by advancement of the flap upward into the base of the columella (Fig. 9-9). The secondary donor defect is approximated by advancement of the remaining lip skin together in the midline. V-Y advancement is helpful in releasing contracted scars that are distorting adjacent structures, such as the eyelid or vermilion. An example is the correction of an ectropion of the vermilion caused by scarring. The segment of distorted vermilion is incorporated into the V-shaped flap and the flap is advanced toward the lip to restore the natural topography of the vermilion-cutaneous junction. The secondary defect is closed by advancement. The suture line resulting from closure of the secondary defect becomes the vertical component of the Y configuration (Fig. 9-10).
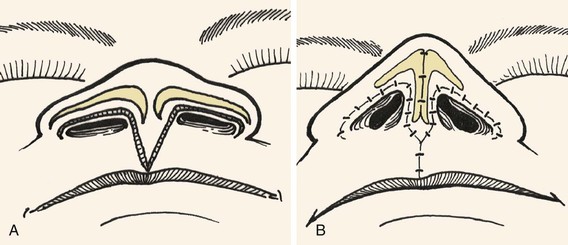
FIGURE 9-9 A, B, V-Y advancement flap dissected from philtrum by recruiting skin from midportion of lip between philtral ridges. Length of columella augmented by advancement of flap superiorly into base of columella.
Bipedicle Advancement Flaps
Bipedicle advancement flaps are used primarily for repair of large defects of the scalp. The flap is designed adjacent to the defect and is advanced into the defect at a right angle to the linear axis of the flap. This leaves a secondary defect that usually must be repaired with a split-thickness skin graft. As a consequence, bipedicle flaps are rarely used for reconstruction of the face and neck. The exception to this is bipedicle nasal vestibular skin advancement flaps used for lining full-thickness nasal defects of the hemi-tip or ala that have a vertical height of no more than 1.0 cm (see discussion of this flap in Chapter 18). The flap consists of vestibular skin and mucosa based medially on the septum and laterally on the floor of the nasal vestibule. An extended intercartilaginous incision is made and the flap is elevated off the undersurface of the alar cartilage and mobilized inferiorly to line the ala or hemi-tip. The donor site on the ventral aspect of the cartilage is covered with a thin full-thickness skin graft. The bipedicle flap is thin and provides natural physiologic material for the interior of the nasal passage with sufficient vascularity to support the concomitant use of free cartilage grafts placed over the lining flap for structural support of the construction.
Applications
Forehead
A general discussion of surgical techniques and preoperative and postoperative surgical care of patients undergoing local flap reconstruction is provided in detail in Chapters 4 and 5. The most effective technique for reconstruction of forehead cutaneous defects usually involves one or more advancement flaps. In spite of the relative inelasticity of forehead skin, the use of advancement flaps versus pivotal flaps is preferred because they typically produce the best aesthetic results. This is because incisions necessary for advancement flaps may be placed in the horizontal creases of the forehead or along the border of the eyebrow, depending on the location of the defect. Transposition flaps work well in the region of the temple, but more medially on the forehead it becomes difficult to close the donor site when such flaps are used.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses