Vital pulp therapy
The aim of this chapter is to outline the technical and clinical elements of prevention and management of pulp disease. The rationale was established in Chapter 2. The general principles of disease management covered previously apply equally well to the primary and secondary dentitions as will be evident from Chapter 1. However, primary teeth bring special challenges of management and are covered here first before describing the management of secondary permanent teeth.
Morphology of primary teeth
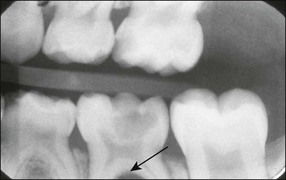
The enamel and dentine of primary teeth are thinner and the pulp chamber, with its extended horns, larger in proportion than in permanent teeth (Fig. 7.1). Caries progresses relatively more rapidly to the pulp in the primary dentition.
Primary molars have irregularly shaped ribbon-like root canals with lateral branches. The floor of the pulp chamber is thin and there are numerous accessory canals in the interradicular area. The permeability of the dentine in this region often leads to interradicular rather than periapical bone loss associated with infected primary molars (Fig. 7.2).
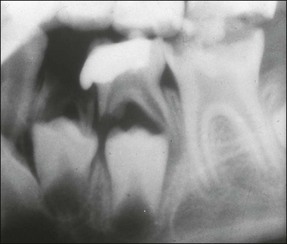
The roots of the primary teeth are in close relationship to the developing permanent successor and will undergo physiological resorption during the process of exfoliation (Fig. 7.3). Materials used within the root canal system must, therefore, also be resorbable. Their close proximity means that trauma to, or infection of, primary teeth may affect the developing successor. Possible sequelae include enamel defects, arrested development or cyst formation.
Pulp disease in primary teeth
Inflammatory pulpal changes in response to caries occur more rapidly in primary teeth compared to permanent teeth, soon becoming irreversible. Symptoms from such pathological changes in primary teeth may not become severe until the later stages of necrosis and abscess formation (Fig. 7.4).
Diagnosis of pulp disease in young children is complicated by their inability to articulate the problem, which is difficult enough for an adult (see Chapter 4); furthermore, they may respond unpredictably to subjective clinical tests. Techniques used in the management of pulp disease in permanent teeth cannot, therefore, be reliably used in the primary dentition. Methods of objectively measuring inflammatory changes in the pulps of primary teeth by molecular (e.g., prostaglandin) assays are under assessment but not yet ready for implementation.
Techniques of pulp therapy
Direct pulp capping
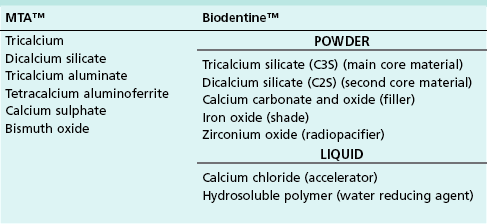
This technique is generally contraindicated for the primary dentition. Pathological changes progress rapidly within the pulps of primary teeth and their healing ability is limited. Pulpal inflammation usually persists and progresses to internal root resorption and then necrosis, particularly when calcium hydroxide is used to dress the exposed pulp (Fig. 7.5). Use of the technique may be justified in exceptional circumstances, such as to manage a small traumatic exposure in otherwise sound dentine during cavity preparation. Haemorrhage from the exposure should be minimal and easily controlled by gentle application of a cotton pledget soaked in sterile water/saline. Further haemorrhage would indicate more severe pulpal inflammation and pulpotomy would be the treatment of choice. If the bleeding is easily arrested, calcium hydroxide or mineral trioxide aggregate (MTA) (Table 7.1) may be used to dress the wound, followed by tooth restoration.
Biodentine™, which is a new biocompatible and bioactive calcium silicate based material (see Table 7.1), has been advocated for use as a dentine “replacement”, as well as a direct pulp capping agent. It has been shown to have the potential to induce transforming growth factor β1 (TGF-β1) release from human pulp cells and early dental pulp mineralization but further laboratory and long-term clinical outcome studies are required.
Vital pulpotomy
The indications for pulpotomy in a restorable tooth include absence of the following: spontaneous or persistent pain, abscess or sinus, interradicular bone loss, or internal resorption. It may also be used to avoid extraction, such as in the area of a haemangioma or child with a bleeding disorder.
Procedure: quick reference guide
1. Adequate local analgesia and isolation, preferably with a rubber dam, are essential. All peripheral caries should be removed prior to entering the pulp chamber. The pulp chamber is then entered via the exposure (Figs 7.6, 7.7).
2. The entire roof of the pulp chamber is removed to leave no overhangs so that removal of the pulp tissue is not compromised. It is important at this stage that the bur is not taken any deeper into the cavity, since this would endanger the thin floor of the pulp chamber (Figs 7.8, 7.9).
3. The coronal pulp is removed using a large sharp excavator or round bur. The chamber is irrigated with saline and moist cotton wool pledgets are applied to control haemorrhage and identify the pulp stumps (Figs 7.10, 7.11).
4. If haemostasis is not readily achieved, 15.5% ferric sulphate solution is applied to the pulp stumps with a microbrush for 15 seconds followed by thorough rinsing and soaking up of excess moisture with a slightly moist cotton pledget. Diluted (0.5%) sodium hypochlorite solution may also be applied to achieve haemostasis; persistent haemorrage at this stage indicates residual pulp inflammation and pulpectomy or extraction should be followed.
5. On removal of the cotton wool, the radicular pulp stumps should appear bright or dark red without haemorrhage (Figs 7.12, 7.13).
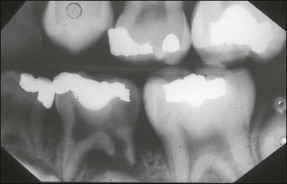
6. Once haemorrhage has been arrested, MTA mixed with sterile water to a “wet sand” consistency is then applied over the radicular pulp and the tooth definitively restored with glass ionomer cement and a stainless-steel crown (Figs 7.14, 7.15).
Restoration of endodontically treated primary teeth
Endodontically treated primary teeth are weakened by the destruction of tooth tissue during preparation. It is important that the definitive restoration has the necessary strength to support the tooth structure and provides an adequate seal following the endodontic treatment. For these reasons, the most suitable restorations are stainless-steel crowns for posterior teeth and composite-resin strip crowns for anterior teeth (Figs 7.16–7.19). The reader is referred to other texts for details of the techniques.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses