Chapter 8
Temporomandibular Joint
Felipe Porto
Department of Oral Health and Diagnostic Sciences, School of Dental Medicine, University of Connecticut
The temporomandibular joint (TMJ) is the joint where the mandible articulates with the cranium (Fig 8.1). The following characteristics make the TMJ a complex and unique joint:
- It is classified as a compound joint even though it does not include three bone structures in the articulation. However, the articular disc, which is interposed between the condylar head of the mandible and the squamous portion of the temporal bone, is considered as a third bone (even though it is not a bone, but a dense fibrous connective tissue).
- It is considered a ginglymoarthrodial joint due to the fact it combines hinge (pivoting) and gliding (sliding) movements.
- The TMJ on one side cannot work independently from the joint on the other side.
As mentioned, the TMJ includes the temporal bone, the mandible, and an articular disc composed of fibrous connective tissue. Before discussing details of the function of the TMJ, it is important to describe the structure of the components of this joint.
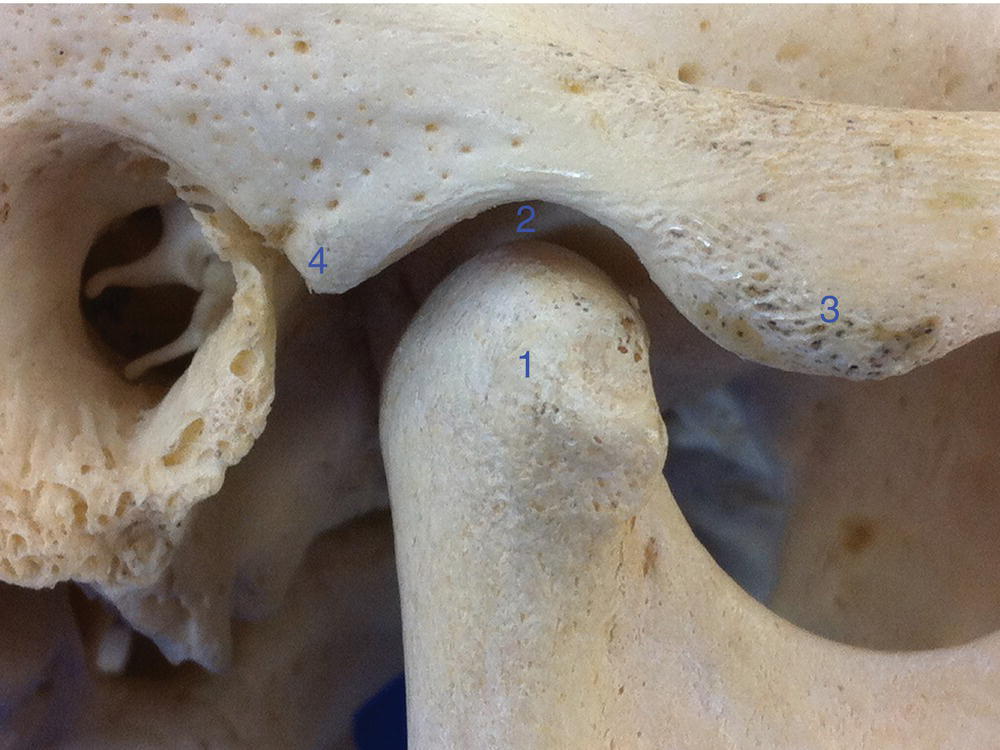
Figure 8.1 Bony structures of the TMJ (right side): (1) Condyle; (2) mandibular fossa; (3) articular eminence; (4) postglenoid process.
Structure of the TMJ
Temporal bone
The areas of the temporal bone that are of interest for the TMJ are the mandibular fossa and the articular eminence. The mandibular fossa, also called the articular fossa or glenoid fossa, is a concave area in the squamous portion (squama) of the temporal bone, limited anteriorly by the articular eminence and posteriorly by the postglenoid process, which is localized immediately anterior to the external acoustic meatus. The articular eminence is a convex bar of bone upon which the articular disc slides during mandibular function (Fig 8.2).
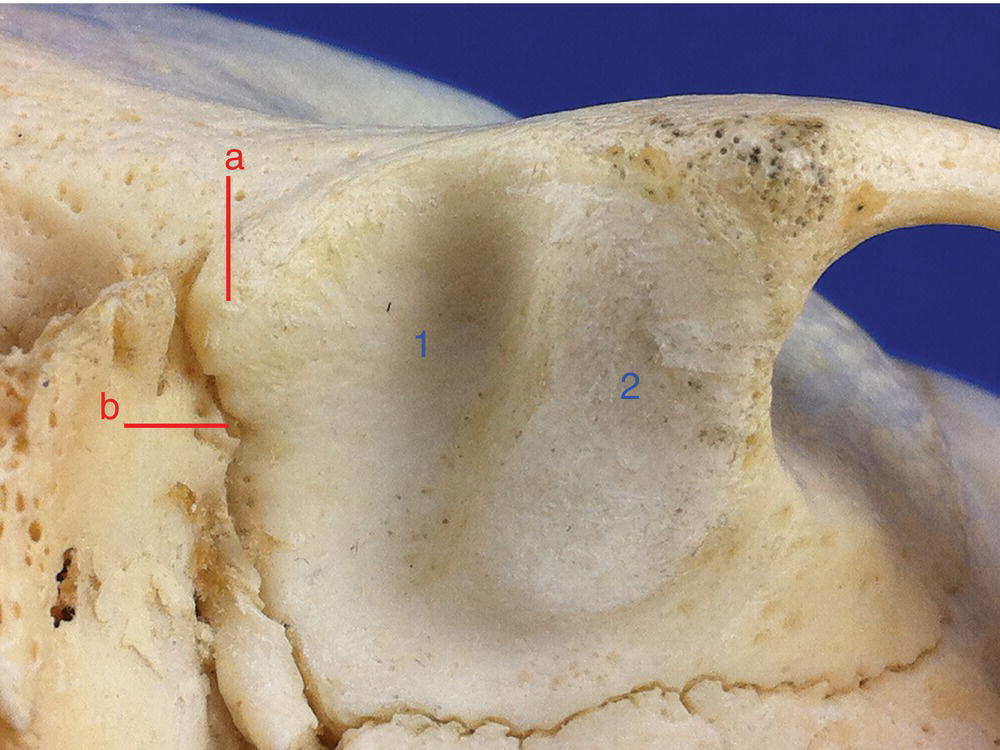
Figure 8.2 Inferior view of the mandibular fossa (1) and the articular eminence (2). Also note the postglenoid process (a) and the squamotympanic fissure (b).
Mandible
The mandible is a horseshoe-shaped bone which holds the lower teeth. It is largely formed from an intramembranous ossification. The condylar process, the anterior border of the coronoid process, and the mental process are formed by endochondral ossification. The mandible is stabilized only by soft tissue (including mainly muscles and ligaments) and it has no direct bony connections to the skull.
The area of the mandible that is of direct interest of the TMJ is the condylar head or condyle, which articulates with the temporal bone.
On the coronal plane the condyle is observed to have two poles, the lateral pole and the medial pole; the latter is more prominent, extending farther beyond the neck of the condyle (Fig 8.3). On a transverse plane the medial pole is positioned slightly more posterior than the lateral pole, and therefore when a long axis line connecting the two poles is drawn it will be medially directed to the anterior border of the foramen magnum (Fig 8.4). The anterior surface of the condyle is concave while the posterior surface is convex.

Figure 8.3 Right condyle (anterior view): (1) lateral pole; (2) medial pole; also note the neck of the condyle (3).
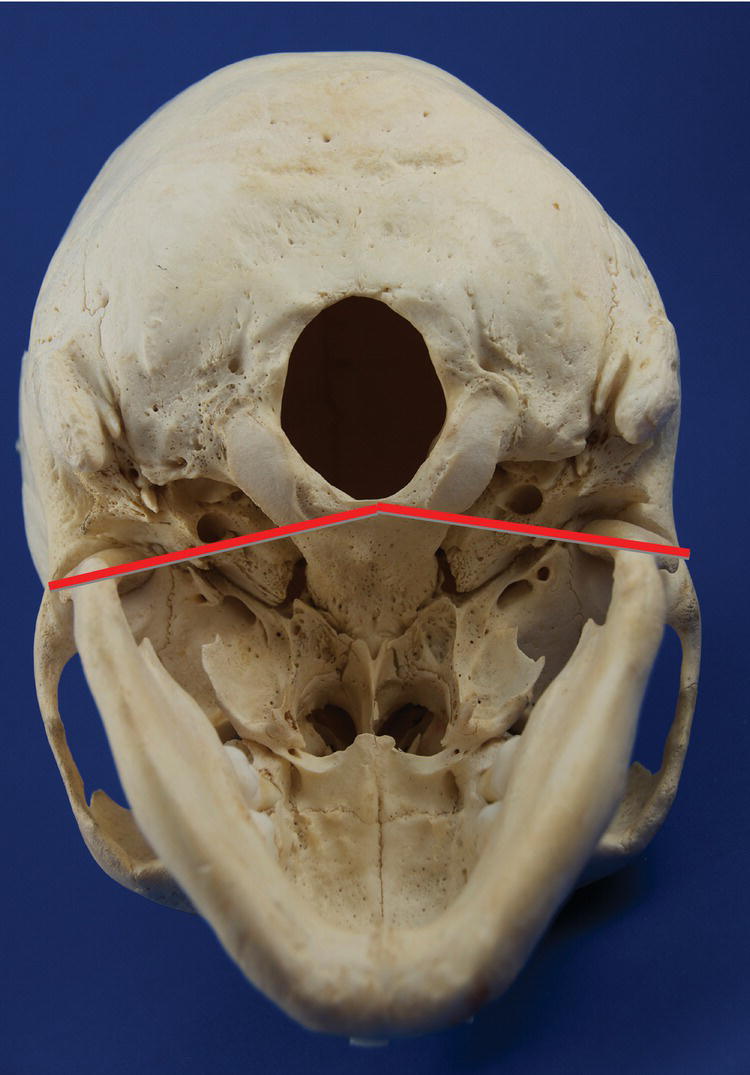
Figure 8.4 Base of the cranium (transverse plane, inferior view), showing that the imaginary lines connecting the medial and lateral poles of the condyles are posteriorly and medially directed toward the anterior border of the foramen magnum.
Articular disc
The articular disc is interposed between the condyle and the mandibular fossa. It is composed of a dense fibrous connective tissue (type I collagen), and it is only innervated on its periphery. Behind the disc, however, there is a well-vascularized and innervated tissue called retrodiscal tissue, which when loaded can elicit pain. On the sagittal plane the disc can be divided into three distinct regions: the posterior region, which is the thickest one; the central region or intermediate zone, which is the thinnest area; and the anterior region. Ideally the condyle should be positioned on the intermediate zone (Fig 8.5).
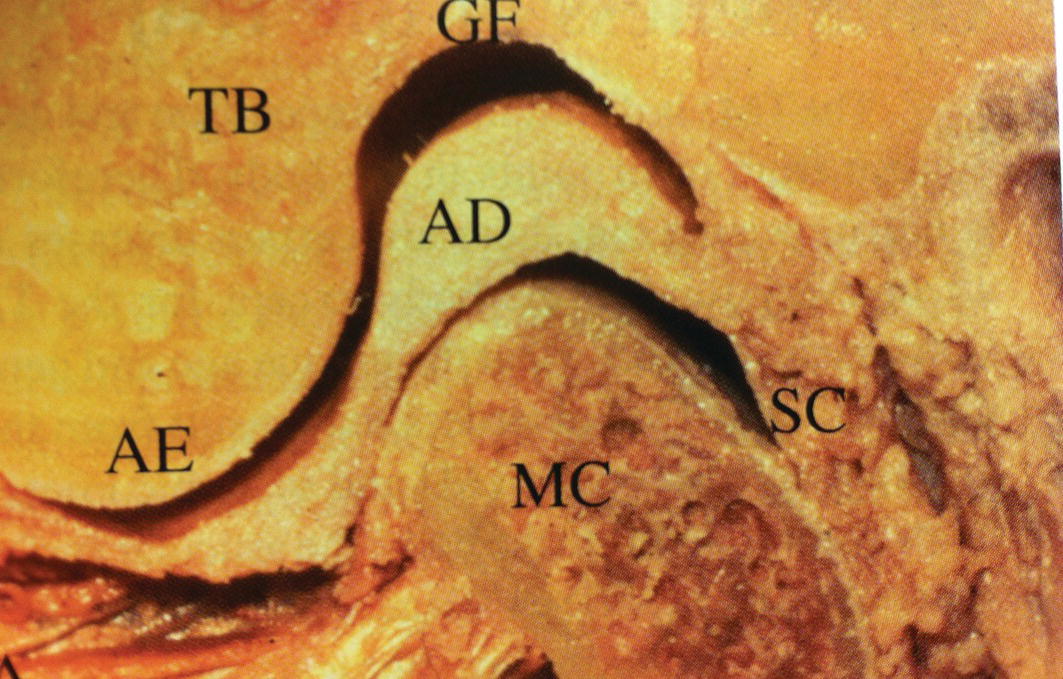
Figure 8.5 Bony components and articular disc of the TMJ: glenoid or mandibular fossa (GF), temporal bone (TB), articular disc (AD), articular eminence (AE), mandibular condyle (MC), and synovial capsule (SC). Note the three portions of the disc—the condyle is positioned on the intermediate zone.
(From: Wadhwa, S. & Kapila, S. (2008) TMJ disorders: future innovations in diagnostics and therapeutics. Journal of Dental Education, 72, 930–947.)
The disc is attached posteriorly to the retrodiscal tissue, which is bordered superiorly by the superior retrodiscal lamina (SRL), and inferiorly by the inferior retrodiscal lamina (IRL). The SLR consists of connective tissue with many elastic fibers. Both the IRL and SRL attach to the articular disc. Unlike the SRL, the IRL is formed by collagenous and nonelastic tissue.
The anterior capsular ligament attaches the disc anteriorly to the anterior margin of the articular surface of the temporal bone (superiorly) and to the anterior margin of the articular surface of the condyle (inferiorly). In between the superior and inferior portions of the anterior capsular ligament, the disc is also attached to the superior lateral pterygoid muscle (Fig 8.6).
Finally, the disc is also attached to the lateral and medial pole of the condyle through the lateral discal (or collateral) ligament and medial discal (or collateral) ligament, respectively (Table 8.1).
Table 8.1 Attachments of the articular disc
| Attachment | Localization | To |
| Superior retrodiscal lamina | Posterior superior | Squamotympanic fissure |
| Inferior retrodiscal lamina | Posterior inferior | Periosteum of the neck of the condyle |
| Retrodiscal tissue | Posterior | —- |
| Anterior capsular ligament (superior portion) | Anterior superior | Anterior margin of the articular surface of the temporal bone |
| Anterior capsular ligament (inferior portion) | Anterior inferior | Anterior margin of the articular surface of the condyle |
| Superior Lateral Pterygoid | Anterior | Infratemporal surface of the greater sphenoid wing |
| Lateral discal ligament | Lateral | Lateral pole of the condyle |
| Medial discal ligament | Medial | Medial pole of the condyle |
As mentioned, the disc is completely surrounded by attachments, therefore creating two separated spaces: the superior articular space (or superior joint cavity), where the translation between the disc and the mandibular fossa/articular eminence occurs; and the inferior articular space (or inferior joint cavity), where the rotation between the condyle and the disc occurs (Fig 8.6). The superior space is delineated by the mandibular fossa and by the superior surface of the articular disc. The inferior space is delineated by the inferior surface of the articular disc and the mandibular condyle. The synovial fluid fills both articular spaces (Fig 8.7 and Fig 8.8).
Figure 8.6 TMJ on the sagittal plane view: (a) closed-mouth and (b) open-mouth. (1) Retrodiscal tissue, (2) superior retrodiscal lamina, (3) inferior retrodiscal lamina, (4) superior joint cavity, (5) articular disc, (6) inferior joint cavity, (7 and 8) anterior capsular ligament, (9) superior lateral pterygoid muscle, and (10) inferior lateral pterygoid muscle.
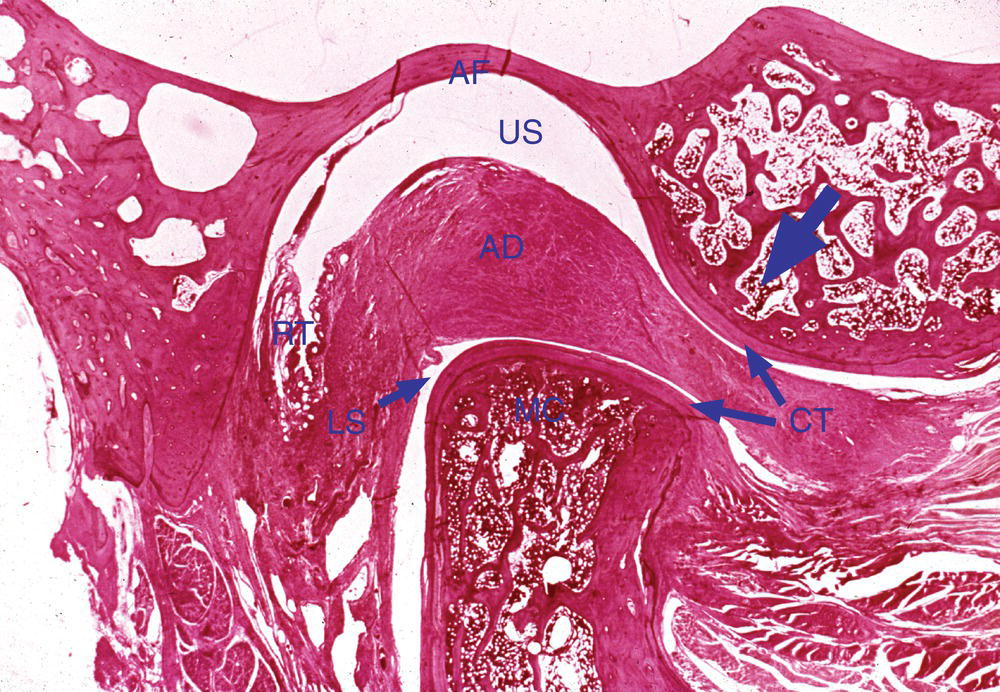
Figure 8.7 Very low-power photomicrograph of the temporomandibular joint sectioned in a sagittal plane. The articular fossa (AF) and articular eminence (indicated by the blue arrow) are visible above, and the head of the condyle (MC) below. The articular disc (AD)—an extension of the fibrous capsule surrounding the joint—separates the two bony surfaces. Notice that a layer of dense connective tissue (CT) covers the surfaces of both the temporal bone and the condyle. The condyle is approximately in its physiological position, riding on the posterior slope of the articular eminence rather than in the depth of the articular fossa. Only a thin layer of bone separates the articular fossa from the cranial cavity. Note the retrodiscal tissue (RT) located posterior to the condyle.
(From Moss-Salentijn, L. (1972) Orofacial Histology and Embryology: A Visual Integration. Reproduced with permission from F.A. Davis Company, Philadelphia, PA.)
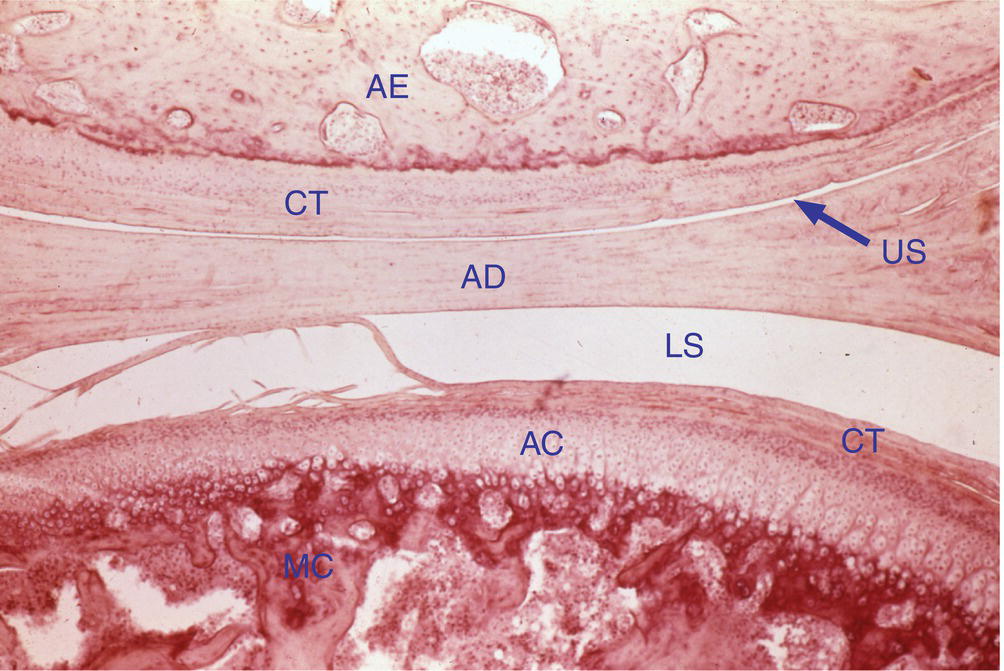
Figure 8.8 A low-power photomicrograph of a temporomandibular joint from an adolescent monkey. The bone and covering connective tissue (CT) of the articular eminence (AE) are above, the disc (AD) near the center, and the condyle (MC) below. The dense CT covering the articular cartilage (AC) of the condyle is quite thick. Some alignment of the cartilage cells into columns is visible in the cartilage, although a continuous layer of bone appears to cover its lower surface, indicating that growth in this joint is just now ceasing. Upper joint space (US) and lower joint space (LS).
Synovial fluid
Synovial fluid is secreted by cells of the synovial lining, and it serves not only as a lubricant minimizing friction upon articular movement but also supports the metabolic exchange among the capsule, the articular tissues, and the synovial fluid itself.
The synovial fluid lubricates the TMJ by two different mechanisms: boundary lubrication and weeping lubrication.
Boundary lubrication occurs when the joint is moved, thereby forcing the synovial fluid to relocate from one area of the joint to another. This mechanism prevents friction in the moving joint.
The second mechanism of lubrication is called weeping lubrication. The weeping lubrication is related to the ability of the articular surfaces to absorb a small volume of synovial fluid. Upon function, compressive force occurs on the articular surfaces of the joint, forcing the small volume of synovial fluid to be released. It is important to note that prolonged compressive forces to the articular surfaces will deplete the small amount of synovial fluid.
The boundary lubrication is related to joint movements while the weeping lubrication is related to compressive forces on the articular surfaces of the joint.
The synovial fluid contains hyaluronic acid (HA), which is important to maintain the lubrication capability of the synovial fluid. The hyaluronic acid is easily degraded under inflammatory conditions, and when degraded it does not prevent lysis of the phospholipids by phospholipase A2 (PLA2). The phospholipids cover the articular surfaces facilitating the sliding movement, therefore when they are broken down the friction between the articular surfaces increases.
Capsule and ligaments
A fibrous nonelastic membrane called the capsule or capsular ligament surrounds the TMJ. The capsule of the TMJ serves to resist any forces that tend to separate the articular surfaces (Fig 8.9). The capsule also retains the synovial fluid. Even though some authors recognize the disc as an extension of the capsule, the capsule is well innervated, unlike the disc that is almost completely devoid of nerve supply (except for its periphery). The inner surface of the capsule is lined by synovial membrane.
Figure 8.9 Capsule.
Two other functional ligaments support the TMJ: the discal or collateral ligaments and the temporomandibular ligament.
The discal ligaments, as mentioned previously, attach the medial and lateral edge of the disc to the respective poles of the condyle (Fig 8.10). The discal ligaments do not stretch since they are composed of connective tissue fibers, but they allow the articular disc to slide anteriorly and posteriorly on the articular surface of the condyle. Like the capsule, the discal ligament is innervated and vascularized and can cause pain when injured.
Figure 8.10 Discal ligaments (anterior view): (1) lateral discal ligament and (2) medial discal ligament.
The temporomandibular ligament consists of two portions: an outer oblique portion (OOP) and an inner horizontal portion (IHP). Both originate at the outer surface of the articular eminence and zygomatic process. The OOP extends posteroinferiorly to the outer surface of the condylar neck, and the IHP extends backward to the lateral pole of the condyle and posterior portion of the disc (Fig 8.11).
Figure 8.11 Temporomandibular ligament (lateral view): (1) Inner horizontal portion and (2) outer oblique portion.
The directions of the ligament’s portions help one to remember their functions:
- The OOP resists excessive inferior displacement of the condyle and limits the amount of rotation that the condyle can undergo in a fixed point, forcing the condyle to start the translation movement if wider opening is needed.
- The IHP restricts posterior displacement of the condyle–disc complex, protecting therefore the retrodiscal tissue.
- Finally, since both TMJs work simultaneously the temporomandibular ligament prevents lateral dislocation of one joint and medial dislocation of the opposite joint.
The TMJ also has two accessory ligaments: the sphenomandibular ligament and the stylomandibular ligament. The sphenomandibular ligament attaches the spine of the sphenoid bone to the lingula on the ramus of the mandible, while the stylomandibular ligament runs from the styloid process to the angle of the mandible.
Innervation and vascularization of the temporomandibular joint
The innervation of the TMJ is provided mainly by the auriculotemporal nerve, however, two other nerves also innervate the TMJ: the deep posterior temporal nerve and the masseteric nerve. The majority of nerve endings in the TMJ are free nerve endings, but Ruffini’s nerve endings, Golgi-Mazzoni corpuscles, and Pacinian corpuscles also are present.
The blood supply of the TMJ is more complex than the innervation. Many vessels supply the TMJ: the superficial temporal artery, internal maxillary artery, meningeal artery, deep auricular artery, anterior tympanic artery, and ascending pharyngeal artery. It is important to note that the vascular supply of the condyle comes from its marrow spaces (via the inferior alveolar artery) and via feeder vessels originating from larger vessels.
TMJ histology
Four layers constitute the articular surfaces of the condyle and the posterior slope of the articular eminence: the articular zone, proliferative zone, fibrocartilaginous zone, and calcified cartilage zone (Fig 8.12).
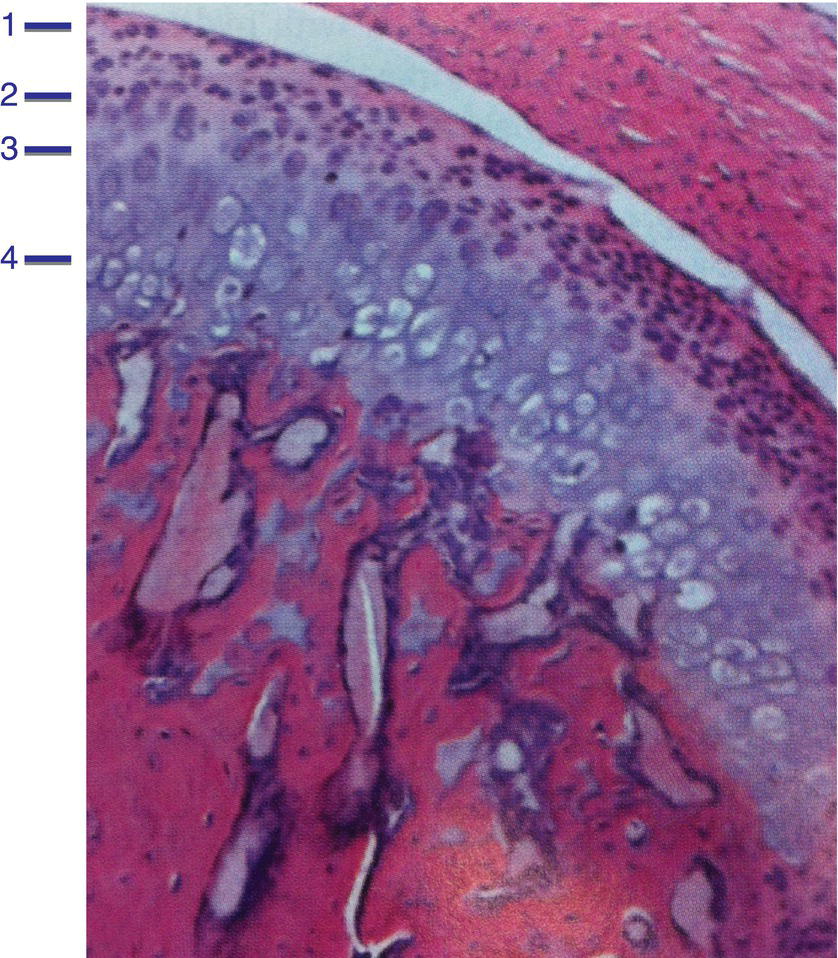
Figure 8.12 Histologic section of the mandibular condylar cartilage showing the four distinct zones: (1) articular zone, (2) proliferative zone, (3) fibrocartilaginous zone, and (4) calcified cartilage zone.
(From: Wadhwa, S., & Kapila, S. (2008) TMJ disorders: future innovations in diagnostics and therapeutics. Journal of Dental Education, 72, 930–947.)
The articular zone is the most superficial layer. This zone is able to dissipate the frictional loads during jaw function due to the fact it contains superficial zone proteins (SZP), which also are present at the superficial layer of the disc. The SZP are synthesized and secreted in the synovial fluid, which is responsible for boundary lubrication. This articular layer of the condyle and the posterior slope of the articular eminence is composed of dense fibrous connective tissue in contrast to most of the synovial joints, which are composed of hyaline cartilage. This characteristic is beneficial to the TMJ, since the dense fibrous connective tissue supports more loading than the hyaline cartilage, is less susceptible to breakdown, and presents better capability for repair (Fig 8.13). At the mandibular fossa level this fibrous layer is thinner than at the posterior slope of the articular eminence.
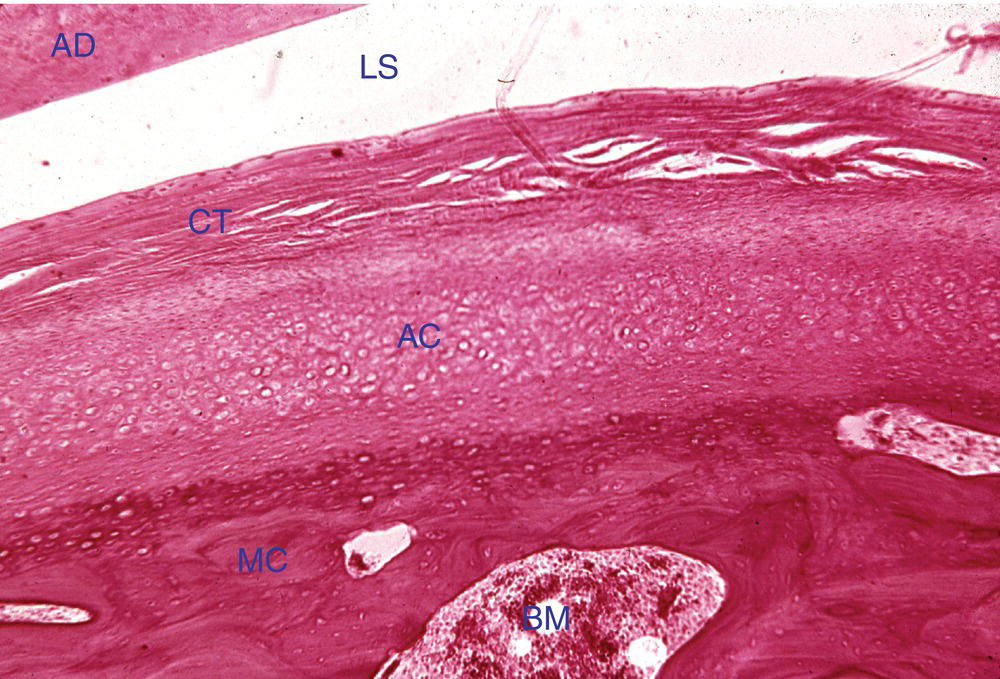
Figure 8.13 Photomicrograph of the head of the mandibular condyle. The bone (MC) is covered by a layer of cartilage (AC), and the cartilage is covered by a layer of dense, irregular fibrous connective tissue (CT). This is an adult condyle and no evidence of growth is visible. Articular disc (AD), lower joint space (LS), and bone marrow (BM).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


