8
Multidisciplinary Team Management of Congenital Orofacial Deformities
Summary
The term ‘craniofacial anomalies’ describes a diverse group of dysmorphic congenital disorders involving abnormalities of craniofacial development that vary from minor changes in the facial features to major abnormalities of craniofacial skeleton and its appendages: that is, ranging from simple craniosynostosis involving single fusions and simple clefts of the lip and palate to complex syndromes marked by multiple sutural fusions, complex facial clefts, branchial arch syndromes, gene depletions, gene mutations, and many more.
The management of children with complex craniofacial anomalies requires the skills of a variety of medical and dental professionals, and includes observation and assessment of their development, and formulation of a comprehensive treatment plan. These children need to be under constant care of this team from birth to adolescence or even beyond. With the emergence of craniofacial orthodontics, orthodontists have become an integral part of the team, providing skills to modify the growth and development of these inherently anomalous conditions. The value brought by the orthodontist to the craniofacial surgery team is clearly enunciated by McCarthy (2009) in his statement that ‘no other field of endeavor has brought the medical and dental professions closer together.’
This chapter aims to provide a concise description of the commonly encountered craniofacial anomalies and their multidisciplinary management.
Introduction
Craniofacial orthodontics, an emerging and challenging field, demands creative and innovative thinking to deal with often unique and very difficult clinical problems. According to the American Dental Association, craniofacial orthodontics is the area of orthodontics concerned with the management of patients with congenital and acquired deformities of the integument and its underlying musculoskeletal system within the maxillofacial area and associated structures (Santiago and Grayson, 2009). The world of craniofacial anomalies is complex and children with craniofacial anomalies show wide variations in their cranial and facial features. Management of these anomalies requires expertise as it involves trying to establish a normalcy which was never there. Comprehensive and coordinated care from infancy through adolescence is essential in order to achieve an ideal outcome, and thus people with formal training and experience in all phases of care must be actively involved in the planning, treatment, and long-term follow-up of these patients (Kapp, 1979; Kapp-Simon, 1995).
The presence of a craniofacial anomaly has a devastating effect on the child and the parents. The complex etiology and involvement of multiple anatomical regions complicate the management and necessitate establishment of centralized units to deliver a team-oriented or interdisciplinary approach as the standard of care. With the advances in intrauterine imaging, early identification of congenital deformities is now possible. However, this finding is usually a source of significant concern to the parents psychologically, and numerous centers have established counseling and family support groups. These support groups educate and reassure the parents that their baby will be well cared for in a structured team environment over a number of years, from birth to adulthood. This gaining of trust of the parents forms an essential component of the integrated team approach, because parents need to be active participants in the treatment protocol, and prepare themselves and their child to confront the challenges that might arise in the ensuing years. Parents appreciate discussing issues with others who have had similar experiences, and reviewing pre- and post-treatment records (M Goonewardene, personal communication, 2010). This approach adds to the complex interdisciplinary interaction, which aims to achieve a more complete integration of all parties concerned with care and attention of the needs of the extended family.
A significant number of medical and dental specialties play important roles throughout the course of treatment of the patient with a congenital craniofacial deformity. The initial acute needs are addressed by the neurosurgeon, neonatologist, pediatric surgeon, and a special nursing unit, but the orthodontist and craniofacial surgeon are often also involved early in the course of care. Additional specialist clinicians may play roles at specific times appropriate for the patient’s specific needs. These needs are determined and constantly reviewed at regular team meetings of the interdisciplinary group, and this excellent level of coordinated communication is the keystone to interdisciplinary-based, interactive care.
As almost all of the craniofacial anomalies involve jaw deformities, which are amenable to timely functional orthopedic and orthodontic treatments, orthodontists play an intrinsic role in their management (McCarthy, 2007). For example, they are actively involved in infant presurgical orthopedics, early mixed dentition treatment, dentofacial orthopedics and orthodontics, adolescent/adult orthodontics, preprosthetic orthodontics, and pre- and postsurgical orthodontics. The present chapter provides an overview of interdisciplinary team management of the most common craniofacial malformations (except cleft lip and palate, which is covered in Chapter 9). For the purpose of this chapter, the major congenital orofacial malformations are considered under the headings of otofacial malformations, craniosynostosis, achondroplasia/FGFR3 mutations, and holoprosencephalic disorders.
Otofacial Malformations
Craniofacial/Hemifacial Microsomia
This term describes a sporadic, complex spectrum of congenital anomalies that primarily involve the jaws, other skeletal components, muscles of mastication, ears, the nervous system, and soft tissues derived from the first and second branchial arches, unilaterally or bilaterally (Ross, 1975; Converse et al., 1979; Kaban et al., 1981; Posnick, 2000). It is the second most common congenital syndrome of the head and neck region after cleft lip and palate, with an incidence as high as 1 in 3500 live births (Munro and Lauritzen, 1985). The hypoplasia can manifest itself in any of the structures derived from the first and second branchial arches, accounting for the wide spectrum of deformities observed in this syndrome. This variable expression has resulted in numerous alternative names, such as Goldenhar syndrome, dysostosis otomandibularis, and oculo-auriculovertebral dysplasia. Gorlin et al. (1990) have suggested that they should all be considered part of the oculo-auriculovertebral group. Over the years, several methods of classification have been developed, describing the anatomical regions and grade of involvement (Posnick, 2000). The most accepted classifications are the orbit, mandible, ear, nerve, and soft tissue (OMENS) classification (Vento et al., 1991) (Box 8.1), and the SAT method, where S stands for skeleton, A for auricle, and T for soft tissue (David et al., 1987).
Box 8.1 OMENS classification of craniofacial anomalies
Orbit
- O0: normal orbital size, position
- O1: abnormal orbital size
- O2: abnormal orbital position
- O3: abnormal orbital size and position
Mandible
- M0: normal mandible
- M1: small mandible and glenoid fossa with short ramus
- M2: ramus short and abnormally shaped
2A: glenoid fossa in anatomical acceptable position
2B: temporomandibular joint (TMJ) inferiorly, medially, anteriorly displaced, with severely hypoplastic condyle
- M3: complete absence of ramus, glenoid fossa, and TMJ
Ear
- E0: normal ear
- E1: minor hypoplasia and cupping with all structures present
- E2: absence of external auditory cannel with variable hypoplasia of the concha
- E3: malposition of the lobule with absent auricle, lobular remnant usually inferior anteriorly displaced
Facial nerve
- N0: no facial nerve involvement
- N1: upper facial nerve involvement (temporal or zygomatic branches)
- N2: lower facial nerve involvement (buccal, mandibular, or cervical)
- N3: all branches affected
Soft tissue
- S0: no soft tissue or muscle deficiency
- S1: minimal tissue or muscle deficiency
- S2: moderate tissue or muscle deficiency
- S3: severe tissue or muscle deficiency
The etiology of this anomaly has been related to defects in neural crest cells (Johnston and Bronsky, 1995), and the most accepted etiopathogenetic mechanism is that of a vascular insult, with hemorrhage and hematoma formation in the developing stapedial artery in the first and second branchial arches, with subsequent maldevelopment (Poswillo, 1975; Soltan and Holmes, 1986). The mandible has long been considered the ‘cornerstone’ of hemifacial microsomia (JC Kaban et al., 1981; Vento et al., 1991), as it is always involved and contributes to the natural course of skeletal asymmetry (Kaban et al., 1981; Kaban et al., 1988; Polley et al., 1997; Kearns et al., 2000). The restricted growth potential of the affected hemimandible inhibits ipsilateral vertical maxillary development, resulting in a progressive facial asymmetry (Figure 8.1). The mandibular hypoplasia may range from mild flattening of the condylar head to complete agenesis of the condyle, ascending ramus, and glenoid fossa. Because of the hypoplastic ramus, the mandibular plane angle is increased, the chin deviates toward the affected side, and there is a corresponding cant of the mandibular occlusal plane, which impacts the maxillary occlusal plane as well as the levels of the pyriform apertures (Figure 8.2).
Figure 8.1 Characteristic facial asymmetry in hemifacial microsomia.

Figure 8.2 Canting of the occlusal plane in a hemifacial microsomia patient.

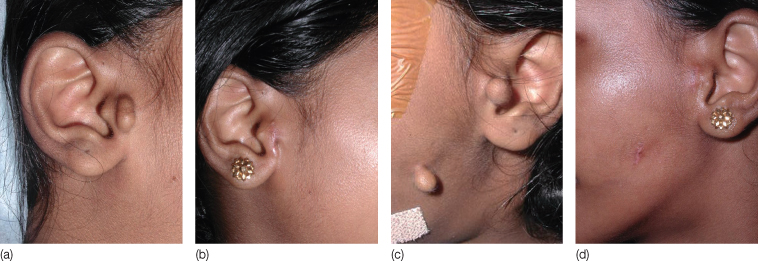
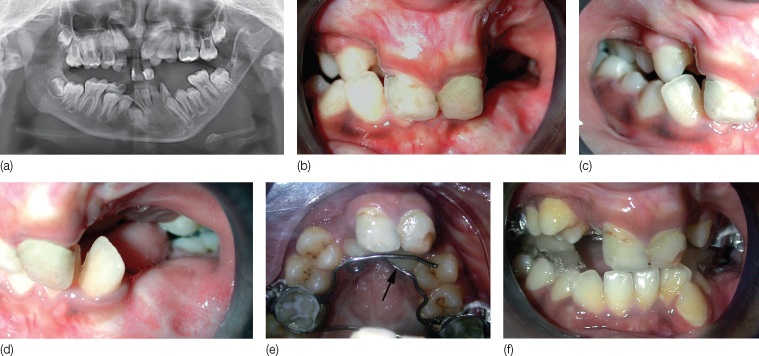
Variable hypoplasia of the ipsilateral zygomatico-orbital region is a common finding, occasionally resulting in orbital dystopia (Gougoutas et al., 2007). Because of their proximity, secondary involvement of skeletal structures not directly derived from first and second branchial arch derivatives, such as the temporal bone, frontal bone, the styloid, mastoid and pterygoid processes, and cervical vertebrae is inevitable (Converse et al., 1973). The auricle is involved in most patients (Meurman, 1957) (Figure 8.3). A combination of cutaneous and subcutaneous connective and neuromuscular tissue deficiency is most evident in the region of the external ear and eye, and the temporal, malar, and masseteric regions of the face, giving rise to a characteristic temporal hollowing and malar flattening (Figure 8.4). This classic appearance may be accentuated by muscular hypoplasia involving the muscles of mastication. Masticatory muscle function on the affected side may likewise be impaired. The maxillary and mandibular dentoalveolar complexes are reduced in the vertical dimension on the affected side, and exhibit crowding, delayed eruption of the deciduous and permanent teeth, and, occasionally, missing molars (Figure 8.5). Macrostomia or clefting through the oral commissure, and hypoplasia of the parotid gland may also be present (Whitaker and Bartlett, 1990) (Figure 8.6). Facial palsies have been estimated to occur in 22–45% of patients (Figure 8.7) (Bergstrom and Baker, 1981; McCarthy, 1997).
Figure 8.3 Malformation of external ear (microtia), as part of hemifacial microsomia.

Figure 8.4 Characteristic malar flattening in hemifacial microsomia.

Figure 8.5 (a,b) Occlusion in two craniofacial microsomia patients.
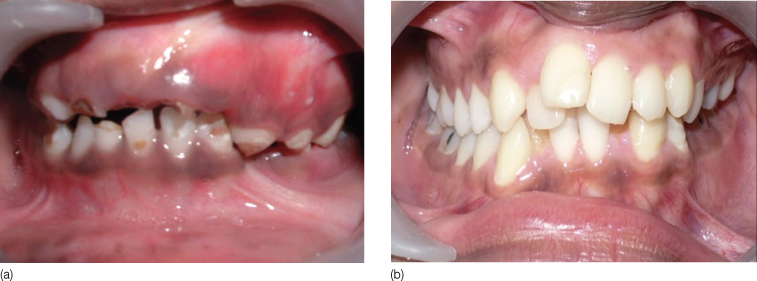
Figure 8.6 Macrostomia and ear anomaly in a baby with craniofacial microsomia.

Figure 8.7 This patient had facial palsy as part of hemifacial microsomia syndrome. (a) Frontal view. (b) Frontal view showing incomplete eye closure and deviation of the angle of the mouth towards the normal left side. (c) Worm’s eye view showing malar flattening and deviation of the angle of the mouth.

Management
Management of hemifacial microsomia requires a comprehensive evaluation of the extent of the skeletal contribution to the deformity. It is possible that functional appliance treatment and dental compensation may suffice for minor skeletal discrepancies, but moderate to severe skeletal problems will require surgical intervention. The timing of and techniques used for correction will differ from center to center, and from patient to patient. The parents are often in a state of shock, and should be met and counseled by the members of the team during the first visit itself (Barden et al., 1989). Treatment will depend on the severity of the dysmorphism and age of the child (Silvestri et al., 1996).
No surgery is indicated in very young children, unless there is an airway disruption due to mandibular micrognathia, which is usually dealt with by tracheostomy or mandibular distraction (McCarthy et al., 1992, Boston and Rutter, 2003). But often, excision of the preauricular skin tags and cartilage remnants and correction of macrostomia are carried out as this is quite reassuring for the parents because it removes some of the stigmata of the syndrome (McCarthy, 2007) (Figure 8.8). Assessment of hearing and provision of hearing aids also need attention during the early childhood.
Figure 8.8 Ear tag excision as part of initial soft tissue corrections in hemifacial microsomia: (a,c) preoperative and (b,d) postoperative photographs.
The most widely followed treatment protocol is that of Silvestri et al. (1996), based on the SAT classification system (David et al., 1987). It emphasizes functional appliance treatment during growth, followed by surgery to reposition the skeleton, and grafting. The objectives of early intervention include providing a growth stimulus for the affected side of the maxilla, and the associated dentoalveolar and soft tissues. Effective mandibular lengthening and correction of facial asymmetry has been reported with distraction osteogenesis, and this has become the treatment of choice, especially in growing children (McCarthy et al., 1992; Cascone et al., 2005). The distraction is beneficial, especially in patients with psychological or functional impairments, as it improves function and appearance during growth, creating an almost normal interim status. Generally, distraction osteogenesis of the mandible is too complicated to perform in children under 2 years of age, because of inaccuracies in the assessment of the location of the tooth germs.
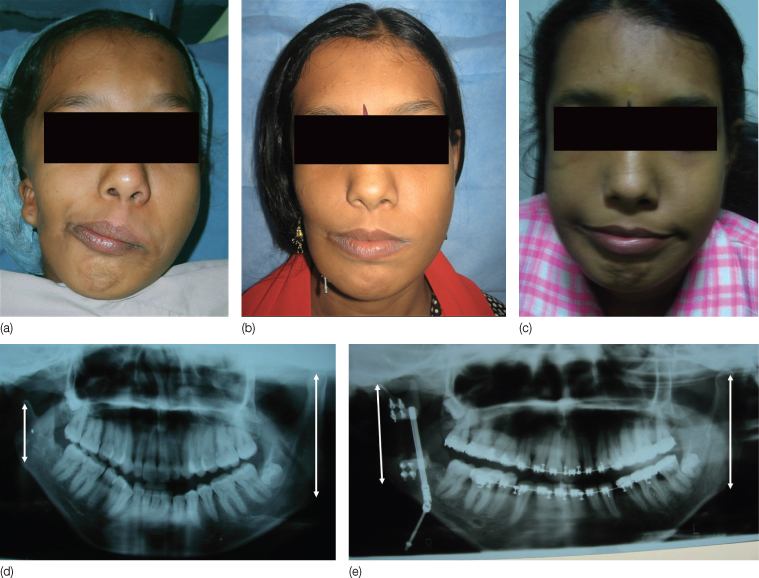
In preadolescent patients, distraction may be performed to open up space vertically and anteroposteriorly for development of the soft tissues, and subsequent secondary maxillary growth. The soft regenerate requires protection from the constricting effects of the healing tissues, so the orthodontist will be required to construct a unilateral bite block to maintain the open bite that is created. This bite block may be modified to encourage dental eruption following consolidation of the regenerate. In postadolescent patients, distraction procedures are reserved for the more severe skeletal anomalies, and it is not uncommon for the patient to undergo mandibular distraction as the major defect usually lies in the mandible, followed by maxillary surgery and revision surgery on the mandible, to achieve the final position of the mandible. The maxilla and mandible may be simultaneously distracted to effect three-dimensional changes, if required (Ortiz-Monasterio et al., 1997). There are conflicting reports regarding the growth potential of the mandible after initial distraction (Figure 8.9). Though Sheyte et al. (2006) have reported mandibular growth after distraction, usually further surgical management is needed after growth is complete, as the inherent growth potential of the affected side is deficient (Iseri et al., 2008; Nagy et al., 2009). The patient will also require a series of soft tissue procedures to compensate for the hypoplasia and ear malformations (Brent, 1992; Longaker and Siebert, 1995; Wang and Andres, 1999) (Figure 8.10).
Figure 8.9 Mandibular distraction in a craniofacial microsomia patient. (a) Pre-distraction occlusion; (b) distractor in place; and (c) post-distraction occlusion.
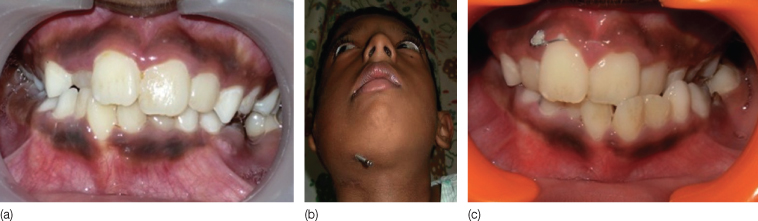
Figure 8.10 Pre- and post-distraction phases in the management of a craniofacial microsomia patient. (a) Pre-treatment extraoral view. (b) Post-distraction extraoral view. (c) Soft tissue corrections performed using a temporoparietal flap. (d) Pretreatment orthopantomogram – note the discrepancy between the right and left mandibular rami in the vertical plane (arrows). (e) Post-distraction orthopantomogram showing nearly symmetrical rami after distraction (arrows).
Orthodontic Treatment in Craniofacial Microsomia
Orthodontic treatment is carried out in a staged manner. The best possible results are achieved when the orthodontist and the surgeon agree on a carefully designed and customized treatment plan. Both should be aware of the treatment objectives, limitations, and risks. This approach should also be explained to the patient and the family.
The orthodontic treatment phases can be broadly divided into pre-distraction orthodontic treatment, orthodontic treatment during distraction and consolidation, and post-consolidation orthodontics.
Pre-Distraction Treatment Planning and Orthodontics
This phase of treatment is carried out in the growing child, where the aim of distraction is to decrease the facial asymmetry. Vector planning is crucial in this stage, depending on the lengthening of the mandible required in the vertical, sagittal, and oblique planes. The decision about the type of movement that would be required, and the associated position of the distractor, is made in a combined clinic between the operating surgeon and orthodontist (Hanson and Melugin, 1999). It is always advantageous to use stabilization appliances as part of pre-distraction, which help in elastic traction (Hanson and Melugin, 1999). This treatment also facilitates control of the force vectors and maintenance of the transverse relationship between the maxilla and mandible, preventing lateral displacement of the dental segment.
Orthodontics During Distraction
The aim of orthodontic treatment during the distraction is to control the force vector to direct the growth of the mandible into an advantageous position. As the distraction progresses, the rami lengthen vertically, resulting in a posterior open bite. In this stage, the mandibular occlusal cant is corrected, and vertical symmetry is established. But as the posterior open bite increases, the patient might find it difficult to occlude and so shifts the mandible to the unaffected side. This situation can be observed clinically as shifting of the dental midline away from the distracted side, and as a buccal crossbite on the distracted side. A crossbite develops on the unaffected side, and is termed laterognathism.
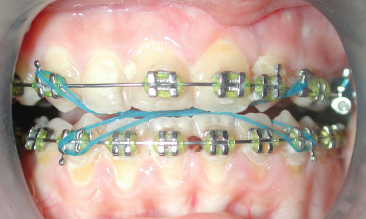
Orthopedic forces are required to correct the laterognathism. The direction of force from the elastics may be opposite to that of the distraction forces, and so the distraction force has to be greater than the elastic traction. Elastic traction can also be used to coordinate the dental arches, and correct the dental midline shifts (Figure 8.11). Orthodontists should maintain all records for future re-evaluations and planning treatment progression.
Figure 8.11 Midline oblique elastics to coordinate dental arches during distraction osteogenesis.
Post-Distraction Orthodontics
In the growing child, post-distraction orthodontic treatment is extremely important. Guided eruption of the teeth, correction of laterognathism with elastics, and controlled vertical closure of the unilateral posterior open bite are the main objectives of this stage of treatment, along with stabilization of the corrected mandibular occlusal plane. Failure to stabilize the occlusal plane will lead to overeruption of both maxillary and mandibular teeth, and re-establishment of the previous maxillary and mandibular occlusal cant. The corrected mandibular occlusal plane is maintained by the selective eruption of the maxillary teeth, and can be performed with:
- An occlusal acrylic wafer that is reduced one tooth at a time, to allow controlled eruption of the maxillary teeth. Santiago and Grayson (2009) recommend inserting a bite block that fills the open bite on the distracted side soon after active distraction, providing a bilateral balanced occlusion (Figure 8.12).
- A functional appliance with lingual shields, to provide lateral control of mandibular position. A bite plane is also included, which is adjusted to allow serial eruption of maxillary teeth. Elastic traction is often added to the appliance, which has been shown to decrease treatment time (Hanson and Melugin, 1999).
Figure 8.12 Sequential steps in orthodontic treatment following distraction osteogenesis in a growing child with hemifacial microsomia and bilateral cleft palate. (a) Pre-treatment orthopantomogram. (b–d) Occlusion after distraction. Note the bilateral posterior crossbite. (e) Fabrication and placement of a soldered custom-made expansion appliance to procline the central incisors. The right maxillary canine can be seen erupting behind the central incisor (arrow). (f) Bite block in the mandibular arch for promoting controlled eruption of maxillary teeth.
The Role of Functional Appliances
The aim of functional therapy is to stimulate impaired function of the stomatognathic system, to substitute for absent structures, and stimulate differential growth on the two sides of the face (Silvestri et al., 1996). Functional appliances alone are more effective in patients with the milder form of the malformation than in those with severe malformation, where the functional appliances have to be combined with further orthodontics and surgery. But even in these cases, several authors believe that functional therapy i/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


