8 Lasers in Fixed Prosthetic and Cosmetic Reconstruction
Laser Wavelengths for Cosmetic/Prosthetic Procedures
Carbon Dioxide Lasers
Oral soft tissue is 90% to 97% water. The CO2 wavelength is highly absorbed by water, more so than any other soft tissue laser wavelength. CO2 lasers are therefore the most efficient lasers because they are best absorbed by soft tissue. Soft tissue excision or incision surgery is accomplished at 100° C, at which vaporization of intracellular and extracellular water causes ablation of biological tissue.1
Erbium Lasers
The erbium-doped yttrium-aluminum-garnet (Er:YAG) wavelength is 2940 nm and the erbium, chromium–doped yttrium-scandium-gallium-garnet (Er,Cr:YSGG) 2780 nm. Erbium laser wavelengths are transmitted through semiflexible hollow waveguides, low-OH− fiberoptic cables, or articulated arms. All the delivery methods terminate in a handpiece that may use sapphire or quartz tips to transmit the energy to the target tissue. These wavelengths are highly absorbed by the OH− radical and thus work well in hard tissue, targeting the OH− in hydroxyapatite. The erbium lasers can also cut soft tissue, but with much less hemostatic ability than soft tissue lasers.2
Erbium lasers are safe when ablating tooth decay and working close to the pulp. Because this laser wavelength penetration is not significant in depth, patients may not need anesthesia. Erbium laser cavity preparation is less traumatic to the tooth’s pulpal tissues than techniques that involve rotary bur drilling. The vibration and heat produced by rotary instruments, which are the main reasons for discomfort during procedures, do not occur with the erbium wavelengths.3
One disadvantage compared with conventional techniques is diminished bond strength, particularly tensile strength, when etching with erbium lasers.4 Another disadvantage is that erbium wavelengths cannot remove gold or metal crowns, vitreous porcelain, or amalgam restorations (see Chapter 11).
Diode Lasers
Diode lasers deliver wavelengths at 810 to 1064 nm. Diode lasers are compact and portable solid-state units. They are used strictly for soft tissue procedures and penetrate 2 to 3 mm or more into soft tissue, depending on the wavelength and tissue biotype. Diode lasers are absorbed by pigmented structures, making them ideal for cutting melanotic soft tissues and providing hemostasis.5
The usefulness of the diode laser can be greatly expanded by proper carbonization of the fiber tip. This allows for vaporization with limited peripheral damage to nonpigmented tissue.6
Neodymium:Yag Laser
The Nd:YAG wavelength of 1064 nm delivered in a free-running mode can be used for numerous soft tissue procedures. Similar to the diode and CO2 lasers, the advantages of the Nd:YAG laser are a relatively bloodless surgical field, minimal swelling, reduced surgical time, excellent coagulation, and in most cases, reduced or no postoperative pain.7
The main disadvantage of the Nd:YAG laser is the depth of penetration into the target tissue. The Nd:YAG wavelength penetrates deeply into tissue because it is poorly absorbed by water, the main component of gingival tissue. The clinician must be alert to the risk of unnecessary collateral tissue damage, particularly to the underlying bone or pulpal tissues. Tissue vaporization is slower than with other, better-absorbed laser wavelengths (e.g., CO2). Applications of a topical photo-absorbing dye can shorten the lag time for absorption of the laser energy.8 Nd:YAG laser light directed at the clinical crown or root surface of the tooth is a concern. Heating of the pulp may be of sufficient magnitude to cause pulpal inflammation and possibly irreversible damage to pulpal tissue.9 This would occur only if incorrect laser parameters were used. This highlights the critical role of proper laser training when performing laser-enhanced prosthetic and cosmetic dentistry (see Chapter 16).
Biologic Width
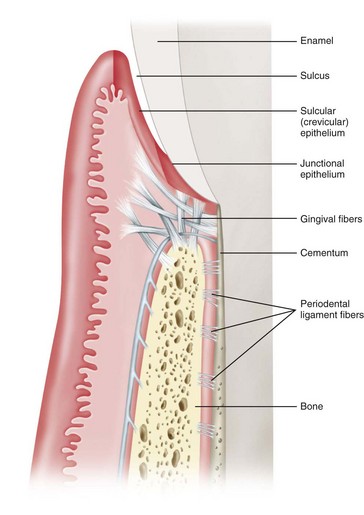
Biologic width is defined as the combined height of connective tissue and epithelium that isolates the bone from the oral cavity. It is the distance from the most apical extent of a dental restoration to the osseous crest necessary to maintain periodontal health10 (Figure 8-1).
The biologic width distance is approximately 2 mm, with about 1 mm of the 2 mm composed of the connective tissue attachment and 1 mm consisting of the junctional epithelium. Because it is impossible to restore a tooth perfectly to the precise coronal edge of the junctional epithelium, the 1 mm of depth of the sulcus can be added to the biologic width to establish a margin of safety.10
This distance is important to consider when fabricating dental restorations, because the dentist must respect the natural architecture of the gingival attachment to avoid complications. The problem is not the restoration but rather bacteria, which will always find shelter in the interface between the restorative margin and the tooth structure. When restorative procedures do not take these considerations into account and violate biologic width parameters, the following three possible issues may arise10 (Figure 8-2):
 Gingival recession and localized bone loss occur, most dramatically in cases with thin labiobuccal bone.
Gingival recession and localized bone loss occur, most dramatically in cases with thin labiobuccal bone.Soft Tissue Troughing With and Without Gingivoplasty
The gingival trough is defined as the narrow space between the free margin of the gingival epithelium and the adjacent enamel of a tooth.11 At times, permanent alteration of the gingival contours around a tooth or teeth is necessary to ensure a superior, long-lasting cosmetic restoration. The outcome of a direct or indirect restoration is related to the dentist’s ability to control the surgical site. In controlling the site for delivery of a superior restoration, lasers provide the following functions:
These steps are essential for the fabrication of precise impressions, for digital scanning, or for direct placement of restorative materials. The displacement of gingival tissue is critical for finalizing tooth preparation and impression taking or restorative material placement.12 A common challenge to the dentist is placement of the preparation “finish line” at or below the crest of the gingiva so that the margin does not show. Retraction of the gingival tissues can be performed mechanically with the retraction cord impregnated with medicaments for hemostasis. Packing of retraction cord around the circumference of the tooth to reflect the gingiva away from the tooth and to absorb crevicular fluids is the conventional technique used to record the finished preparation margin or to complete placement of the direct restorative material.
Conventional Techniques
A technique widely used for gingival retraction is a double-cord technique for subgingival reflection of tissue. Removing the second (top) retraction cord before injecting the impression material or creating an optical impression allows for complete capture of the finish line. This time-consuming technique has its disadvantages, including potential injury to the periodontal ligament if excessive force is used; difficulty in removing the retraction cord without creating bleeding, and postoperative discomfort.13
Another conventional gingival troughing technique, electrosurgery or radiosurgery, allows for contouring of gingival tissues and hemorrhage control. Healing after electrosurgery can produce a delayed wound-healing response, asymmetrical gingival heights, crestal bony recession, and moderate postoperative discomfort.14 In a study of electrosurgical gingival troughing with a fully rectified current on rhesus monkeys, Wilhelmsen et al.15 showed statistically significant recession of the gingival margin along with apical migration of the junctional epithelium. Deep soft tissue resections close to bone repeatedly produced gingival recession, bone sequestration and necrosis, loss of bone height, furcation involvement, and tooth mobility. Electrosurgery (or radiotherapy) is contraindicated around dental implants16 and must not be used in patients with pacemakers, with previous radiation to the jaws, with poorly controlled (or uncontrolled) diabetes, or with blood dyscrasias, immunodeficiencies, or other diseases that cause delayed or poor healing.10
Scalpel techniques are primarily used to resect tissue to provide access and visualization of the target site. Scalpel incision surgery may result in gingival attachment loss with apical repositioning, exposure of sensitive root surface to the oral environment, asymmetrical gingival margins, and the postoperative pain and discomfort typically associated with periodontal surgery.17
Laser Troughing
In contrast to conventional techniques, laser troughing allows for clear, clean visualization of gingival margins. Most lasers are excellent coagulation devices, with minimal to no bleeding. Unlike blade or electrosurgical techniques, laser gingival troughing with a laser gingivectomy can be performed at the same appointment as impression taking. The patient saves a trip to the office, greatly reducing valuable chair time. The ease with which necrotic tissue debris is removed from around the preparation finish line simplifies impression taking. Retraction cord is not necessary for reflection around the tooth or teeth; no placement or removal of cord from multiple pockets is required when taking impressions of multiple teeth or a full arch. Laser treatment causes no recession or repositioning of the gingival margin.18 Laser troughing promotes an ideal environment for current impression scanning devices.
Dentists who practice laser surgery and laser gingival troughing have reported high patient acceptance and comfort. Neill’s survey19 on patient comfort after laser gingival troughing revealed that 3 hours after treatment, patients were comfortable, with half “extremely” comfortable. The overall pain rating was 1.9 (scale of 0.0-10.0), indicating patients experienced minimal to no pain.
Laser vaporization of fibrotic tissue around crown margins is extremely fast, with virtually no bleeding, swelling, or postoperative pain. There is predictable stability of the gingival tissue on healing, with the additional benefit of elimination of pathogens from the periodontal pocket.20,21
Procedure
To maximize its efficiency, the tip must be kept free of debris. With CO2 lasers, a stream of air blown through the tip keeps the hollow tip patent. Debris may accumulate on the outside of the tip, however, in which case the tip should be wiped down with dry gauze or replaced. Nd:YAG and diode lasers use glass/quartz fibers, which become dulled and scratched after multiple uses. A dull tip may cut tissue poorly, like cutting tissue with a broken piece of glass, leaving tissue tags.7 The tip must therefore be cleaved periodically to ensure optimal results. Some diode lasers are supplied with multiuse disposable tips, but the cost of tips is much greater than simply using a standard 3-meter optical fiber. The tip must also be “activated” so that the depth of penetration of the wavelength is minimized, with no deep thermal damage.
During troughing to establish gingival proportions with the diode and Nd:YAG lasers, the clinician may note carbonization on the tissues.8,22 This can be quickly removed with a 3% hydrogen peroxide diffusing-brush syringe (Figures 8-3 and 8-4).
Crown-Lengthening Procedures
Crown-lengthening procedures have progressively become more driven by esthetics because of the increasing popularity of “smile enhancement” procedures. Crown lengthening is a surgical procedure performed to expose a greater gingivoincisal length of tooth structure, usually to restore the tooth prosthetically. This involves excising a small amount of gingival tissue around the tooth and predictably removing a given height of only gingival tissue (soft tissue crown lengthening) or both gingival tissue and alveolar bone (osseous crown lengthening). Although many general dentists perform this procedure, many others refer crown lengthening to a periodontist or oral surgeon. Conventional techniques of osseous crown lengthening generally involve a full-thickness flap procedure to establish the new gingival level.10
Soft Tissue
The crown-lengthening procedure is basically an excision of gingival soft tissue. Conventional methods of executing this technique involve surgical scalpels, periodontal knives, or electrosurgery. Recommended placement of the excision is at least 2 mm coronal to the bottom of the gingival attachment, to reduce the risk of root exposure and violation of biologic width rules.23
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses