IMPLANTOLOGY
Riccardo Benzi, Giuseppe Giulio Gullo Vivaldi
INTRODUCTION
In the last ten years, dental practice has had an important evolution in new high quality dental ma-terials, giving to the patients the possibility of different choices of dental treatments, with best functional and aesthetic results in oral rehabilitation if compared with the past. In fact, during the 50’s and 60’s, modern implantology, going through a “pioneer” phase with professor Branemark’s studies, has been scientifically structured and it is actually one of the most important procedure in surgical techniques and prosthetic rehabilitative possibilities in dentistry. Today, we should confront ourselves with a reality in which the implant therapy, correctly executed and according to the surgical protocols, validated by the prosthetic point of view, is absolutely in many circumstances the most “conservative” therapy, allowing us, whenever possible, an extremely “focal” approach in the rehabilitation of the most disparate types of edentulia. Surgical techniques always less invasive and protocols more and more strict in the rehabilitation times have found their presuppositions in implant surfaces and in quicker and quicker osteointegra-tion times, thanks to technological supports for the execution of “Guided Surgery”. The possibilities of a computerized Implant-Prosthetic solution (CADD – Computer Aided Dental Design) have supported some instruments for the execution of surgeries with a “blind guide” in the flapless technique with an exceptional possibility of post-surgical complications for the patients. In the beginning, the costs of this new technique were very high and few people could accept this type of treatment. Nowadays, the developing of new materials and the diffusion of this technology have allowed a large consensus of this implanto-prosthetic approach with a good relationship between costs/benefits. The consequence of this diffusion is that, for example, in Italy, more than 1.000.000 of implants are annually inserted, according to the data in 2006. Only 60% of these implants is represented by brand products, supported by studies and research, while the other 40% have no clinical trials and basic research. For this reason, it is very important not only the surgical technique, but also the correct choice of the implant materials. Implantology has a central role for the therapeutical choices in Oral Rehabilitation: consequently, research orientation and development of the manufacturers in this sector are in continuous, rapid and constant evolution of the devices, the prosthetic components and all the products correlated with the adoption and/or the individuation of particular applications of other technologies to the implant therapies. One of these technologies are represented by Laser application.
LASER AND IMPLANTS
In the constant research of operative strategies of cooperation for the execution of therapies with a high technical, biological and economical contents, it has become logical to researchers and makers of medical lasers, to test and finalize protocols in order to obtain the best characteristics of most laser sources to use in the management of the daily clinical implantology. But, in this wide panorama of laser sources, The question is: “which is best laser for the operative needs in implantology? And what can we better do with the others and what can we not do?” (Table 8.1)
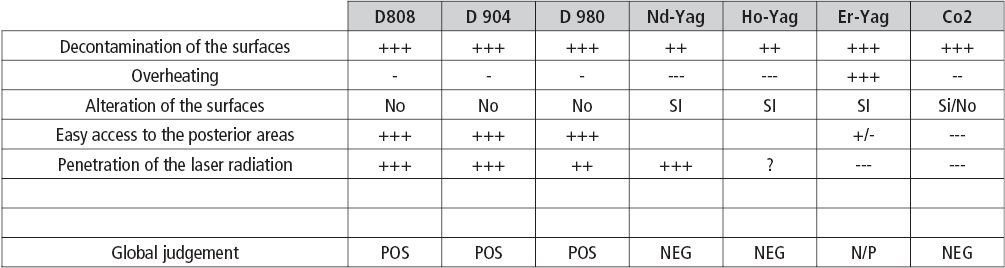
Table 8.1
Before evaluating all this we have to define what are ours expectations of reference regarding the characteristics that a laser must have or must not have to be utilizable in implantology, and thus we will say:
It should have the minimal possible risk to damage the soft tissues as well as the hard tissues because of the overheating and the lateral diffusion of the heat. In fact, different wavelengths could be applied on soft tissues, according to the laser-tissue interaction, using correct parameters and protocols. Erbium laser family is the only laser capable to interact securely on hard dental tissues.
It should not be able to modify the implant surface especially with the modern bioactive surfaces in that it would jeopardize irreparably the characteristics and therefore the disposition for osseointegration.
It should have the best characteristics of decontamination of the implant surfaces by the useful power density as low as possible, remembering that power output inferior to 2.5W are not resolutive over the spores; This concept is at the base of decontamination techniques for implant surfaces and for a higher predictable and efficient management in the peri-implantitis cases. (Figg. 8.1-8.15)
Case 1: Peri-Implantitis (Fig. 8.1-8.15)
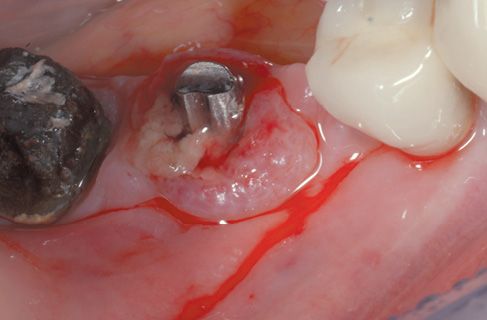
Figure 8.1 • Pre-operatory view of the surgical site.

Figure 8.2 • Pre-operatory x-ray.
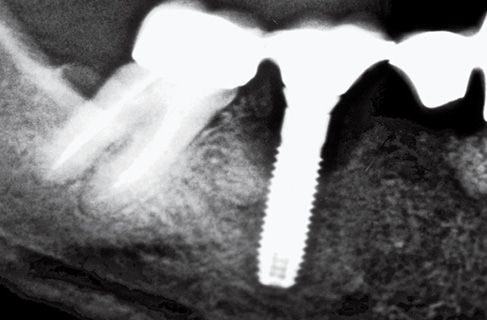
Figure 8.3 • Pre-operatory x-ray.
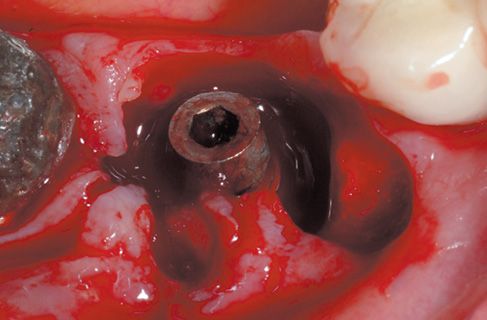
Figure 8.4 • View of perimplantary granulation tissue.
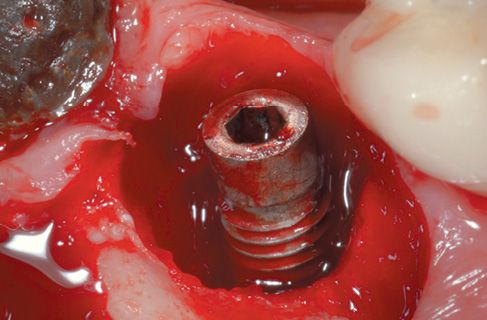
Figure 8.5 • View of the surgical site after diode laser decontamination.
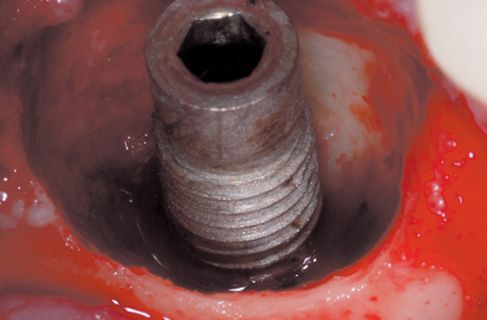
Figure 8.6 • View of the surgical site with granulation tissue perfectly removed.
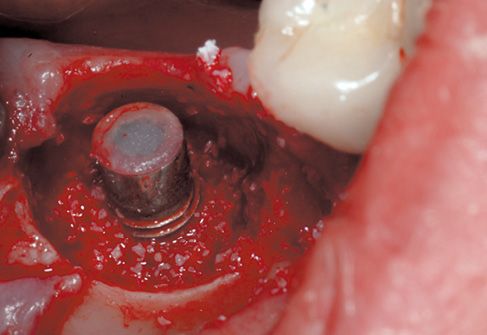
Figure 8.7 • Filling with biomaterial, first step.

Figure 8.8 • View of the surgical site, filling with biomaterial is completed.
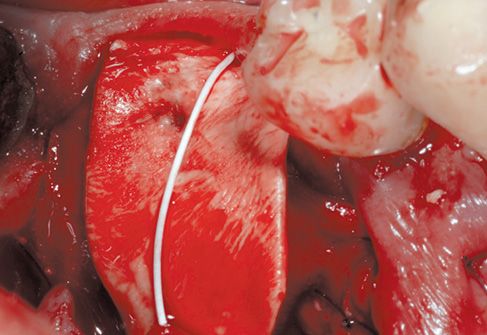
Figure 8.9 • The surgical site is protected with a connective membrane.
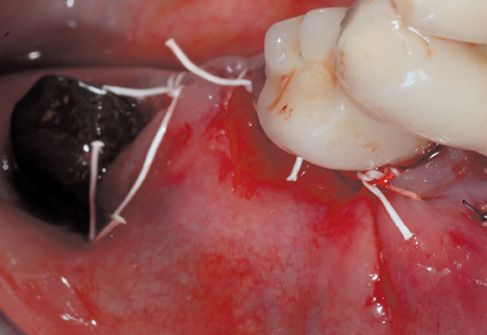
Figure 8.10 • After suitable tissue release, continuous suture with single points results perfectly sealed.

Figure 8.11 • Final x-ray, post-surgery.
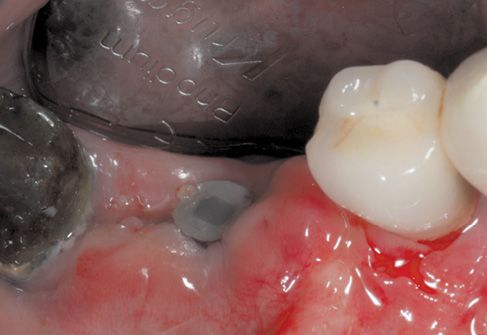
Figure 8.12 • Healing at 1 month.
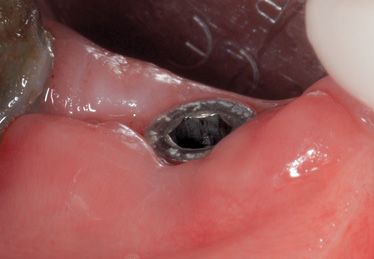
Figure 8.13 • Healing at 3 months.

Figure 8.14 • Control at 5 months.
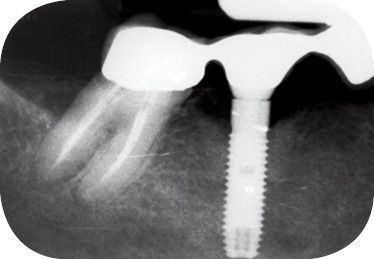
Figure 8.15 • Control at 1 year.
It should be provided Preset (better if it could be brought up to date periodically with Updates of the producing house) that allows the operator to utilize always the protocols and the settings of the instrument that are more efficacious for the therapy in act.
It should have a great manageability and practical use: this will make us prefer the Laser with light transmission by optical fibers, for an easy access to the posterior areas in oral cavity than those with articulated arms and mirrors system.
THERAPEUTICAL INDICATIONS
In this section, we should consider how the Laser technology, if well managed with the correct parameters, could more and more simplify and make most of the procedures linked to the implant therapy in its different phases. Particularly, the medical Lasers could be of great efficacy in the various phases of the implant therapy: we will consider thus a typical therapy in all its phases and we will analyze the possible ideal applications of the Laser. (Table 8.2).
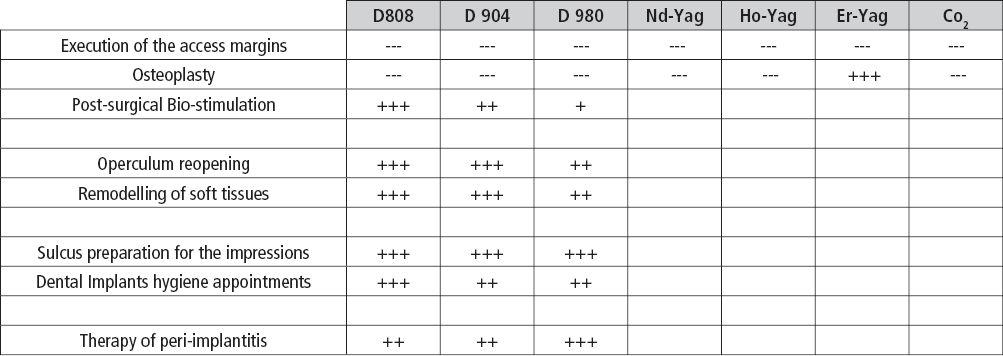
Table 8.2
PHASE I Surgical
Execution of the access margins: the surgical execution of the access margin should be always performed by a cold knife or with a non-laser technique. In fact the intrinsic characteristics of the laser in cutting soft tissue, produce haemostatic intravascular coagulation and a layer, even if minimal, of protein denaturation will m/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


