8
Endodontic Aspects of Root Resorption
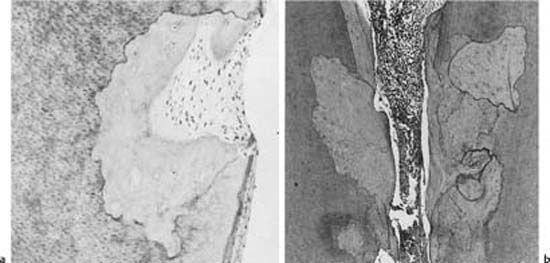
The mineralized tissues of the permanent teeth are not normally resorbed. They are protected in the root canal by the predentin and the odontoblasts and on the root surface by the precementum and the cementoblasts. If the predentin or the precementum becomes mineralized or, in the case of precementum, is mechanically damaged or scraped off, osteoclast-like cells will colonize the mineralized or denuded surfaces and resorption will ensue. However, resorbing cells require continuous stimulation during phagocytosis, and stimulation by a denuded dentin or cementum surface is not sufficient to sustain the resorptive process for long. A phagocytic colonization of denuded areas of the root, therefore, will be transient without additional stimulation of the cells, and repair with formation of a cementum-like tissue will occur both in the root canal and on the root surface (Fig. 8.1). This type of resorption is referred to as transient root resorption.
Transient root resorption occurs quite frequently in traumatized teeth and in teeth which have undergone orthodontic and periodontal treatment, but is also seen in other teeth apparently as a result of wear and tear. Transient root resorption is without clinical importance and the resorption defects are usually too small to be detected, even radiographically.
Root resorption which is initiated by a denuded area of the root surface may be sustained by mechanical irritation, increased pressure in the tissue, or infection of the root canal and tubules of the crown and root dentin.
Mechanical stimulation of osteoclasts to sustain a progressive resorption is seen, for example, in root-fractured teeth where the sharp edges of the root fragments are selectively resorbed. Only when the fragments are well rounded and cause no further tissue irritation will the resorption stop (Fig. 8.2).
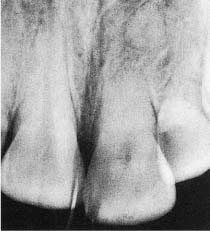
Pressure resorption in the permanent dentition may be seen during tooth eruption, especially of maxillary canines and mandibular third molars, and in patients with certain tumors impinging on the roots of the teeth. Pressure resorption is also commonly seen during orthodontic movement of teeth, usually in the form of apical resorption and a shortening of the roots (Fig. 8.3). Pressure resorption may be quite destructive if diagnosed late on. However, the resorptive process will be arrested when the stimulation of the resorbing cells stops.
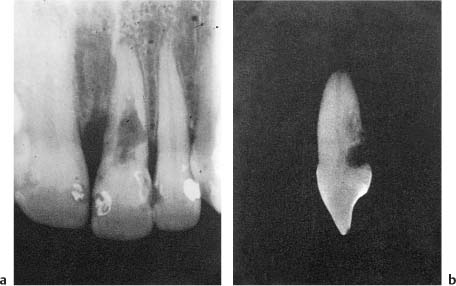
Fig. 8.1 Transient root resorption (a) on the root surface and (b) in the root canal. A cementum-like tissue is laid down in the resorption lacunae at both locations.
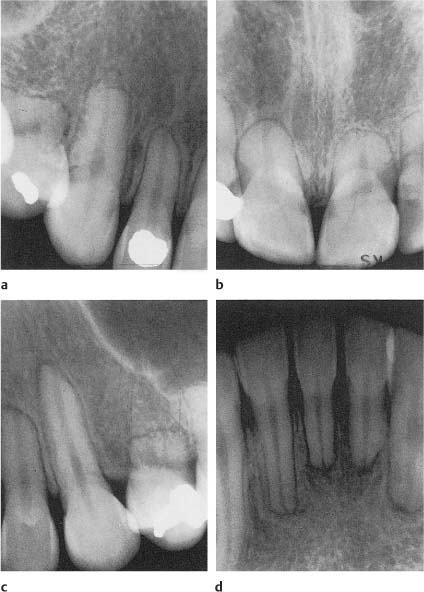
Root resorption sustained by infection is by far the most important clinical condition from an endodontic point of view. It can occur in the root canal (called internal resorption; Fig. 8.4), or on the root surface (referred to as cervical resorption; Fig. 8.5 or external inflammatory resorption; Fig. 8.6), depending on whether the microbial stimuli come from the gingival sulcus or from the root canal. An infectious inflammation is accompanied by the production and release of cytokines such as interleukin-1, tumor necrosis factor, and lymphotoxin, which are mediators of hard-tissue resorption. In addition, prostaglandin E2, bacterial products, and components such as endotoxins will be present. A resorptive process sustained by infection can therefore progress quite rapidly, and in a short time may lead to complete destruction of the root (Fig. 8.6).
Fig. 8.2 Radiograph of a maxillary left central incisor 24 years following a traumatic injury resulting in a fracture of the root of the tooth. Note selective resorption of the sharp edges of both root fragments and repair.
Fig. 8.3a–d Radiographs of maxillary and mandibular teeth with apical root resorption following orthodontic tooth movement. The root resorption in this case is severe and the etiology may not be fully understood.
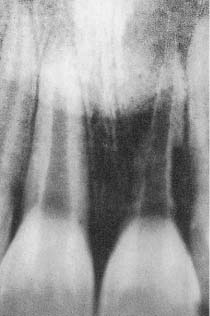
Fig. 8.4 Radiograph of a maxillary central incisor with a midroot radiolucent area indicating internal root resorption.
Fig. 8.5 Radiograph of an endodontically treated maxillary incisor with a cervical radiolucent lesion in the tooth and adjacent bone (arrow) indicating cervical root resorption. Note the difference in the location of the resorption cavity and the proximal restorations of carious lesions.
Fig. 8.6 Radiograph of a maxillary left central incisor with external inflammatory resorption. Four months following a luxation injury, most of the root is resorbed. Note that the outline of the entire root canal can be recognized.
Replacement or endosteal root resorption is seen in teeth which have suffered dentoalveolar ankylosis because of necrosis of the periodontal ligament. With time, the roots of these teeth will be replaced by bone (Fig. 8.7).
Fig. 8.7 Radiograph of a maxillary left central incisor with replacement resorption. The tooth is ankylosed and in infraocclusion, and the root has been replaced by bone. Note that endodontic treatment has had no effect on this type of resorption.
Internal Root Resorption
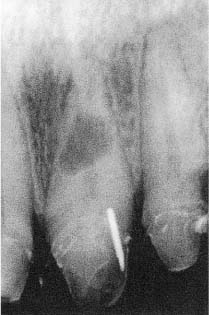
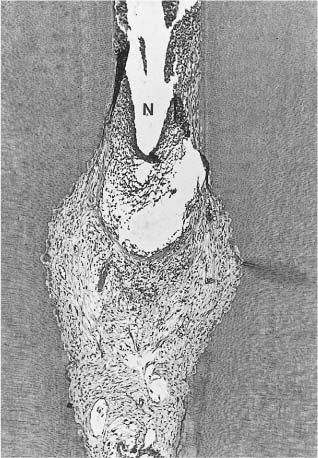
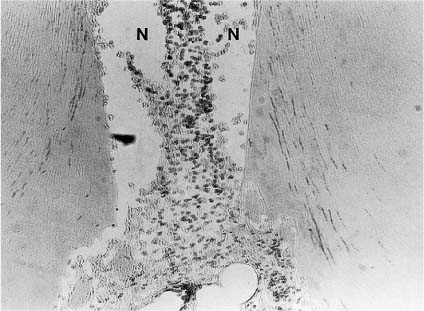
Traditionally, internal resorption has been associated with a long-standing, chronic inflammation in the pulp (Fig. 8.8). This may hold true in the sense that the transient type of internal resorption discussed above may occur if the odontoblasts in an area of the root canal are destroyed so that the predentin becomes mineralized. However, in teeth with progressive internal resorption where the resorption lacunae are large enough to be diagnosed radiographically, the resorptive activity is sustained by infection of necrotic tissue coronally in the root canal. Bacterial products may then reach areas of the canal with vital pulp tissue through the dentinal tubules (Fig. 8.9). Thus, in order for progressive internal resorption to occur, the dentinal tubules have to have a special and fortuitous course. They have to be open to an area of the root canal where the tissue is necrotic and infected so that microorganisms may enter the tubules, and then lead to an area of the canal with vital pulp tissue. This is a rather unlikely occurrence and probably explains why progressive internal resorption is a rarity in permanent teeth.
An internal resorption lacuna when seen radio-graphically is a definite sign that endodontic treatment is indicated. Clinically in such teeth, one will find pulp necrosis in the pulp chamber and usually in the root canal to a level somewhere coronally to the resorption lacuna. The resorptive area and the root canal apical to this area will contain vital tissue. In some instances, the entire pulp will be necrotic. The resorptive process will then have stopped since obviously vital cells are needed for the resorption to continue. In root canals with vital tissue it may prove difficult to remove the tissue in the resorption lacuna since this cannot be reached by instruments. Irrigation with copious amounts of 5% sodium hypochlorite may have some effect, but the treatment of choice is to pack the canal and the resorption lacuna with calcium hydroxide paste. By the next visit, the calcium hydroxide will have necrotized any remaining tissue in the lacuna, and the necrotic remnants are readily removed by irrigation with sodium hypochlorite.
Fig. 8.8 Interface between necrotic (N) and vital inflamed tissue in a root canal. Resorption of the root canal walls (internal resorption) near the inflamed area of the pulp can be seen (hematoxylin-eosin).
Fig. 8.9 Interface between necrotic (N) and vital tissue with an internal resorption lacuna in a root canal. Bacteria are present in the dentinal tubules leading from the area of the root canal with necrotic (infected) tissue to an area with vital tissue and internal resorption (Brown–Brenn stain).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses