Chapter 8
Case studies in ultrasonic debridement
CHAPTER OBJECTIVE
- Through the presentation of clinical cases, this chapter integrates the content addressed in preceding chapters and demonstrates the application of evidence-based theory to case-based decision making in the clinical practice of periodontics.
CASE A: INITIAL AND SUPPORTIVE PERIODONTAL THERAPY
Presentation
This 53-year-old Caucasian male presented to a general dental practice for a dental examination and subsequent care after not receiving any dental care since at least seven years prior, due to financial constraints. The patient suggested that his spouse compelled him to make an appointment as she was concerned with the appearance of his teeth.
Medical history
- The patient’s height and weight are 5′ 7″ (1.70 m) and 190 lbs (86.2 kg). Body mass index (BMI) = 29.8.
- The patient has smoked cigarettes since the age of 17, and is currently smoking an average of a half a pack (10 cigarettes) per day.
- Three years ago, the patient was diagnosed with high blood pressure and was prescribed valsartan, an angiotensin receptor blocker, 160 mg/daily.
- The patient’s blood pressure control has improved and is now averaging 133/80 mm Hg. He reportedly is reevaluated by his physician every three months.
Clinical examination
- Moderate–heavy supragingival and subgingival calcified deposits at multiple sites.
- Soft tissue changes (contour and color changes) consistent with inflammation were noted at multiple sites, especially at posterior lingual and palatal sextants.
- Generalized bleeding upon probing was noted.
- Carious enamel and root surfaces were noted at multiple teeth.
- Exposed root surface structure was noted at multiple teeth.
- Broken restoration noted at tooth #30 (FDI 46).
- Malocclusion of left posterior with crowding and challenging oral hygiene access.

Figure 8.1 Pretreatment intraoral views of the initial therapy patient
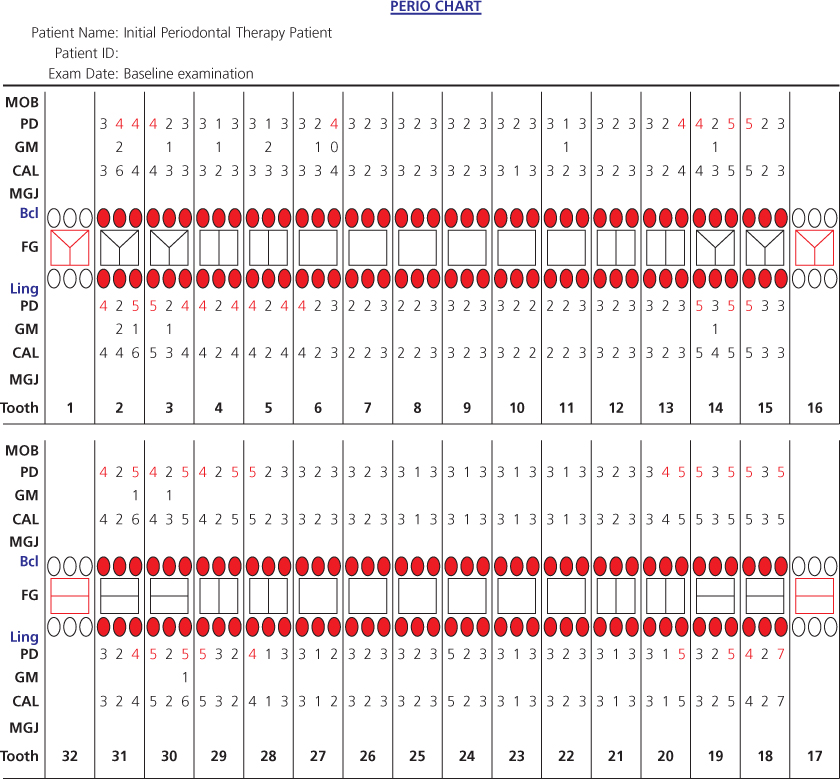
Figure 8.2 Baseline periodontal charting of the initial therapy patient
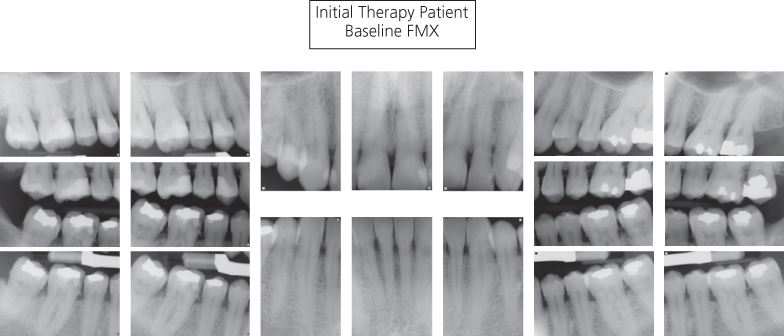
Figure 8.3 Baseline radiographs of the initial therapy patient
Radiographic examination
- Moderate bone loss with a vertical component was noted at teeth #2–3 (FDI 17, 16), 14–15 (FDI 26, 27) and distal to tooth #18 (FDI 37). Other posterior areas of mild horizontal bone loss were noted.
- Subgingival calculus deposits were noted interproximally at most teeth and distal to all second molars.
- Mesial root concavity was noted at tooth #5 (FDI 14).
Risk assessment and diagnosis
- Periodontal risk factors included tobacco use, lack of regular care and overweight (BMI of 29.8 places this patient in the overweight category).
- Diagnosis: Chronic periodontitis with isolated areas of slight to moderate loss of periodontal support.
- The lack of more generalized and advanced loss of periodontal support despite the patient’s risk factors, lack of previous care, and generalized heavy etiology was noteworthy.
Treatment planned
- Full mouth nonsurgical periodontal debridement scheduled over two sessions
- Crown—porcelain/ceramic substrate #3 (FDI 16), #5 (FDI 14), #15 (FDI 27), and #30 (FDI 46)
Periodontal treatment provided
Session 1:
- Initial ultrasonic debridement of maxillary right, mandibular right, and mandibular anterior sextants.
- 36 mg 2% lidocaine w/0.018 mg epinephrine administered via IANB
- 72 mg 4% articaine w/0.009 mg epinephrine administered via infiltration
Session 2:
- Initial ultrasonic debridement of maxillary anterior, maxillary left, and mandibular left sextants
- Supportive ultrasonic debridement of sextants previously treated at Session 1
- 36 mg 2% lidocaine w/0.018 mg epinephrine administered via IANB on the left
- 85 mg of a commercially-available 2.5% lidocaine/2.5% prilocaine anesthetic gel applied subgingivally to maxillary sextants
Discussion
Although the intent was to complete the initial debridement therapy in two sessions scheduled one week apart, the patient failed to show for the second appointment. Numerous attempts were made to reschedule him in a timely manner, but scheduling conflicts delayed the second session by three months. By then, reevaluation and supportive maintenance therapy in the sextants previously treated were indicated, and therefore, completed during the same appointment.
- INITIAL THERAPY
The presence of moderate–heavy calculus deposits required that initial debridement therapy be implemented in two stages. A standard diameter tip, straight by default and with one-bend, was utilized first, at a medium–high power setting, to reduce the calculus deposits to a lesser degree in both anterior (Figure 8.4) and posterior areas (Figure 8.5).
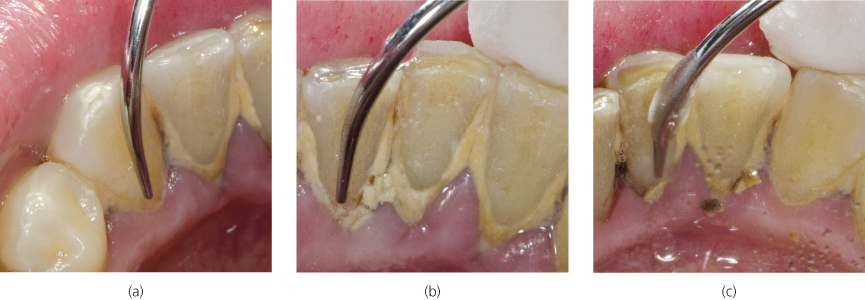
Figure 8.4 Standard diameter cylindrical tip vertically adapted at 0° angulation to the lingual surfaces of (a) #22 (FDI 33); (b) #24 (FDI 31); and (c) #25 (FDI 41)
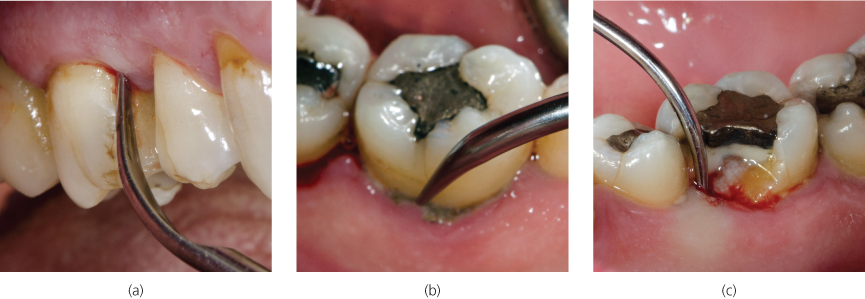
Figure 8.5 (a) Proper adaptation of rectangular standard tip to #3M (FDI 16); (b) tapping the point of the tip against heavy calculus at the gingival margin of #19L (FDI 36); (c) appropriate adaptation and advancement into the pocket at #30ML (FDI 46)
As the clinician is right-handed, scaling of the mandibular anterior lingual sextant commenced at the midline of #22 (FDI 33) (Figure 8.4a) and continued, following the transitional sequence, to the distal of #27 (FDI 43). Removal/reduction of the heavy supragingival calculus preceded subgingival scaling and occurred as the oscillating tip engaged with the edges of the supragingival deposits (Figure 8.4b,c)
Scaling of various posterior sextants is illustrated in Figure 8.5a–c. The rectangular standard tip utilized in the maxillary right buccal (Figure 8.5a) and mandibular left lingual (Figure 8.5b) sextants provided greater force against the heavy calculus deposits (without increasing the power setting), compared to the cylindrical standard tip utilized to scale the fractured surface in the mandibular right lingual sextant (Figure 8.5c). A tapping stroke (Figure 8.5b) was utilized to break up the heavy calculus deposits at the lingual gingival margins of the mandibular molar prior to initiating subgingival instrumentation.
Figure 8.6 illustrates implementation of the transitional sequence used to advance the tip, as described in Chapter 7, during scaling of the mandibular right buccal sextant.
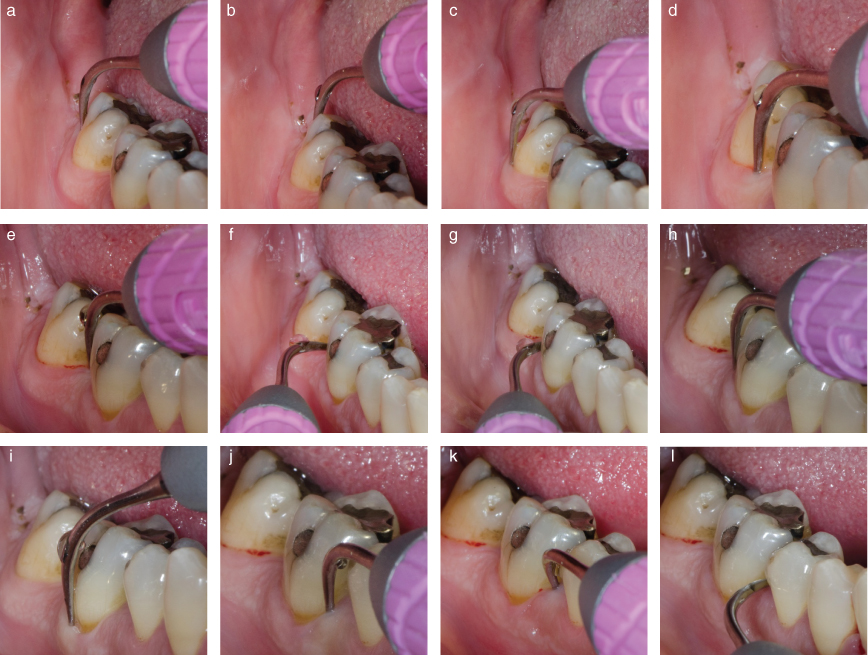
Figure 8.6 Proper adaptation and advancement of the tip is illustrated, beginning with (a) vertical adaptation at the DB line angle of #31 (FDI 47) and continuing, in sequential order, to (l) horizontal adaptation of the back of the tip to the mesial of #30 (FDI 46)
On removal or reduction of the calculus deposits in the posterior and anterior sextants, the clinician switched to slim diameter tips and appropriately reduced the power setting to medium to definitively scale any remaining calculus and optimize the debridement of biofilm from the root surfaces (Figures 8.7–8.9). Remember that a medium power setting is preferred over a low power setting for debridement, as medium power produces the greatest amount of cavitation without inherently over-instrumenting the root surface (Chapter 3).
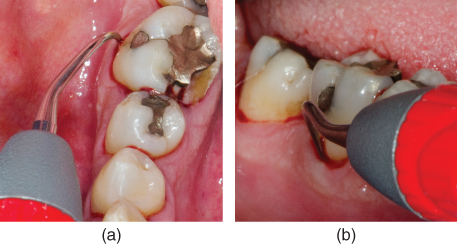
Figure 8.7 Vertical adaptation of the right curved tip at 0° to the buccal surface of #30 (FDI 46), as visualized from (a) occlusal and (b) buccal perspectives
The “correct” site-specific curved tip (right or left), that is, the configuration indicated for the treatment site, can be easily identified from the occlusal perspective (Figure 8.7a), as the contra-angle of the tip will bend toward the tooth, allowing for vertical adaptation of the active area, with the point of the tip directed away from the tooth.
The right curved tip was also utilized for debridement of the maxillary right palatal surfaces. As the tip crossed the ML line angle of #3 (FDI 16), the back of the tip adapted to the mesial surface (Figure 8.8a). Oblique strokes were implemented to advance the tip subgingivally and mesially across the mesial surface. Contact between the back of the tip and the mesial surface was maintained as the tip was transitioned to horizontal adaptation in the interproximal space (Figure 8.8b) and stroked vertically.
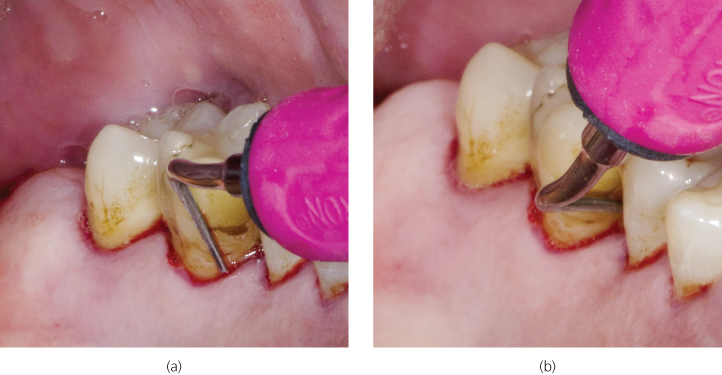
Figure 8.8 Adaptation of the right curved tip in the maxillary right palatal sextant as visualized from the perspective of the right-handed clinician positioned at 12:00
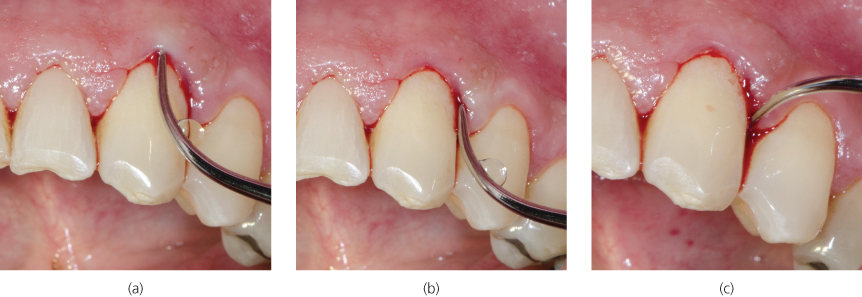
Figure 8.9 Advancement of a straight slim tip on the facial surface of #27 (FDI 43) from (a) midline to (b) the distal surface to (c) the distal interproximal space (from viewpoint of a right-handed clinician positioned at 12:00)
For debridement of the facial surfaces of the mandibular anterior sextant, either the left curved or a straight slim or ultraslim tip design can be utilized. In this case, the clinician opted to use a straight slim diameter tip.
As the mandibu/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


