7
Tooth Impaction
Introduction
Failure of eruption or impaction of a tooth is a commonly encountered problem in orthodontics and affects almost 20% of the general population. With the exception of third molars, the most commonly impacted permanent teeth occur in the maxilla and include canines, second molars, central incisors and first molars (Kurol and Bjerklin, 1982; Bishara, 1992; Bondemark and Tsiopa, 2007). General causes of failed eruption include mechanical obstruction, ectopic dental development with the tooth assuming an abnormal position, or a failure of the eruption process itself.
Causes of mechanical obstruction include crowding, resulting in insufficient space to accommodate the tooth in the dental arch, and the presence of supernumerary teeth physically blocking the tooth from erupting; the latter being the main cause of the failure of eruption of maxillary central incisors. Manifestations of ectopic dental development include palatally displaced maxillary canines, maxillary first molars impacted against the second primary molar and, less commonly, dental transpositions.
The reasons for tooth ectopia remain poorly understood. While there is a definite genetic component to true transpositions (Ely et al., 2006), the aetiology of ectopic eruption of palatally impacted maxillary canines is less clear. Epidemiologically, there are racial and gender differences, implying a degree of familial inheritance (Peck et al., 1994). There is also an association with aberrant or missing lateral incisors, implying that eruption of the canine is guided by the root of the lateral incisor and indicating a mechanical cause for the ectopia (Brin et al., 1986). However, given that tooth size and form is also under genetic control, ectopic maxillary canines in conjunction with absent or diminutive lateral incisors also implicates an inherited pattern in ectopia. Failure of the eruptive process is also seen in teeth that have become ankylosed following trauma and in cleidocranial dysplasia.
Occasionally, teeth can fail to erupt or to erupt fully, with no obvious cause for the defective eruption. This rare condition may affect a group of teeth (primary failure of eruption) or may be confined to one tooth (mechanical failure of eruption) with teeth posterior to the affected tooth erupting normally (Proffit and Vig, 1981; Frazier-Bowers et al., 2007). Specific mutations leading to primary failure of eruption have been identified (Frazier-Bowers et al., 2010).
Correct diagnosis of unerupted teeth requires comprehensive records, often involving radiographs to locate the tooth and identify any associated pathology. Location usually involves two radiographs taken at different angles to the impacted tooth using the principle of parallax, whereby apparent movement of an impacted tooth will occur due to movement of the X-ray tube. The advent of cone beam computed tomography (CT) scanning has helped in accurately locating impacted teeth, highlighting higher levels of root resorption of adjacent teeth than are apparent on normal films (Walker et al., 2005). Three-dimensional imaging is also becoming increasingly useful in planning treatment and mechanics, permitting visualization of the potential path of eruption, particularly for palatally ectopic canines (Ericson and Kurol, 1987, 2000a).
Whilst asymptomatic impacted third molars may be routinely left untreated, problems may arise with unerupted teeth, including dentigerous cyst formation and pathological resorption of adjacent teeth. Active management varies depending upon the presentation, particularly the position of the impacted tooth and the underlying malocclusion. Treatment may range in complexity from simple interceptive removal of the overlying primary tooth to mechanical eruption, surgical removal or even auto-transplantation of the impacted tooth (Ericson and Kurol, 1988a). With profound failure of the eruptive process, the options are more limited, as these teeth are invariably not amenable to orthodontic tooth movement. In general, however, optimal treatment usually involves space redistribution to accommodate the impacted tooth in the dental arch, followed by surgical exposure if the tooth fails to erupt with mechanical traction via an orthodontic fixed appliance. Thus, the management of impacted teeth routinely necessitates a multidisciplinary approach involving both orthodontist and oral and maxillofacial surgeon.
Case 7.1
| Extra-oral | |
| Skeletal relationship | |
| Antero-posterior | Skeletal class II |
| Vertical | FMPA: Average |
| Lower face height: Average | |
| Transverse | Facial asymmetry: None |
| Soft tissues | Normal protrusion |
| Lip competence: Competent | |
| Naso-labial angle: Obtuse | |
| Upper incisor show | At rest: 3 mm |
| Smiling: 7 mm | |
| Temporo-mandibular joint | Healthy with good range and co-ordination of movement |
| Intra-oral | |
| Teeth present |  |
| Dental health | Good |
| (restorations, caries) | |
| Oral hygiene | Good |
| Lower arch | Crowding: Moderate |
| Incisor inclination: Average | |
| Curve of Spee: Average | |
| Upper arch | Crowding: Moderate |
| Incisor inclination: Average | |
| Canine position: Buccal | |
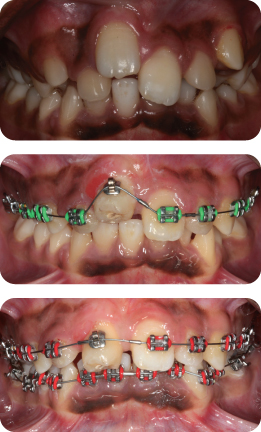
Summarize the Occlusal Features (Figure 7.1)
- Incisor relationship: Class I
- Overjet: 2 mm
- Overbite: Reduced and complete
- Canine relationship: Class I on left; 1/2 unit class II on right
- Molar relationship: Class I on right; 1/2 unit class II on left
- Centre lines: Co-incident with each other and facial midline
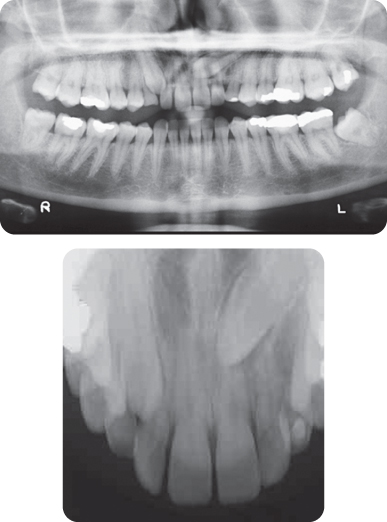
What Additional Information Does the Panoramic Radiograph Provide (Figure 7.2)?
The LL5 is ectopic, being horizontally orientated. The follicle surrounding this tooth is slightly enlarged. Some minor root resorption of the LLE has occurred; however, the form and length of the roots are good, and there is no caries or coronal restoration.
Summary
A 13-year-old female presented with a class I incisor relationship on a mild skeletal class II base complicated by the presence of an impacted LL5 in a poor developmental position and a retained LLE (Figure 7.1).
Treatment Plan
- Surgical removal of the LL5 and extraction of the UR4, UL4, LR5 and LLE
- Upper and lower pre-adjusted edgewise appliances
- Long-term retention
The final occlusal result is shown in Figure 7.3.
Why Are the LL5, UR4, UL4, LR5 and LLE Being Extracted?
The ectopic position of the LL5 tooth is not favourable for surgical exposure and accommodation in the lower arch. The presence of moderate crowding in both arches means that space is required for alignment and this is provided by loss of the LLE, LL5 and three further premolar units.
Could this Patient Have Been Treated Without Extractions? If So, Comment on the Relative Merits of Such an Approach in this Case
Yes. This approach would have allowed advancement of the labial segments to provide additional soft tissue support and improve the facial profile. This would have placed a premium on permanent fixed retention in the lower labial segment to limit relapse potential. Furthermore, mechanical eruption and alignment of the LL5 would have been complex and prolonged, extending treatment time significantly. If mechanical eruption of the LL5 were unsuccessful, prosthetic replacement of the LL5 would have been necessary. Therefore, an alternative plan may have involved removal of the LL5 only, with indefinite preservation of the LLE. However, surgical removal of the LL5 without causing any damage to the LLE might be difficult to achieve.
Is There Any Association between an Enlarged Dental Follicle and Dentigerous Cyst Formation?
The follicular sizes of unerupted canines developing ectopically and those developing normally have been compared (Ericson and Bjerklin, 2001). Little difference in follicle size was noted between the groups. Follicles developing into cysts were also indistinguishable on CT scans from those that had been enlarged physiologically.
Could Auto-Transplantation of the LL5 Have Been Considered?
Yes. If this approach were undertaken, the malocclusion would have been treated on a non-extraction basis. However, this approach was not considered viable, as auto-transplantation requires successful atraumatic removal. As the LL5 was severely displaced, this would not have been possible. Furthermore, the ideal time had passed, as in excess of two-thirds of the root of the LL5 had formed.
How Successful Is Auto-Transplantation of Teeth?
Success rates of up to 98% have been reported in Scandinavia (Andreasen et al., 1990; Czochrowska et al., 2002). However, success is related to careful surgical technique and experience. Transplants are performed less frequently in the UK and North America. However, a recent retrospective analysis of maxillary canine transplantation carried out in a UK hospital setting has suggested a mean survival period for transplants of over 14 years (Patel et al., 2011).
What Factors Influence the Success Rate of Auto-Transplantation?
- Surgical technique
- Degree of root maturity
- Donor tooth and site
- Size of the apical foramen
Transplantation of mandibular second premolars to the maxillary central incisor region is particularly successful (Kvint et al., 2010). The second premolar is rotated 90 degrees to occupy the correct amount of space and to improve gingival aesthetics. In Figure 7.4 a mandibular second premolar has been autotransplanted to replace a UR1.
Case 7.2
| Extra-oral | |
| Skeletal relationship | |
| Antero-posterior | Skeletal class I |
| Vertical | FMPA: Average |
| Lower face height: Average | |
| Transverse | Facial asymmetry: None |
| Soft tissues | Lip competence: Competent |
| Naso-labial angle: Average | |
| Upper incisor show | At rest: 3 mm |
| Smiling: 8 mm | |
| Temporo-mandibular joint | Healthy with good range and co-ordination of movement |
| Intra-oral | |
| Teeth present |  |
| Dental health | Good |
| (restorations, caries) | Restorations in first permanent molars |
| Oral hygiene – periodontal | Good |
| Lower arch | Crowding: Mild |
| Incisor inclination: Average | |
| Curve of Spee: Average | |
| Upper arch | Crowding: Mild |
| Incisor inclination: Average | |
| Canines unerupted | |
Summarize the Occlusal Features in Figure 7.5
- Incisor relationship: Class I
- Overjet: 3 mm
- Overbite: Average and complete
- Canine relationship: Both primary maxillary canines retained
- Molar relationship: Class I on left; 1/4 unit class II on right
- Centre lines: Upper 2 mm to left and lower 1 mm to right of facial midline
- Functional occlusion: Group function
Describe the Position of the Maxillary Canines (Figure 7.6)
Both maxillary canines are ectopic. The UR3 is vertically-orientated, with the tip overlying the lateral incisor. The UL3 is severely displaced. On the panoramic view, the canine tip has crossed the midline of the central incisor, has a mesial angulation and is also vertically displaced. There is no evidence of associated pathology.
The position of the UL3 can also be assessed using vertical parallax. The tooth appears to move upwards on the anterior occlusal view relative to the adjacent central incisor when compared to its relationship to this tooth on the panoramic view. As the tooth has appeared to move in the direction of the tube-shift, it is palatally placed.
Summary
A 26-year-old female presented with a class I malocclusion on a skeletal class I pattern with average vertical dimensions complicated by ectopic palatal maxillary canines (Figures 7.5 and 7.6).
Treatment Plan
- Extraction of the primary canines and surgical open exposure of the maxillary permanent canines
- Upper and lower pre-adjusted edgewise appliances to align the teeth and accommodate the canines
- Long-term retention
List the Reasons for the High Prevalence of Impacted Maxillary Canines
- Long, tortuous eruption path
- Displacement of developing tooth germ
- Congenital absence of maxillary lateral incisors
- Diminutive maxillary lateral incisors
- Commonly erupts after the maxillary first premolar, making it susceptible to crowding
- Retention of primary canines
- Ankylosis
- Trauma
- Pathology
What Appliances May Be Used to Mechanically Erupt Maxillary Canines?
Although upper or lower removable appliances may be used as adjuncts to permit eruption of canines, the mainstay of treatment involves fixed appliances.
What Auxiliaries May Be Used in Conjunction with Fixed Appliances to Permit Mechanical Eruption?
- Elastomeric traction
- Piggy-back archwires
- Customized auxiliaries
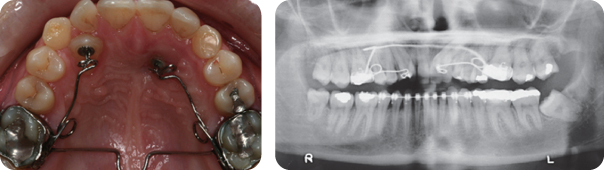
What Was Used in this Case (Figure 7.7)?
A trans-palatal arch with two auxiliary springs was fitted. This has the advantage of re-enforcing anchorage and providing a means of applying a distally-orientated extrusive force on the canines.
What Reactionary Forces May Arise During Treatment?
A reactionary intrusive force on the adjacent teeth may arise. Mesial tipping of the maxillary buccal segments and narrowing of the maxillary arch may also occur.
How Are Unfavourable Reactionary Forces Minimized During Eruption of the Canine?
Mesial tipping of the buccal segments and constriction of the maxillary arch may be limited by the use of a trans-palatal arch. Vertical anchorage may be augmented using rigid stainless steel base archwires (0.018 or 0.019 × 0.025 inch) while applying vertical traction to the displaced tooth. Temporary anchorage devices may also be used to facilitate distal and vertical canine movement while resisting reactionary forces.
What Type of Surgical Exposure of Impacted Canines May Be Undertaken?
- Open exposure
- Apically-repositioned flap
- Closed exposure and bonding
What Factors Govern the Choice of Exposure Type?
Exposure type is governed primarily by the position of the tooth and individual preferences of the treating clinicians. Superficial palatally-displaced canines lend themselves to open surgical exposure; deeper impactions and those in the line of the arch are more suited to closed exposure and bonding to avoid excessive bone removal and damage to adjacent teeth, respectively. Apically-repositioned flaps may be considered with teeth lying labially or in the line of the dental arch where the crown is covered by a band of attached gingiva.
What Is the Expected Duration of Treatment to Align an Ectopic Canine?
Treatment duration varies considerably for canine ectopia, with more severe impactions likely to require an extended period of treatment. An average treatment duration of almost 29 months has been reported to align an impacted canine prior to commencing finishing procedures (Iramaneerat et al., 1998).
Is There a Difference in Overall Treatment Duration with Different Exposure Types?
Research in this area would suggest little difference in treatment time, although these studies have all been retrospective in design. One study reported a time saving of 4 months with open exposure (Wisth, 1976), whilst another described open exposure taking 4 months longer (Pearson et al., 1997). A further study has reported no difference in treatment duration (Iramaneerat et al., 1998).
Outline the Risks of Treatment Involving Mechanical Eruption of Impacted Canines
Most canines are treated successfully without deleterious consequences. However, specific risks include:
- Root resorption of neighbouring teeth
- General root resorption
- Pulpal obliteration with discolouration of the crown
- Crestal bone loss
- Decalcification
- Poor compliance
- Treatment failure.
Are the Positions of these Canines Likely to Be Stable Following Their Mechanical Eruption (Figure 7.8)?
Post-treatment changes are likely following any orthodontic intervention with inadequate retention. Following alignment, maxillary canines can be more prone to changes, including mesial rotation, lingual displacement and intrusion (Woloshyn et al., 1994).
What Other Options Exist in this Case If the Patient Is Not Prepared to Wear Fixed Appliances?
- No treatment. However, the impacted canines should be periodically reviewed for any signs of pathology; the long-term prognosis for the ULC and URC is poor.
- Extraction of the impacted canines and primary canines followed by restorative replacement.
- Extraction of the primary canines and auto-transplantation of the impacted canines. This strategy is complicated by the fact that the coronal width of the primary canines is less than that of the permanent canines, which in the absence of any orthodontic treatment means that transplantation can be difficult, although the transplanted canines can be rotated slightly to take up less space. In addition, the position of the UL3 is not conducive to atraumatic removal.
Case 7.3
| Extra-oral | |
| Skeletal relationship | |
| Antero-posterior | Skeletal class II |
| Vertical | FMPA: Average |
| Lower face height: Average | |
| Transverse | Facial asymmetry: None |
| Soft tissues | Lip competence: Competent |
| Naso-labial angle: Average | |
| Upper incisor show | At rest: 2 mm |
| Smiling: 6 mm | |
| Temporo-mandibular joint | Healthy with good range and co-ordination of movement |
Describe the Intra-Oral Findings
- Teeth present
UR1 is unerupted - Dental health (restorations, caries): Active caries in LR6
- Oral hygiene: Reasonable, some gingival inflammation associated with the UR3
- Lower arch:
- Crowding: Moderate
- Incisor inclination: Average
- Curve of Spee: Average
- Upper arch:
- Crowding: Potentially moderately crowded
- Incisor inclination: Average
Summarize the Occlusal Features
- Incisor relationship: Class II division 1 (the UR1 is unerupted)
- Overjet: increased (to 5 mm)
- Overbite: Increased and complete
- Molar relationship:
- Class II on right side
- Class I on left side
- Centre lines:
- Upper 2 mm to right side
- Lower correct to facial midline
Are There Any Other Features of Note from the Clinical Examination?
The maxillary incisors and mandibular second premolars are significantly enlarged, introducing a Bolton tooth-size discrepancy.
What Are the Radiographic Findings (Figure 7.9)?
- All teeth are present, including the UR1 and third molars
- UR1 is vertically-orientated, crowded, with complete root development and no evidence of dilaceration or associated pathology
- UL1 had a short root form
- LR6 is grossly carious
- An unerupted conical supernumerary is present in the lower right premolar region, with no associated pathology
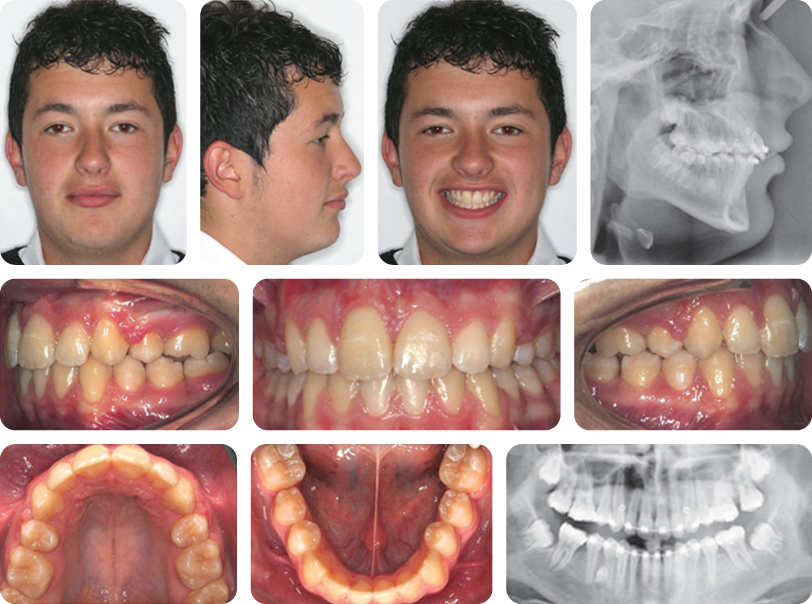
Summary
A 15-year-old male presented with a class II division 1 incisor relationship on a mild skeletal class II base, complicated by the presence of:
- Impacted UR1
- LR6 of poor long-term prognosis
- Potentially moderate crowding in both dental arches
- An unerupted supernumerary tooth in the lower right quadrant.
Treatment Plan
- Oral hygiene instruction
- Exposure and bonding of UR1. Removal of the unerupted supernumerary in the lower right quadrant was suggested; however, the patient decided against this due to the risk of surgical morbidity. Therefore upper and lower pre-adjusted edgewise appliances were used in conjunction with the extraction of upper first premolars and lower first permanent molars. The unerupted supernumerary was left in situ
- Long-term retention
The final treatment result is shown in Figure 7.10.
What Are the Possible Causes of Impacted Central Incisors?
- Supernumerary teeth
- Dilaceration
- Trauma
- Retained primary tooth
- Ankylosed primary tooth
- Systemic causes
Comment on the Anchorage Demands in this Case
The anchorage demand was high in the upper right quadrant, necessitating inter-maxillary class II traction and individual retraction of the UR1 into a class I relationship prior to consolidation of space in the maxillary arch. Vertical anchorage was also necessary to allow mechanical eruption of the UR1; this was provided by a rigid 0.018-inch steel-base archwire in conjunction with a nickel–titanium piggy-back archwire.
Are There Any Problems Associated with the Use of Fixed Appliances in this Case?
The UL1 has a short root form. Short, tapered, thin and pipette-shaped roots are predisposed to further root resorption during appliance therapy. The risk of resorption during treatment is related to longer treatment times and greater apical movement. In particular, the following should be undertaken with caution:
- Inter-arch elastics
- Torque application
- Intrusion.
What Factors Govern the Likelihood of Spontaneous Eruption of a Central Incisor Following Removal of the Supernumerary?
- Adequate space
- Position of the incisor and displacement of the apex
- Morphological type of supernumerary (Ashkenazi et al., 2007)
- Chronological age (Leyland et al., 2006)
How Likely Is Spontaneous Eruption Following the Removal of a Supernumerary Alone, Without Resort to Orthodontic Treatment?
Retrospective studies have suggested spontaneous eruption occurs in up to 92% of cases, although other studies have demonstrated lower success rates (DiBiase, 1969; Mitchell and Bennett, 1992; Leyland et al., 2006). In many of these, orthodontic alignment is required to improve the final position of the impacted tooth. As a general anaesthetic is often required to remove the supernumerary, concurrent exposure of the unerupted incisor is usually performed to avoid the risk of a further anaesthetic.
Does Spacing in the Anterior Region Have an Impact on Oral Health-Related Quality of Life (OHrQoL)?
A significant association has been demonstrated between impaired OHrQoL and both visible spacing and increased overjet. In one study, the OHrQoL of parents of affected children was also impaired (Johal et al., 2007). Consequently, successful management of impacted incisors is of benefit to dental, social and psychosocial health.
What Measures May Be Taken to Identify and Manage Progressive Resorption of the Central Incisor?
A mid-treatment radiograph is advocated to assess root resorption during treatment, as a significant correlation between resorption arising during the first 6 months of treatment and overall root resorption has been demonstrated (Smale et al., 2005). If significant progressive resorption is noted, consideration may be given to pacifying the appliance for 2–3 months (Levander et al., 1994).
Case 7.4
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses