3
Class I Malocclusion
Introduction
A class I malocclusion is associated with a class I incisor relationship and an Angle class I molar relationship. However, the molar relationship is not immutable; it can be affected by dental factors and may not truly represent the underlying skeletal relationship. The skeletal pattern is usually class I, with any variation from this being generally mild antero-posteriorly. In the vertical dimension a larger range of difference can be seen; from a slightly increased overbite to a frank anterior openbite with an associated increase in the lower face height. A markedly increased overbite is incompatible with the definition of a class I incisor relationship and is more in the domain of a class II division 1 or a class II division 2 malocclusion. Again, by definition, the overjet is within the normal range, although cases of bi-maxillary proclination can have a class I incisor relationship with an increased overjet or even slightly reduced overjet. The soft tissues in class I cases are generally favourable and rarely have a significant influence on the malocclusion, although an increased lower face height and anterior openbite is usually associated with lip incompetence and bi-maxillary proclination may occur in association with lip protrusion.
A spectrum of dento-alveolar problems can be seen in class I malocclusions, including dental crowding, crossbite and open bite. Crowding or dento-alveolar disproportion is one of the commonest manifestations of a class I malocclusion. Indeed, in developed countries crowding is endemic and has become more prevalent over the last century. There has been much speculation why this is the case. Lack of inter-proximal attrition or jaw development as a result of a soft diet has been implicated (Begg, 1954; Varrela, 2006). However, compared to isolated communities, most Western societies represent significant genetic heterogeneity and as such, there is probably a large genetic component to the increased incidence of crowding that has been reported.
Transverse or vertical problems can have a variety of causes. An anterior open bite can be skeletal in origin, secondary to a hyper-divergent facial form, or due to failure of incisor eruption following a persistent non-nutritive sucking habit. An important part of diagnosis is therefore to define the aetiology, as this determines the treatment aims and mechanics. Posterior crossbites can be associated with digit sucking or a skeletal discrepancy and facial asymmetry. In the former, simple dental expansion is usually appropriate, but in the presence of skeletal discrepancy this is often inappropriate.
Treatment planning is influenced primarily by the dento-alveolar features of the malocclusion, as the skeletal pattern is generally class I:
- Orthodontic treatment: The treatment of crowding usually requires comprehensive upper and lower fixed appliance therapy with or without the extraction of permanent teeth. Mild crowding can usually be managed without extraction, space being created by distalization of arches, utilization of the Leeway space or inter-proximal reduction (Cetlin and Ten Hoeve, 1983; Sheridan, 1985; Brennan and Gianelly, 2000). Excessive lower arch expansion or proclination of the lower incisors should generally be avoided as this is inherently unstable (Ackerman and Proffit, 1997). In severe crowding the extraction of teeth is usually required. The premolars are often the teeth of choice as they are close to the site of labial crowding and are of similar size and form in the maxillary and mandibular arch. A vocal minority has made much of the possible detrimental effects associated with elective orthodontic tooth extraction, particularly in relation to the effect on the soft tissue profile and as a cause of temporo-mandibular dysfunction. However, to date there is no evidence that the use of extractions, when appropriate and as part of a properly planned course of treatment, leads to any long-term problems. As such, extractions remain a valuable tool to address dento-alveolar disproportion (DiBiase and Sandler, 2001).
- Orthodontics and surgery: For those cases with a significant vertical skeletal component to their malocclusion, combined orthodontic–surgical treatment can be carried out. In growing patients, numerous techniques have been described to treat an anterior open bite, including extra-oral traction and repelling magnets designed to intrude the buccal dentition, all with limited success. More recently, mini-screws and plates have been introduced, which may in the long-term prove to be an effective alternative to surgery.
Case 3.1
| Extra-oral | |
| Skeletal relationship | |
| Antero-posterior | Mild skeletal class II |
| Vertical | FMPA: Average |
| Lower face height: Average | |
| Transverse | Facial asymmetry: None |
| Soft tissues | Lip competence: Competent |
| Naso-labial angle: Obtuse | |
| Upper incisor show | At rest: 4 mm |
| Smiling: 9 mm | |
| Temporo-mandibular joint | Healthy with good range and co-ordination of movement |
| Intra-oral | |
| Teeth present |  |
| Dental health (restorations, caries) | Good |
| Oral hygiene – periodontal | Poor with gingival hyperplasia labial to UL2 |
| Lower arch | Crowding: Mild |
| Incisor inclination: Average | |
| Curve of Spee: Average | |
| Upper arch | Crowding: Moderate |
| Incisor inclination: Average | |
| Canine position: Buccally placed | |
| Occlusion | Incisor relationship: Class I |
| Overjet: 3 mm | |
| Overbite: Average and complete | |
| Molar relationship: 1/4 unit class II bilaterally | |
| Canine relationship: 1/2 unit class II bilaterally | |
| Centre lines: upper centre line 1 mm to left | |
| Functional occlusion: Group function | |
Summary
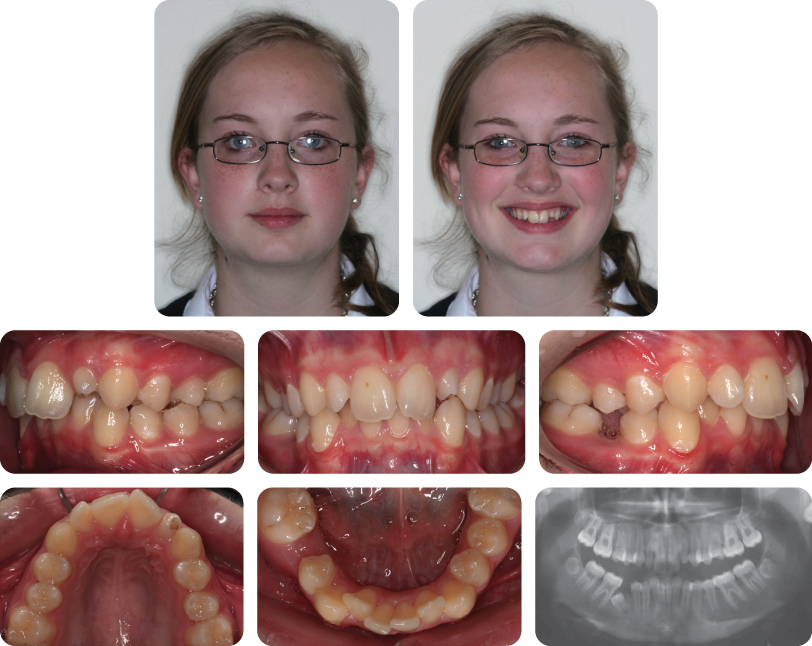
A 13-year-old female presented with a class I malocclusion on a mild skeletal class II pattern with average vertical dimensions complicated by moderate upper arch crowding, palatal displacement of the UL2 and a localized crossbite (Figure 3.1).
Treatment Plan
- Occipital pull extra-oral traction to reinforce anchorage
- Upper and lower pre-adjusted edgewise appliances
- Long-term retention
Treatment Progress
Headgear compliance was poor. It was therefore decided to remove both maxillary second premolars to recreate space for maxillary arch alignment (Figure 3.2).
What Options Were There in This Case in the Absence of Headgear Wear?
The initial aim of this case was to achieve a class I incisor relationship with distal movement of the upper molars. Distal molar movement would have facilitated upper arch alignment by space recreation. Consideration was given to use of a non-compliance class II corrector (Pendulum appliance, Forsus spring, Jasper jumper) to correct the molar relationship. However, it was decided to remove maxillary second premolars in view of the space and anchorage requirements.
Self-Ligating Brackets (SLBs) Were Used in This Case. What Are SLBs and What Are the Advantages of These Systems?
SLBs are brackets that use a clip or slide mechanism to engage the archwire rather than the application of ligatures. SLBs have demonstrated marked reductions in frictional resistance in laboratory studies, which might be expected to accelerate tooth movement and reduce orthodontic treatment time. However, clinical studies have largely failed to confirm this (DiBiase et al., 2011; Fleming et al., 2009, 2010; Scott et al., 2008). A slight advantage of SLBs is a possible reduction in chair-side time for the orthodontist (Turnbull and Birnie, 2007).
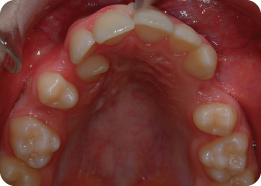
Describe What Is Happening in Figure 3.2
Both maxillary second premolars have been removed and the upper fixed appliance has been placed. An 0.013-inch nickel–titanium archwire is in place, with nickel–titanium coil spring being used between the UL1 and UL3 to recreate space and accommodate the UL2 in the arch. Simultaneously, elastomeric chain has been placed from the first molars to maxillary canines to aid retraction of these teeth. The UL2 has been ligated directly to the archwire to initiate labial movement of this tooth. Use of active mechanics on nickel–titanium archwires is traditionally not recommended due to the risk of loss of arch form, round tripping of teeth and unpredictable reactionary forces. However, some clinicians believe the secure ligation afforded by SLBs lends itself to this approach (Damon, 1998).
What Are the Arrows Pointing to in Figure 3.2 (Lower Panel)?
These are small metal stops placed on the archwire to prevent its excessive sliding through the SLBs, which can be a problem during the early stages of treatment because of the reduced static friction associated with these appliances. Without the use of stops, the archwire can slide into the soft tissues behind the molar bands and cause trauma.
Why Has Glass Ionomer Cement Been Placed on the Maxillary First Molars?
This is done to disengage the occlusion, facilitating correction of the crossbite involving the UL2. Removable appliances and fixed bite raisers may be used as an alternative.
What Is the Final Buccal Segment Relationship (Figure 3.3)?
The final canine relationship is class I; however, the molar relationship is class II because premolar units have been removed in the upper arch only.
Case 3.2
| Extra-oral | |
| Skeletal relationship | |
| Antero-posterior | Mild skeletal class II |
| Vertical | FMPA: Average |
| Lower face height: Average | |
| Transverse | Facial asymmetry: None |
| Soft tissues | Lip competence: Competent |
| Naso-labial angle: Average | |
| Upper incisor show | At rest: 4 mm |
| Smiling: 9 mm | |
| Temporo-mandibular joint | Healthy with good range and co-ordination of movement |
| Intra-oral | |
| Teeth present |  |
| Dental health | Good |
| (restorations, caries) | UL2 is diminutive with abnormal coronal morphology |
| Oral hygiene – periodontal | Good |
| Lower arch | Crowding: Moderate |
| Incisor inclination: Average | |
| Curve of Spee: Average | |
| Upper arch | Crowding: Mild |
| Incisor inclination: Average | |
| Canine position: Line of the arch | |
| Occlusion | Incisor relationship: Class I |
| Overjet: 3 mm | |
| Overbite: Average and complete | |
| Molar relationship: Class I bilaterally | |
| Centre lines: | |
| Upper centre line correct to mid-facial axis | |
| Lower centre line deviated 3 mm to right side | |
| Functional occlusion: Group function | |
What Are the Main Radiographic Findings (Figure 3.4)?
- LR5 is unerupted and distoangularly impacted against the LR6
- UL2 appears to be invaginated (dens in dente) with a short root form
- Upper third molars are absent but the lower third molars are developing
Summary
A 13-year-old female presented with a class I malocclusion on a mild skeletal class II pattern with average vertical dimensions complicated by impaction of the LR5 and an invaginated UL2 (Figure 3.4).
An opinion from a paediatric dentist suggested that the long-term prognosis for the UL2 was poor.
Treatment Plan
The moderate crowding in the lower arch was sufficient to indicate the need for extractions; in addition, the LR5 was impacted. Therefore, extraction of the LR5 and LL5 was indicated. Extraction in the lower arch dictated the need for extractions in the upper arch and, given the poor morphology associated with the UL2, a decision was made to extract this tooth. In the interests of symmetry, the UR2 was also extracted rather than a premolar in the upper right quadrant.
- Extraction of the UR2, UL2, LR5 and LL5
- Upper and lower pre-adjusted edgewise appliances
- Long-term retention
What Factors Need to Be Considered When Substituting a Maxillary Canine for a Lateral Incisor?
Canine substitution may be performed to place a canine in the position of a maxillary lateral incisor. This can be achieved by orthodontic tooth movement, localized bleaching, reshaping and direct restorative build-ups. Orthodontic considerations include the mismatch in gingival heights and requirement for palatal root torque. Palatal root torque is enhanced by using bracket prescriptions that already incorporate this or inverting brackets with a labial root torque prescription (Figure 3.5) and by using large-dimension finishing wires (0.021 × 0.025 inch). Reshaping of cusp tips is performed incrementally to limit pulpal responses and sensitivity, and to avoid sclerosis or devitalization in the longer term (Thordarson et al., 1991; Zachrisson and Mjor, 1975).
The Archwire Illustrated in Figure 3.6 is a Heat-Activated Nickel–Titanium Wire. What Properties Make It a Suitable Initial Aligning Wire?
Archwires during initial alignment are required to have a large range, low stiffness and adequate strength to resist occlusal forces (Kusy, 1997). Nickel–titanium archwires demonstrate all of these features in addition to a property called shape memory, which in conjunction with their high flexibility permits alignment of grossly-displaced and rotated teeth. Nickel–titanium wires are also claimed to display superelastic properties, with constant levels of force delivered at varying deflections.
What Are the Alternatives to Nickel–Titanium Wires During Initial Alignment?
- Multiloop stainless steel wires
- Co-axial or braided stainless steel wires
The flexibility of these steel wires is based on increasing the length of wire; however, their usability is poor, being susceptible to permanent deformation when fully engaged in teeth with more severe crowding.
Is There Any Evidence to Suggest That Orthodontic Alignment Is Accelerated with Nickel–Titanium Wires?
No. A recent systematic review considered seven randomized controlled trials comparing nickel–titanium wires and multi-strand stainless steel wires of varying dimensions. No differences in relation to the efficiency of alignment, root resorption and subjective pain experience were found (Wang et al., 2010).
How Have the Canines Been Modified Following Appliance Removal (Figure 3.7)?
The mesial tips have been built up with composite.
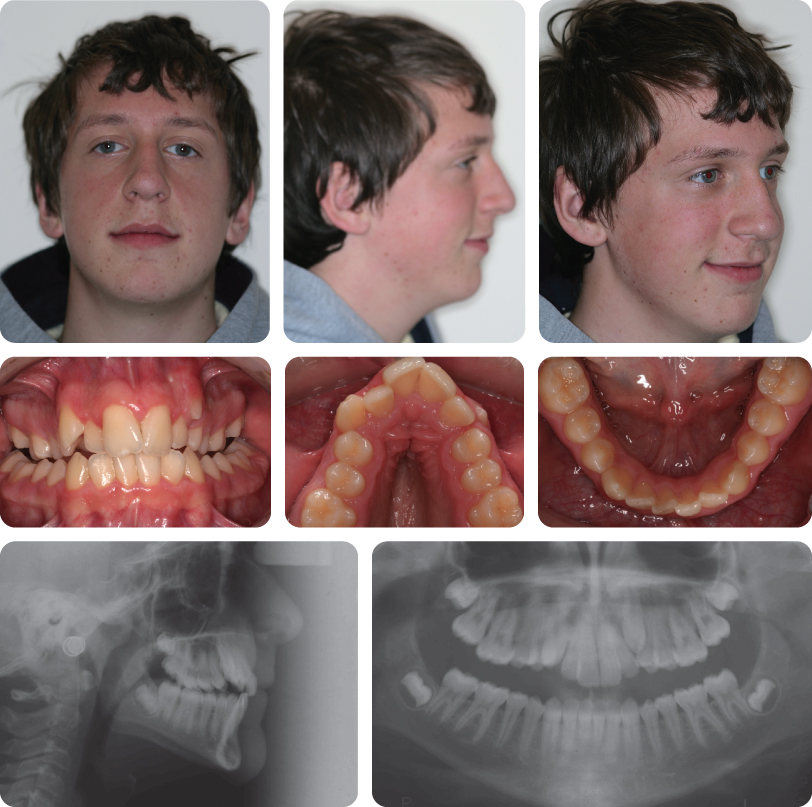
Case 3.3
| Extra-oral | |
| Skeletal relationship | |
| Antero-posterior | Skeletal class I |
| Vertical | FMPA: Average |
| Lower face height: Average | |
| Transverse | Facial asymmetry: None |
| Soft tissues | Lip competence: Competent |
| Naso-labial angle: Average | |
| Upper incisor show | At rest: 3 mm |
| Smiling: 6 mm | |
| Temporo-mandibular joint | Healthy with good range and co-ordination of movement |
| Intra-oral | |
| Teeth present |  |
| Dental health (restorations, caries) | Good |
| Oral hygiene – periodontal | Good |
| Lower arch | Crowding: Severe |
| Incisor inclination: Average | |
| Curve of Spee: Average | |
| Upper arch | Crowding: Moderate |
| Incisor inclination: Average | |
| Canine position: Palatal on right side; erupted on left | |
| Occlusion | Incisor relationship: Class I |
| Overjet: 3 mm | |
| Overbite: Average and complete | |
| Molar relationship: Class I on right side; 1/2 unit | |
| class II on left | |
| Centre lines: | |
| Upper 2 mm to right | |
| Lower 2 mm to left of facial midline | |
| Functional occlusion: Group function | |
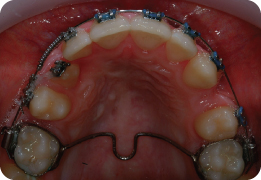
Radiographic Findings (Figure 3.8)
- UR3 is ectopic and mesially-angulated
- Cusp tip overlies the lateral incisor and has a favourable prognosis for mechanical eruption
- No evidence of associated pathology
- All third molars are developing
Summary
A 14-year-old male presented with a class I malocclusion on a skeletal class I base with average vertical dimensions complicated by an ectopic UR3, crowding of both arches and centre line discrepancies (Figure 3.8).
Treatment Plan
- Extraction of the UR5, UL4, LR5 and LL5
- Open surgical exposure of the UR3
- Trans-palatal arch
- Upper and lower pre-adjusted edgewise appliances
- Long-term retention
What Are the Common Causes of a Centre Line Discrepancy and How Can They Be Corrected?
Centre line discrepancies may arise due to skeletal asymmetries, particularly mandibular asymmetry, or more commonly due to dental asymmetries. Dental causes include asymmetric crowding, early loss of primary teeth, tooth-size discrepancies, hypodontia, supernumerary teeth, localized impactions and other pathology (Holmes et al., 1989). A mandibular deviation on closing (secondary to an anterior or posterior crossbite) can also cause a centre line discrepancy due to the displaced position of the mandible in the intercuspal position.
Centre line deviations of dental origin may be treated with unilateral or asymmetric extraction patterns, asymmetric mechanics (asymmetric headgear, push–pull mechanics and asymmetric inter-arch elastics) and elimination of any displacement. Centre line discrepancies of skeletal origin may also be masked using these techniques; however, significant asymmetries may warrant a combined orthodontic–surgical approach to permit complete correction.
What Has Happened in Figure 3.9?
An open surgical exposure of the UR3 has taken place. The tooth has subsequently been allowed to erupt for 3 months. Advocates of open surgical exposures favour this approach as it may permit autonomous eruption without recourse to active forces (Schmidt and Kokich, 2007).
What Mechanics Are Being Used in Figure 3.10?
An open nickel–titanium coil spring has been used on an 0.018-inch stainless steel archwire to recreate space for alignment of the UR3. The UR4 has been moved distally and the UR2 has been moved mesially to facilitate correction of the maxillary centre line. Elastomeric traction is also being used to move the UR3 buccally and distally. Anchorage support is provided by a trans-palatal arch. The UR2 and UR4 have been ligated with stainless steel ligatures to maintain rotational control of these teeth as space is created for the UR3.
Why Is 0.018-Inch Stainless Steel Favoured as a Base Archwire During This Treatment Phase?
Stainless steel arch wires have sufficient rigidity to provide anchorage and resist unwanted reactionary forces to the elastomeric traction (such as loss of arch form). Round steel wire also has relatively low frictional resistance; therefore sliding mechanics can be performed easily to recreate the space required to accommodate the canine in the arch.
Mandibular Second Molars Were Also Included in the Fixed Appliance. What Are the Advantages of This?
- Provide vertical anchorage facilitating overbite reduction
- Prevent mesial tipping of first molars during space closure
- Alignment of the second molars
Nickel–Titanium Closing Coils Are Being Used for Space Closure (Figure 3.11). Is There Any Evidence to Support Their Use?
Yes. Nickel–titanium closing coils have proven superior to elastomeric chains during space closure (Dixon et al., 2002; Nightingale and Jones, 2003; Samuels et al., 1998). However, their additional cost makes their use over alternative methods of space closure (elastomerics) less clear-cut.
What Force Level Should Be Used During Space Closure with Nickel–Titanium Closing Coils?
Force levels of approximately 150 g are considered ideal (Samuels et al., 1998). Lower levels result in slower tooth movement. Higher force levels do not increase the rate of tooth movement but may predispose to greater pain levels, undermining resorption and root resorption.
Figure 3.12 shows the final occlusion.
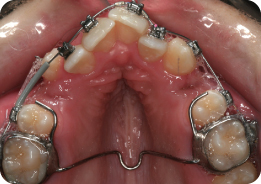
Case 3.4
| Extra-oral | |
| Skeletal relationship | |
| Antero-posterior | Mild skeletal class II |
| Vertical | FMPA: Increased |
| Lower face height: Increased | |
| Transverse | Facial symmetry: None |
| Soft tissues | Lip competence: Incompetent with lip strain to achieve anterior oral seal |
| Naso-labial angle: Average | |
| Upper incisor show | At rest: 3 mm |
| Smiling: 7 mm | |
| Temporo-mandibular joint | Healthy with good range and co-ordination of movement |
| Intra-oral | |
| Teeth present |  (The UL3 is partially erupted) (The UL3 is partially erupted) |
| Dental health | Good |
| (restorations, caries) | No restorations or active caries |
| Oral hygiene – periodontal | Moderate with localized marginal gingivitis |
| Occlusion | Incisor relationship: Class I |
| Overjet: 2 mm | |
| Overbite: Reduced and incomplete | |
| Molar relationship: Class II on the left side; 1/2 unit class II on right side | |
| Centre lines: | |
| Upper is 2 mm to left side | |
| Lower is coincident with facial midline | |
| Functional occlusion: Group function | |
| Lower arch | Crowding: Mild |
| Incisor inclination: Average | |
| Upper arch | Crowding: Severe |
| Incisor inclination: Average | |
| Canine position: Buccal | |
Summary
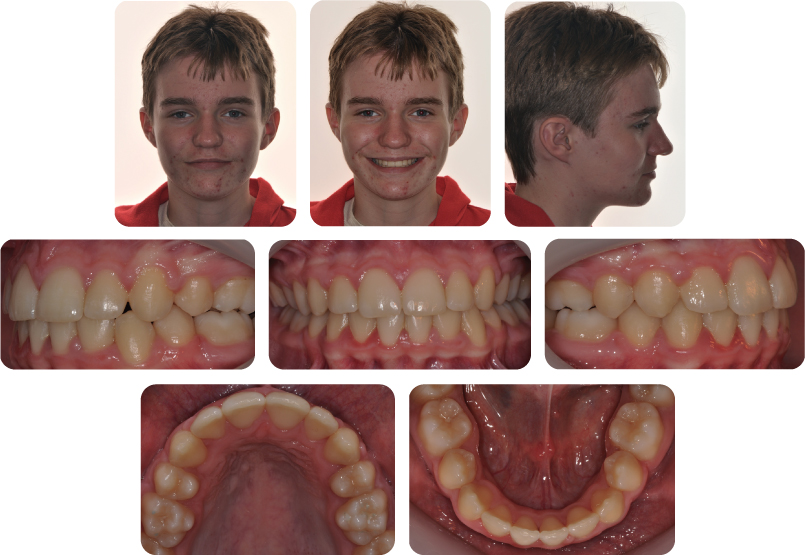
A 14-year-old male presented with a class I malocclusion on a mild skeletal class II pattern with increased vertical dimensions complicated by severe maxillary arch crowding, buccally-displaced maxillary canines, bilateral posterior crossbites and a reduced overbite (Figure 3.13).
Treatment Plan
- Improve oral hygiene
- Rapid maxillary expansion (Figure 3.14)
- Upper and lower pre-adjusted edgewise appliances with extraction of maxillary first premolars and mandibular second premolars
- Long-term retention
What Is the Biological Basis of Rapid Maxillary Expansion?
Rapid maxillary expansion (RME) is a form of palatal expansion used during adolescence. It relies on the presence of the mid-palatal suture, which in autopsy studies has been shown to remain patent until 15 years at least (Melsen, 1975). Appliances may be banded (usually on first premolars and first molars) or bonded to the buccal segment teeth. Expansion usually occurs at a rate of 0.5–1 mm per day, while slow expansion with removable appliances is usually undertaken at 0.25–0.5 mm per week. Over-expansion is usually desirable to allow for some relapse during fixed appliance therapy. The RME is usually left in situ for 3 months following the active phase of treatment to help maintain the expansion. Alternatively, a modified palatal arch can be fitted with palatal arms to maintain the expansion, which is a little less obtrusive than leaving the RME appliance in place.
How Is Arch Expansion Generally Achieved?
Arch expansion arises through a combination of bodily tooth movement and tipping. Tipping movements are likely to be unstable and may have bite-opening effects with inferior movement of supporting cusps resulting in a decrease of overbite. Tipping and bodily movements occur in a ratio of almost 1:1 with rapid expansion, while tipping movements predominate with more gradual forms of expansion, including removable appliances and quadhelices (Frank and Engel, 1982). Banded rapid expansion designs are commonly used; however, bonded designs may limit bite opening due to occlusal coverage posteriorly (Reed et al., 1999).
What Were the Main Options to Achieve Maxillary Arch Expansion in This Case?
- Removable appliances
- Fixed appliances:
- Quadhelix
- Bonded or banded RME
Why Was RME Used?
- Greater than 4 mm of expansion was required.
- Patient was of a suitable age and likely to have a patent mid-palatal suture.
- RME offers greater potential bodily movement, which would mean any likely bite opening effect may be less marked. This is important in this case because of the reduced overbite.
What Is the Role of the Cemented Appliance in Figure 3.15?
This is a modified trans-palatal arch. Its purpose is to retain the expansion generated with RME following removal of the active appliance. It is discarded when rigid stainless steel wires are engaged in the fixed appliance. The modification involves extending rigid wires from the first molar band to the second premolars.
Why Were Mandibular Second Premolars Extracted As Part of the Treatment Plan in This Case?
- Relief of crowding
- Transverse constriction of the mandibular arch
- Maintain a positive overbite
The Final Result Is Shown in Figure 3.16. Is Crossbite Correction Likely to Be Stable?
Maxillary arch expansion is inherently unstable. Prolonged follow-up suggests that significant reductions in transverse skeletal and dental dimensions occur following therapy (Lagravere et al., 2005a,b). Consequently, prolonged retention is necessary to maintain transverse increases, with rigid Hawley-type retainers recommended for this purpose. Removal of mandibular second premolars and transverse constriction is likely to be more stable and may contribute to the stability of crossbite correction.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses