7
Stability of Anterior Open Bite Correction—An Assessment of the Evidence
Background and Etiology of Open Bite
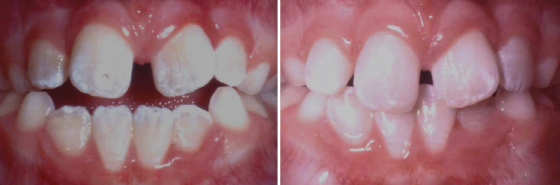
Ask any orthodontist what types of malocclusions are the most challenging to treat and anterior open bite is among those at the top of the list. The following examples illustrate the clinical range and complexity of open bite malocclusions (Figure 7.1). Not only is treatment difficult, retention can be even more challenging. This chapter will attempt to compile information on suspected etiologies of anterior open bite, the prevalence in various populations, and strategies that have been employed to treat open bite malocclusions. Additionally, the evidence on long-term stability after orthodontic treatment will be assessed. Finally, new techniques and strategies for addressing open bite malocclusions will be discussed.
Figure 7.1 Three examples of open bite malocclusion.

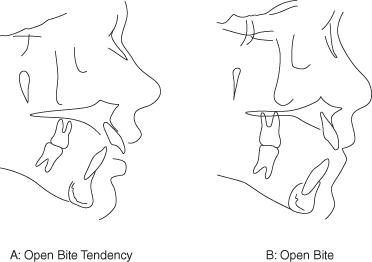
It may be helpful to propose some definitions. One clinical definition of anterior open bite may be the lack of incisor contact in centric occlusion. Another may be the lack of incisor overlap, as measured relative to a defined plane, such as the occlusal plane. Cephalometrically, the use of a reference plane to measure vertical relationships of the incisors seems reasonable, and several have been used. The occlusal plane is commonly employed as a reference, as are perpendicular lines to Frankfort horizontal and sella-nasion (or derivatives of sella-nasion). Another commonly used reference line is nasion-menton. Regardless of the reference line that is used, some factors to consider for cephalometric measurement are reliability in identifying the points that establish the plane of reference, reasonable geometric relationships to the measurement of interest, and stability of the reference plane over time. The definition of open bite and the measurement method employed can influence prevalence, diagnosis, success, and long-term stability. For the purposes of this chapter, an open bite tendency describes an anterior tooth relationship that does not display incisor contact but does have some vertical overlap of the incisors. Patients with open bite tendencies can often bring their incisors into contact on protrusion (Figure 7.2A). The true anterior open bite designation will be reserved for those individuals who have no vertical overlap of the incisors, as measured via a reference line such as occlusal plane or Nasion-Menton (Figure 7.2B). Distinction is sometimes made between dental and skeletal open bites:
- Dental open bites display normal skeletal relationships, with the open bite primarily due to vertical displacement of the incisors.
- Skeletal open bites are characterized by steep mandibular planes, divergent facial patterns (increased anterior facial height, shortened posterior facial height), and antegonial notching (Cangialosi 1984; Sassouni 1969).
Figure 7.2 Open bite tendency (A) and open bite (B).
Although the etiology of open bite is often difficult to confirm, many factors have been implicated. For example, various digit, lip, and other oral habits have been reported in the literature (Subtelny & Sakuda 1964; Swineheart 1942; Popovich & Thompson 1973). Some habits involve tongue function and/or posture (Swineheart 1942; Rogers 1927; Straub 1960, 1961, 1962). Historically, tongue thrusting during swallowing has been considered as a cause of open bites. Experiments by Proffit demonstrated that although forces from the tongue during swallowing are significant in magnitude, the duration of these forces is probably insufficient to cause anterior open bite (Proffit 1978). A large tongue, or a tongue that is habitually postured between the incisors, is another commonly cited etiologic factor. There does appear to be some literature that supports this theory, as therapies that address tongue posture appear to result in fairly good long-term stability (Justus 1976; Huang et al. 1990). Additionally, glossotomies for patients with macroglossia have been reported to assist in closing open bites (Kawakami et al. 2005; Hotokezaka et al. 2001; Ball & Horrocks 1995; Ruff 1985). Prolonged pacifier use has also been found to be related to an increased incidence of anterior open bite (Gois et al. 2008; Verrastro et al. 2007; Warren et al. 2005; Adair et al. 1995). Obviously, discontinuing these habits, if possible, is the first step in trying to address the open bite.
It is commonly asked if open bites cause behaviors such as altered swallowing and speech or if these altered behaviors result in or perpetuate open bites. This “chicken or the egg” dilemma is difficult to answer with the existing literature. In past decades, speech and tongue function have been implicated as etiologic factors, and speech and myofunctional therapy have been recommended as treatments for open bite (Mason 2008; Haruki, Kishi & Zimmerman 1999; Benkert 1997; Zimmerman 1989; Garliner & Gables 1982). However, the scientific evidence on the success rate and long-term benefits of these therapies is lacking.
Airway has also been thought to be a contributor to anterior open bite, specifically in those whose primary mode of respiration is by mouth. Many investigators have studied the relationship between mouth breathing and anterior open bite in animal and human studies (Linder-Aronson 1970; Mahony, Karsten & Linder-Aronson 2004; Bresolin et al. 1983; Sassouni et al. 1985; Soukiet et al. 2009). There do appear to be some relationships, but these correlations are not always consistent(Fields et al. 1991; Vig KW. 1998).
Another causative factor may be genetics, which encompasses several entities. For example, unfavorable growth patterns have also been described as being associated with open bite (Sassouni 1969; Subtelny & Sakuda 1964; Schudy 1965; Bjork 1969). Many open bite patients do have divergent facial patterns and/or long faces. Also, patients with open bite have been reported to have weak musculature, which could be classified under genetic influence (Bakke & Michler 1991).
Sometimes patients are born with or develop neurological or neuromuscular deficits that can influence facial growth patterns and the vertical relationships of the teeth. For example, it is not uncommon that subjects with cerebral palsy or other developmental disabilities exhibit open bite (Asdaghi Mamaghani, Bode & Ehmer 2008; Carmagnani et al. 2007; Vittek et al. 1994). Likewise, patients affected by muscular dystrophy often have a higher occurrence of open bite (Ghafari et al. 1988; Kiliaridis, Mejersjo & Thilander 1989; Erturk & Dogan 1991; Morel-Verdebout, Botteron & Kiliaridis 2007).
Changes to the morphology of the condyle may also result in open bite. These changes may be sudden, as occurs in traumatic injuries, or progressive, as in idiopathic condylar resorption, arthritic processes, or avascular necrosis of the condyle (Hoppenreijs et al. 1998a). In any case, the usual result is a shortening of the posterior facial height, causing a clockwise rotation of the mandible around the molars, which act as a fulcrum, as the muscles of mastication elevate the ramus superiorly.
A careful diagnosis should be made to determine the possible cause of each patient’s open bite. If the etiologic factor can be identified and addressed, orthodontic treatment should have a higher chance for stability in the vertical dimension. If identification of the etiologic factor is ignored, stability will be unpredictable.
Prevalence of Open Bite
Several papers report on the prevalence of open bite, and prevalence appears to be related to various factors, such as age and race. The best data in the United States comes from the U.S. Health and Vital Statistics (Kelly, Sanchez & Kirk 1973; Kelly & Harvey 1977) and from NHANES III (Brunelle, Bhat & Lipton 1996). These surveys from the early 70s and early 90s, respectively, report on the prevalence of open bite among different races and age ranges.
Table 7.1 Open bite prevalence (2 mm or more).
Data from: U.S. Health and Vital Statistics, 1973–1974.
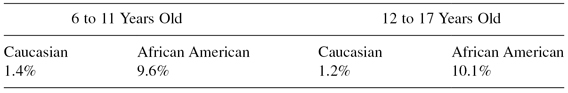
Sample consisted of 8000 subjects in each age range.
Table 7.2 Distribution of subjects with open bite.
Data from: NHANES III, 1989–1994.
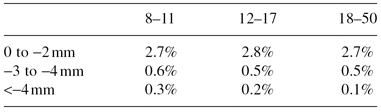
Sample consisted of 14,000 subjects, weighted to represent the population of Caucasian, African American, and Hispanic citizens of the United States.
Interestingly, there is considerable variation by race. Within each race, the prevalence is quite stable over the various age categories. These findings lead us to wonder how many of these open bite subjects are getting treatment and how often treatment leads to stable results.
A question that commonly arises is “how often do open bites spontaneously correct?” Several studies have addressed this question with cross-sectional data. Perhaps the most commonly cited one is a cross-sectional study conducted by Worms and colleagues (1971). He classified open bites into three categories: (1) pseudo-open bite—those with no incisor contact but positive overlap; (2) simple open bite—those with no overlap from canine to canine; and compound open bite—indicating open bite from premolar to premolar. Using Worm’s data for the simple and compound open bites, whose definitions are consistent with the classification of “true” open bites illustrated in Figure 7.2B, we can calculate the rates of open bite subjects in the sample that Worms analyzed (Table 7.3). Although this study has commonly been cited as reporting an 80% spontaneous correction of simple open bite from the 7–9 age range to the 10–12 age range, it is rarely reported that the data also seem to indicate a doubling of the rate of open bite in the next age range. The variability of the data, relatively small samples in each age range, and cross-sectional nature of this study are all reasons to view these data cautiously.
Table 7.3 Open bite classification by age category.
Data from: Worms, Meskin & Isaacson (1971).
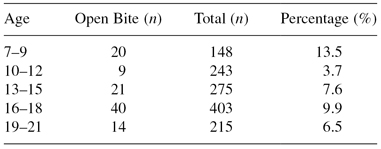
It is difficult to collect longitudinal data on spontaneous closure of open bite in the United States, as orthodontists almost always recommend treatment when it is recognized. However, there are two small samples of untreated open bite that have been reported in the literature. The first comes from a randomized trial of 146 mixed dentition patients in Washington state, half of whom received interceptive orthodontic treatment and half of whom received observation only. Of the 14 patients that had no incisor overlap and underwent 2 years of observation only, 6 (43%) displayed spontaneous correction after 2 years (Jolley et al. 2010). Another report from Brazil reported on 30 untreated open bite subjects, with a mean age slightly over 8 years (Pedrin et al. 2006). They reported that 4 (13%) exhibited spontaneous closure during the observation period, which lasted 1 year. The corresponding 30 subjects that underwent crib and chin cup therapy had an 80% closure rate in the same time period.
The data presented above seem to suggest a wide variation in the rate of spontaneous closure, and the evidence, at this time, is not conclusive. Data from the two large national surveys (cross-sectional) seem to indicate little change in open bite prevalence across age groups. Finally, data from two, small longitudinal studies seem to indicate that there may be some of spontaneous closure (13% to 40%) in the mixed dentition.
Treatment Options for Open Bite
Primary or Early Mixed Dentition
When open bites are discovered early, they are often accompanied by digit habits. Sometimes children may be very motivated to stop digit habits, and a candid discussion with their orthodontist may be sufficient to arrest the habit. Orthodontists may allow 3 to 6 months for children under 7 to attempt self-correction with simple therapies such as a mitten or glove worn at night, bitter compounds applied to the thumb, or thumb guards. If these are not sufficient, a thumb crib could be considered as a reminder. Although these are not particularly popular appliances to wear, acceptance is usually good if patients have already attempted simpler therapies without success. A common thought is that stopping a thumb or digit habit before the eruption of the permanent teeth usually results in spontaneous correction of the open bite and no long-term detrimental incisor relationships. However, every experienced orthodontist has probably seen a few patients stop their thumb habits early but still demonstrate persistence of an open bite as the permanent incisors erupt.
Late Mixed Dentition
By this time, most thumb and digit habits have stopped, and open bites persisting into this age group may be due to other factors, such as tongue posture or airway problems. Tongue posture is a commonly suspected etiologic factor, and late mixed dentition is usually a good time to recommend a tongue crib for correction of this problem. Two studies have suggested that tongue cribs lead to a high percentage of successful long-term closure of open bites (Justus 1976; Huang et al. 1990). A typical response to crib therapy is illustrated in Figure 7.3. Myofunctional therapy has been proposed as a means to modify aberrant tongue function and/or speech. However, the literature on the long-term success of myofunctional therapy is sparse (Mason 2008; Haruki, Kishi & Zimmerman 1999; Benkert 1997; Zimmerman 1989; Garliner & Gables 1982). Airway problems such as mouth breathing and enlarged tonsils have also been implicated in open bites, and tonsillectomy has been prescribed as a therapy. Extensive studies have been conducted on this issue, but no consistent etiologic relationships have been demonstrated (Linder-Aronson 1970; Mahony, Karsten & Linder-Aronson 2004; Bresolin et al. 1983; Sassouni et al. 1985; Soukiet et al. 2009; Fields et al. 1991; Vig KW. 1998). Other therapies that have been proposed in this developmental stage, including vertical elastics, posterior biteplates, magnets to intrude posterior teeth, chin cups to influence anterior vertical dimensions, spurs bonded to the incisors, jaw exercises, and low-seated transpalatal arches.
Figure 7.3 Nine months of crib use in a mixed dentition patient.
Permanent Dentition—Adolescent
In this developmental stage, conventional orthodontic treatment is commonly attempted for open bite patients. Correction of open bites using brackets and bands results primarily in dentoalveolar changes. For example, the multiloop edgewise (MEAW) technique closes open bites by dentoalveolar compensation (Kim et al. 2000). There is some support that extraction therapy may have a higher degree of long-term success compared to nonextraction therapy (Janson et al. 2006). The authors suggest that extraction therapy is more advantageous with respect to retracting incisors, thus encouraging deepening of the bite. During this time, growth modification is also possible, and many devices that target growth have been proposed, including high-pull headgear, chin cups, and functional appliances. The success of these devices long term is not well documented in the literature. In cases where the tongue is obviously in a forward position, tongue cribs may be prescribed. Again, if the etiologic agent can be identified prior to treatment and then addressed during treatment, the chance for success is probably increased.
Permanent Dentition—Adult
In nongrowing individuals with moderate to severe open bites, orthodontists may often consider surgery as the most appropriate and stable method to correct an open bite. The most common surgical procedure is LeFort I maxillary impaction with clockwise rotation, with concomitant mandibular surgery as needed for anteroposterior correction. Other types of surgery have been recommended, such as the Schuchart procedure (Ermel et al. 1999), which impacts the maxillary buccal segments, or bilateral sagittal split osteotomy with counterclockwise rotation (Bisase, Johnson & Stacey 2009). A surgical procedure that is rarely recommended is glossotomy. It may seem reasonable in patients who have unusually large tongues, and there are some reports of successful correction of open bite after glossotomy in the dental literature (Kawakami et al. 2005; Hotokezaka et al. 2001; Ball & Horrocks 1995; Ruff 1985). Some orthodontists may also consider conventional orthodontic treatment for mild open bites or for patients who may not be concerned about the lack of incisal contact. Some recent suggestions for treatment of open bite include temporary anchorage devices (Seres & Kocsis 2009; Sakai et al. 2008; Sherwood 2007; Kuroda et al. 2007; Kravitz & Kusnoto 2007; Xun, Zeng & Wang 2007; Kuroda, Katayama & Takano-Yamamoto 2004; Erverdi, Keles & Nanda 2004; Umemori et al. 1999), corticotomy (Akay et al. 2009), and occlusal equilibration (Janson et al. 2008).
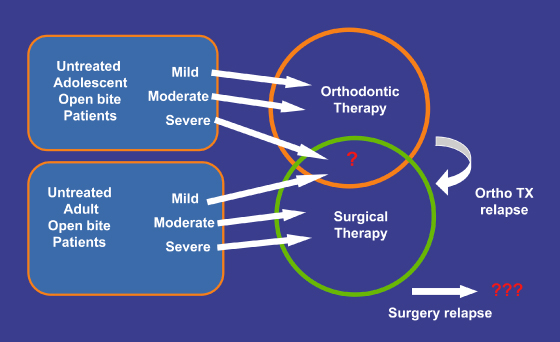
Impact of Severity and Growth Status
For many malocclusions, the severity of the problem, as well as the growth status of a patient, may influence an orthodontist’s choice of treatment. This is certainly the case for open bite patients. For example, consider open bites in growing subjects. In mild to moderate open bites, orthodontists would routinely attempt nonsurgical treatment, as they may be optimistic that habit and growth modification would allow correction of open bites that are not severe. Orthodontic treatment may also be recommended to correct severe open bites in adolescents to either eliminate orthognathic surgery or to reduce the severity of the vertical discrepancy. Thus, we might routinely observe orthodontists trying nonsurgical treatment for the majority of their adolescent patients, regardless of the severity of the problem.
On the other hand, orthodontists may take the opposite approach with adults, recommending surgery as the primary method of correction for moderate to severe open bites, citing a lack of growth as a reason to consider more aggressive techniques. Some orthodontists might even recommend that adults with mild open bites undergo surgery to maximize the chance for long-term stability. They may reason that adults have demonstrated a persistence of their vertical relationships and that more aggressive treatment will be needed to change and retain these new vertical relationships. The evidence for long-term stability of surgical versus nonsurgical therapy is covered in the next section of this chapter.
A deduction from this discussion, though, is that it becomes potentially difficult to compare success rates in adolescent and adult open bite patients due to the differing approaches that may be employed. Perhaps the areas of greatest overlap might be recommendations for adolescents with severe open bites, for which orthodontists might recommend surgical or nonsurgical treatment, and adults with mild open bites, which might be amenable to both surgical or nonsurgical treatment options (Figure 7.4). Ultimately, evidence about treatment and stability should allow us to decide how to best recommend treatment. Additionally, evidence to guide us on managing cases that relapse would be helpful for future patients.
Figure 7.4 Strategies for adolescents and adults.
Retention
For the typical orthodontic patient, alignment is the major factor to c/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


