7 Periodontics
OVERVIEW
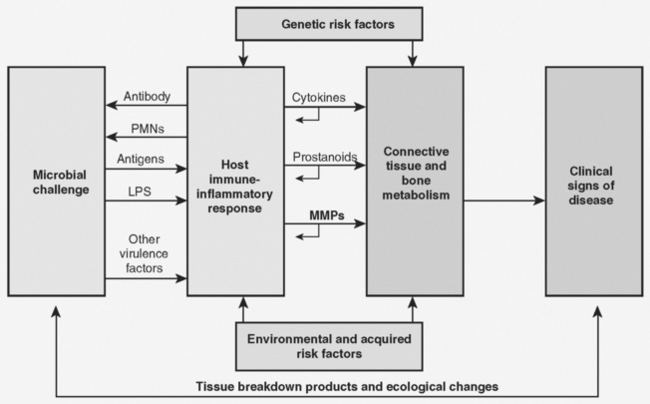
Periodontal disease describes a group of inflammatory conditions that affect the supporting structures of the teeth or periodontium. The initiation, development, diagnosis, and subsequent treatment of the disease follow a well-documented sequence (Fig. 7-1). Microbial plaque is generally considered to be the initiating factor in periodontal disease. When plaque accumulates on tooth and gingival surfaces, it instigates the development of an inflammatory response in the periodontal tissues. The nature and duration of the inflammatory response is critical to the clinical outcome. If the inflammatory response is sufficient to control the challenge from plaque without destruction of periodontal ligament or alveolar bone, the clinical condition is termed gingivitis. If there is destruction of periodontal ligament and alveolar bone, the condition is termed periodontitis. The fundamental diagnosis of gingivitis or periodontitis impacts treatment. With gingivitis, there is no destruction of the periodontium and therefore treatment should be focused on removing plaque and controlling inflammation. In periodontitis, the removal of plaque and control of inflammation may be supplemented with attempts to repair or regenerate the lost periodontal tissues and correct any anatomical deformities that may have resulted from the disease process.
1.0 DIAGNOSIS
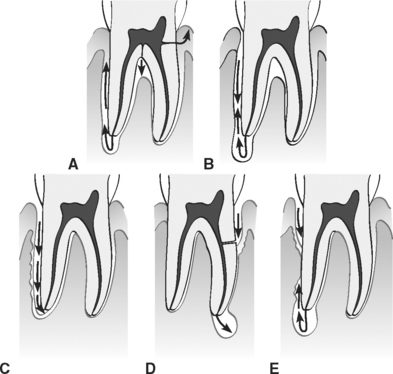
The complex anatomy of the furcation makes this a difficult area to treat and maintain.
Using the information described previously, the clinician can now diagnose one of the following conditions (Box 7-1):
Box 7-1 Classification of Periodontal Diseases and Conditions
Data from Armitage GC: Ann Periodontol 4:1, 1999. (From Newman MG, Takei HH, Klokkevold PR, Carranza FA: Carranza’s Clinical Periodontology, ed 10, St Louis, Elsevier, 2006.)
Developmental or Acquired Deformities and Conditions
Localized tooth-related factors that predispose to plaque-induced gingival diseases or periodontitis
Mucogingival deformities and conditions around teeth
Mucogingival deformities and conditions on edentulous ridges
* These diseases may occur on a periodontium with no attachment loss or on a periodontium with attachment loss that is stable and not progressing.
† Chronic periodontitis can be further classified based on extent and severity. As a general guide, extent can be characterized as localized (<30% of sites involved) or generalized (>30% of sites involved). Severity can be characterized based on the amount of clinical attachment loss (CAL) as follows: slight = 1 or 2 mm CAL; moderate = 3 or 4 mm CAL; and severe ≥ 5 mm CAL.
Periodontitis is defined as an inflammatory disease of the supporting tissues of the teeth caused by specific microorganisms or groups of specific microorganisms resulting in progressive destruction of the periodontal ligament and alveolar bone with pocket formation, recession or both. The clinical feature that distinguishes periodontitis from gingivitis is the presence of clinically detectable attachment loss. The most common forms of periodontitis and their distinguishing characteristics are listed in Box 7-2.
Box 7-2 Periodontitis
(From Newman MG, Takei HH, Klokkevold PR, Carranza FA: Carranza’s Clinical Periodontology, ed 10, St Louis, Elsevier, 2006.)
Chronic Periodontitis
The following characteristics are common to patients with chronic periodontitis:
Aggressive Periodontitis
The following characteristics are common to patients with aggressive periodontitis:
Localized form:
2.0 ETIOLOGY
Plaque formation can be divided into three phases:
3.0 PATHOGENESIS
The pathogenesis (genesis of pathological change; the cellular events and reactions and other pathological mechanisms occurring in the development of disease) of the periodontal diseases is the result of a complex interaction between plaque microorganisms and the host response to the presence of those microorganisms on tooth and gingival tissues. As outlined in Figure 7-1 of the Overview to this review, microbial plaque is considered to be the initiator of the disease process because it serves as a challenge to the host and host tissues (periodontal tissues). How the host responds to the plaque challenge determines the severity and extent of the tissue damage associated with that response.
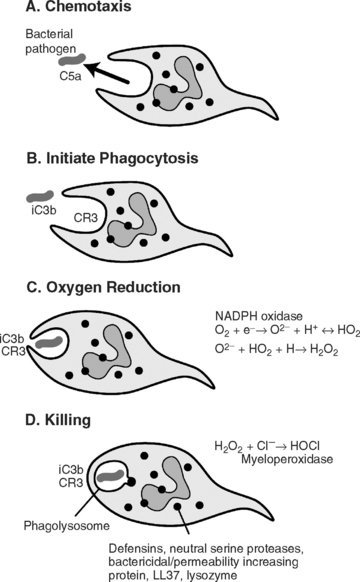
The extent and severity of the inflammatory response can be influenced by:
| CHEMOTAXIN | SOURCE |
|---|---|
| Tumor necrosis factor (TNF) | Macrophages/monocytes |
| Interleukin-8 (IL-8) | Neutrophils (PMNs), endothelium |
| Platelet-activating factor Leukotriene B4 | Many cells |
| C5a | Serum/plasma |
| Neutrophil chemotactic factor | Mast cells |
| Interleukin-1 (IL-1) | B cells, macrophages |
| Interferon-γ (IFN-γ) | Activated T cells |
| N-formyl-methionyl peptides | Bacteria |
PMNs, Polymorphonuclear leukocytes.
(From Newman MG, Takei HH, Klokkevold PR, Carranza FA: Carranza’s Clinical Periodontology, ed />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses