Chapter 7
Non-plaque-induced Periodontal Diseases II: Periodontal Lesions
Aim
The aim of this chapter is to raise the awareness of practitioners of the rare systemic diseases that may, as part of their clinical course, give rise to severe periodontal destruction. Fortunately, there are relatively few conditions that may present in this manner.
Outcome
It is anticipated that, having read this chapter, the practitioner will bear in mind the need to examine the primary, mixed and secondary dentitions for signs of periodontal destruction. In addition, the reader will be able to recognise the periodontal hallmarks of underlying systemic diseases and refer for specialist management with an appropriate degree of priority.
Introduction
The 1999 International Workshop Classification for Periodontal Diseases (see Chapple and Gilbert 2002) broadly classifies systemic diseases with periodontal manifestations as those of:
-
genetic origin
-
haematological origin
-
not otherwise specified.
In this chapter, “not otherwise specified” is not discussed but Connective tissue disorders are discussed (Table 7-1).
| Aetiology | Condition | Subcategory | GDP/ refer |
| Genetic disorders | Down syndrome | GDP-r | |
| type 1 diabetes | GDP-r | ||
| Papillon-Lefèvre syndrome | refer | ||
| Ehlers-Danlos syndrome | type IV | refer | |
| type VIII | refer | ||
| hypophosphatasia | perinatal | refer | |
| infantile | refer | ||
| childhood | refer | ||
| adult | refer | ||
| Cohen syndrome | refer | ||
| Job syndrome | refer | ||
| glycogen storage disease | refer | ||
| Haematological disorders | |||
| White blood cell disorders | Infantile genetic agranulocytosis | refer | |
| Leukocyte adhesion deficiency | refer | ||
| Lazy leukocyte syndrome | refer | ||
| Chédiak-Higashi syndrome | refer | ||
| agamma/hypogamma-globulinaemia | refer | ||
| Chronic granulomatous disease | refer | ||
| Histiocytosis-x | Hand-Schüller-Christian disease | refer | |
| Letterer-Siwe disease | refer | ||
| eosinophilic granuloma | refer | ||
| lymphocyte deficiencies – t-cell | DiGeorge syndrome | refer | |
| lymphocyte deficiencies – t- and b-cell | Wiskott-Aldrich syndrome | refer | |
| Red blood cell disorders | acatalasia | refer | |
| aplastic anaemia | refer | ||
| Connective tissue disorders | scleroderma | systemic sclerosis | refer |
| morphoea (localised) | refer |
GDP-r, manage in practice but refer if concerned or problems arise.
Refer, refer to periodontal specialist for advice and treatment.
Genetic Conditions with Periodontal Manifestations
Down Syndrome
Down syndrome is an inherited autosomal disorder that results from trisomy of chromosome 21. Approximately 50–90% of patients suffer from destructive periodontal disease, affecting both primary and secondary dentitions and an increased incidence of necrotising ulcerative gingivitis (NUG) has been reported. The lower incisors and upper molars are most commonly affected, and the propensity for shortened roots can result in early tooth loss. The underlying pathobiology is believed to involve neutrophil (polymorphonuclear leucocyte – PMNL) defects of chemotaxis, phagocytosis and killing, depressed T-cell-induced antigen killing and abnormal collagen biosynthesis. Care should be taken when planning periodontal therapy, since cardiac defects requiring antibiotic prophylaxis are very common in patients with Down syndrome.
Type 1 Diabetes
The incidence of Type I diabetes in Europe varies between 0.03% and 0.005%. However, data regarding the incidence of periodontitis in diabetic children and non-diabetic controls are conflicting. There appears to be an increased susceptibility to gingival inflammation in younger type 1 diabetics with poor glucose control in comparison to those with good control or non-diabetic subjects (see Chapter 3). However, the data for an increased risk of periodontitis are not as convincing.
Papillon-Lefèvre Syndrome
Papillon-Lefèvre syndrome (PLS) is an inherited autosomal dominant disorder, more common in consanguineous families. Thus, some Indian and Pakistani children may be affected more than Caucasians. The gene defect was recently mapped to the long arm of chromosome 11 (11q) and results in the loss of function of an important PMNL enzyme called cathepsin-C. Cathepsin-C is a lysosomal enzyme found in the primary granules of PMNLs that is important for bacterial destruction and is expressed in the skin of the feet and hands. PLS affects one to four patients per million and the classic signs are usually apparent by two to four years of age:
-
Palmar-plantar keratosis (Fig 7-1 and 7-2).
-
Rapidly progressive periodontal breakdown affecting both primary and secondary dentitions and leading to premature tooth loss (Figs 7-3 and 7-4).
-
Intracranial calcifications (sometimes reported).
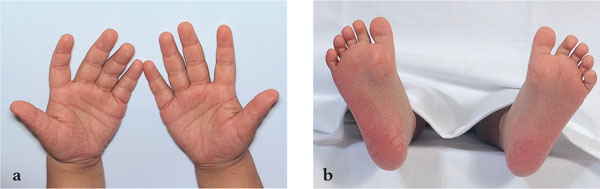
Fig 7-1 Keratosis affecting (a) the palms of the hands and (b) the soles of the feet of a two-year-old boy with Papillon Lefèvre syndrome. The gene mutation was a common mutation (R272P).

Fig 7-2 Keratosis affecting (a) the palms of the hands and (b) the soles of the feet of the father of the child in Fig 7-1.

Fig 7-3 Severe gingival inflammation in a seven-year-old boy with Papillon Lefèvre syndrome whose anterior teeth had grade II mobility.

Fig 7-4 Substantial bone loss affecting the permanent incisors of the patient in Fig 7-3.
The infant presents with severe gingival inflammation with or without recession and tooth mobility (Fig 7-3). Bone loss is severe and rapidly progressive, often leading to total deciduous tooth loss by four years of age. The inflammation resolves during the edentulous phase, consistent with a microbial aetiology, and returns with the eruption of the permanent dentition. Frequently, complete loss of the adult dentition results by early to mid-teens.
Diagnosis of PLS is largely based on clinical signs and symptoms and a thorough family history. Genetic diagnosis is now offered in specialist laboratories, and referral is recommended. Symptoms do appear to decrease with age, irrespect/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


