CHAPTER 7. Cysts of the jaws
TYPICAL FEATURES OF JAW CYSTS
Most jaw cysts behave similarly and usually grow slowly and expansively. They differ mainly in their relationship to a tooth and the radiographic features are usually a good guide as to their nature (Box 7.1). Even when it is not possible to decide the nature of a cyst, this affects treatment only with less common types. However, it is particularly important to distinguish odontogenic keratocysts and unicystic ameloblastomas from common types. These occasionally have identical radiographic appearances and diagnosis ultimately depends on histopathology.
Box 7.1
Key features of jaw cysts
• Form sharply-defined radiolucencies with smooth borders
• Fluid may be aspirated and thin-walled cysts may be transilluminated
• Grow slowly, displacing rather than resorbing teeth
• Symptomless unless infected and are frequently chance radiographic findings
• Rarely large enough to cause pathological fracture
• Form compressible and fluctuant swellings if extending into soft tissues
• Appear bluish when close to the mucosal surface
The classification of cysts is summarised in Box 7.2. There is not currently a complete classification of cysts that is accepted internationally.
Box 7.2
Classification of cysts of the jaws (WHO – modified)
Developmental cysts
• Odontogenic
‘Gingival cysts’ of infants (Epstein pearls)
Odontogenic keratocyst (‘primordial’ cyst)
Orthokeratinised odontogenic cyst
Dentigerous (follicular) cyst
Eruption cyst
Lateral periodontal cyst
Gingival cyst of adults
Glandular odontogenic; sialo-odontogenic cyst
• Non-odontogenic cysts
Nasopalatine duct cyst
Nasolabial cyst
Inflammatory odontogenic cysts
• Radicular
Residual
Lateral
• Paradental
OTHER CYSTIC OR CYST-LIKE LESIONS → Summary p. 157
Cystic odontogenic tumours are not included in the above classification, but cystic ameloblastomas and calcifying odontogenic (ghost cell) cysts can be mistaken radiographically for radicular or other non-neoplastic cysts as discussed later.
Also excluded from the above classification are cysts (in bone cavities) without epithelial lining (pseudocysts), namely solitary (simple) bone cysts and aneurysmal bone cysts. These also are cystic only in their radiographic appearances. They are skeletal diseases and affect the jaws only occasionally, as discussed in Chapter 9.
Odontogenic cysts (not surprisingly) affect the tooth-bearing region of the jaws. Most non-odontogenic, true cysts are developmental and form in the region of the anterior maxilla. Their relative frequency is shown in Box 7.3, though figures in the different surveys vary as a result of differences in categorisation, what kinds of cysts are included and other factors.
Box 7.3
Relative frequency of different types of jaw cysts
| Radicular | 65–70% |
| Dentigerous | 15–18% |
| Odontogenic keratocyst | 3–5% |
| Nasopalatine | 5–10% |
| Lateral periodontal | <1% |
| Paradental | <1% |
Radicular cysts are discussed first as, being the most common type, their treatment forms the basis for that of most other jaw cysts.
RADICULAR CYSTS → Summaries pp. 135, 190
Clinical features
Radicular cysts are the most common cause of major, chronic swellings and the most common type of cyst of the jaws. They are rarely seen before the age of 10 and are most frequent between the ages of 20 and 60 years. They are more common in males than females, roughly in the proportion of 3 to 2. The maxilla is affected more than three times as frequently as the mandible.
Radicular cysts, like other cysts of the jaws, cause slowly progressive painless swellings, with no symptoms until they become large enough to be conspicuous (Fig. 7.1). If infection enters, the swelling becomes painful and may rapidly expand, partly due to inflammatory oedema. The swelling is rounded and at first hard. Later, when the bone has been reduced to eggshell thickness, a crackling sensation may be felt on pressure. Finally, part of the wall is resorbed entirely away, leaving a soft fluctuant swelling, bluish in colour, beneath the mucous membrane. The dead tooth from which the cyst has originated is (by definition) present and its relationship to the cyst will be apparent in a radiograph (Fig. 7.2).
 |
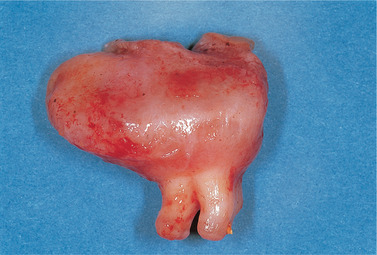
| Fig. 7.1
Typical clinical appearance of a large cyst. This radicular cyst in the right maxillary alveolar process forms a rounded swelling with a bluish colour.
|
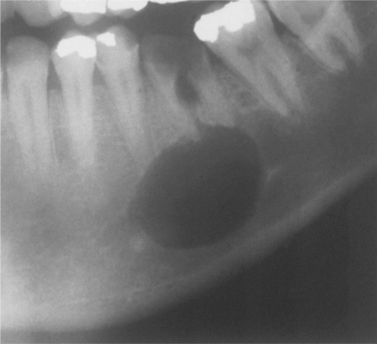 |
| Fig. 7.2
A radicular cyst on a grossly carious and non-vital first permanent molar. A rounded and sharply defined area of radiolucency is associated with the apices of the roots.
|
Pathogenesis and pathology
The main factors responsible for cyst development are summarised in Box 7.4.
Box 7.4
Major factors in the pathogenesis of cyst formation
• Proliferation of epithelial lining and fibrous capsule
• Hydrostatic pressure of cyst fluid
• Resorption of surrounding bone
Epithelial proliferation
Infection from the pulp chamber induces inflammation and proliferation of the epithelial rests of Malassez. If infection can be eliminated from the root canal, small radicular cysts (up to 1 or 2 cm diameter) may occasionally regress without surgery.
Hydrostatic effects of cyst fluids
That radicular and many other cysts expand in balloon-like fashion, wherever the local anatomy permits, indicates that internal pressure is a factor in their growth. The hydrostatic pressure within cysts is about 70 cm of water and therefore higher than the capillary blood pressure.
Cyst fluid is largely inflammatory exudate and contains high concentrations of proteins, some of high molecular weight which can exert osmotic pressure. Consistent with the inflammation usually present in cyst walls, cyst fluid may contain cholesterol, breakdown products of blood cells, exfoliated epithelial cells and fibrin.
Low-molecular-weight proteins are present in similar concentrations to those in the plasma, but there are smaller amounts of high-molecular-weight proteins. The capillaries in the cyst wall are more permeable as a result of inflammation and contribute varying amounts of immunoglobulins and other proteins. The net effect is that pressure is created by osmotic tension within the cyst cavity.
Bone-resorbing factors
Experimentally, cyst tissues in culture release bone-resorbing factors. These are predominantly prostaglandins E2 and E3. Different types of cysts and tumours may produce different quantities of prostaglandins but, if so, it is unclear whether this affects the mode of growth of the cyst. Collagenases are present in the walls of keratocysts, but their contribution to cyst growth is also unclear.
Pathology
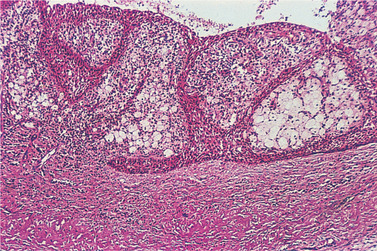
All stages can be seen from a periapical granuloma containing a few strands of proliferating epithelium derived from the epithelial rests of Malassez (Figs 7.3 and 7.4), to an enlarging cyst with a hyperplastic epithelial lining and dense inflammatory infiltrate. Epithelial proliferation results from irritant products leaking from an infected root canal to cause chronic periapical inflammation.
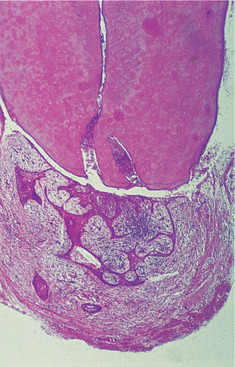 |
| Fig. 7.3
The earliest stages of formation of a radicular cyst. Some periapical granulomas, such as this, contain proliferating strands of odontogenic epithelium. In places the epithelium has broken down centrally to form small epithelium-lined spaces.
|
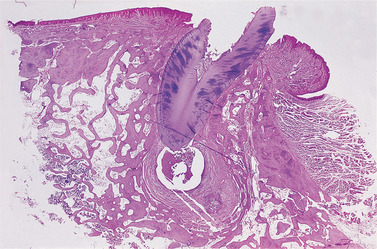 |
| Fig. 7.4
A developing radicular cyst. An epithelium-lined cavity has formed in this large periapical granuloma. There is a thick fibrous capsule infiltrated by chronic inflammatory cells. The alveolar bone has been resorbed and remodelled to accommodate the slowly expanding swelling.
|
Epithelial lining
The epithelial lining consists of stratified squamous epithelium of variable thickness. It lacks a well-defined basal cell layer and is sometimes incomplete. Early, active epithelial proliferation is associated with obvious chronic inflammation and may then be thick, irregular and hyperplastic or appear net-like (Fig. 7.5), forming rings and arcades (Fig. 7.6). Hyaline bodies may be seen in the epithelium (Fig. 7.7) and mucous cells may be present as a result of metaplasia (Fig. 7.8). Longstanding cysts typically have a thin flattened epithelial lining, a thick fibrous wall and minimal inflammatory infiltrate.
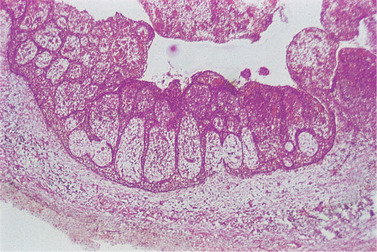 |
| Fig. 7.5
Radicular cyst. The epithelial lining often assumes this arcaded pattern with numerous inflammatory cells beneath its surface.
|
 |
| Fig. 7.6
Higher power of the lining of a radicular cyst. The arcaded epithelium contains numerous neutrophils emigrating into the lumen and there are pale-staining areas of foamy macrophages in the inner wall.
|
 |
| Fig. 7.7
Hyaline or Rushton bodies. These translucent or pink-staining lamellar bodies are formed by the cyst lining epithelium and indicate the odontogenic origin of a cyst.
|
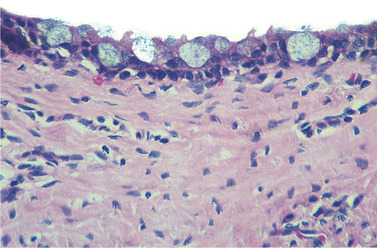 |
| Fig. 7.8
Mucous metaplasia in a radicular cyst. The numerous goblet cells can be seen but are more typical of dentigerous cysts.
|
The cyst capsule and wall
The capsule consists of collagenous fibrous connective tissue. During active growth the capsule is vascular and infiltrated by chronic inflammatory cells adjacent to the proliferating epithelium. Plasma cells are often prominent or predominant and are a response to antigens leaking through the tooth apex.
In the bony wall, there is osteoclastic activity and resorption. Beyond the zone of resorption there is usually active bone formation. The net effect is that a cyst expands but retains a bony wall, even after it has extended beyond the normal bony contours. This bony wall, nevertheless, becomes progressively thinner since repair is slower than resorption, until it forms a mere eggshell, then ultimately disappears altogether. The cyst then starts to distend the soft tissues and appears as a soft bluish swelling (see Fig. 7.1).
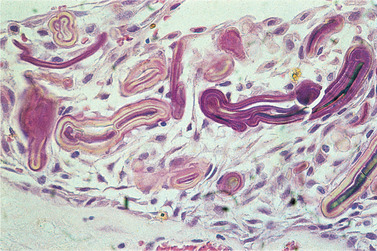
Clefts
Within the cyst capsule there are often areas split up by fine needle-shaped clefts (Figs 7.9 and 7.10). These are left by cholesterol dissolved out during preparation for sectioning. The cholesterol is derived from breakdown of blood cells. Small clefts are enclosed by foreign body giant cells and extravasated red cells and blood pigment are associated. Clefts may also be seen extending into the cyst contents but are formed in the cyst wall.
 |
| Fig. 7.9
Cholesterol clefts in a cyst wall. This low-power view shows the relationship of cholesterol clefts to the cyst. Cholesterol crystals are formed in the fibrous wall. The epithelium overlying this focus has broken down and the cholesterol has leaked into the cyst contents. Elsewhere the lumen is lined by a flattened layer of squamous epithelium.
|
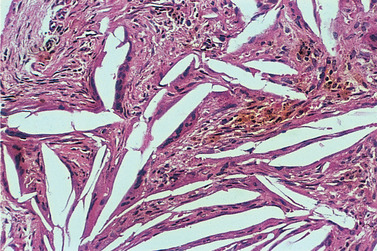 |
| Fig. 7.10
Cholesterol clefts. Cholesterol has been dissolved out during preparation of the section, leaving clefts. The crystals are treated as foreign bodies and flattened multinucleate foreign body giant cells are seen along the edges of several clefts.
|
Cyst fluid
The fluid is usually watery and opalescent but sometimes more viscid and yellowish, and sometimes shimmers with cholesterol crystals. A smear of this fluid may show typical notched cholesterol crystals microscopically (Fig. 7.11). Histologically, the protein content of the fluid is usually seen as amorphous eosinophilic material, often containing broken-down leucocytes and cells distended with fat globules.
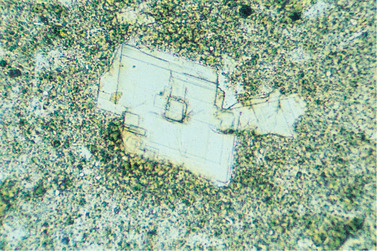 |
| Fig. 7.11
Cholesterol crystals from a cyst aspirate indicating the presence of inflammation. The rectangular shape with a notched corner is characteristic.
|
Radiography
A radicular cyst appears as a rounded, radiolucent area with a sharply defined outline. A condensed radiopaque periphery is present only if growth is unusually slow and is usually more prominent in longstanding cysts. The dead tooth from which the cyst has arisen can be seen and often has a large carious cavity. Adjacent teeth may be tilted or displaced a little or occasionally become slightly mobile. Very large cysts in the maxilla may extend in any available direction and become irregular. Infection of a cyst causes the outline to become hazy as a result of greater vascularity and resorption of the surrounding bone.
Key features of radicular cysts are summarised in Box 7.5.
Box 7.5
Radicular cyst: key features
• Form in bone in relation to the root of a non-vital tooth
• Arise by epithelial proliferation in an apical granuloma
• Are usually asymptomatic unless infected
• Diagnosis is by the combination of radiographic appearances, a non-vital tooth and appropriate histological appearances
• Clinical and radiographic features are usually adequate for planning treatment
• Do not recur after competent enucleation
• Residual cysts can remain after the causative tooth has been extracted and diagnosis is then less obvious
• Cholesterol crystals often seen in the cyst fluid but not specific to radicular cysts
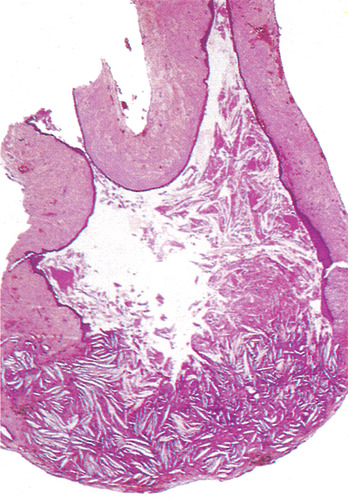
Residual and lateral radicular cysts → Summaries pp. 135, 190
A radicular cyst may persist after extraction of the causative tooth. Residual cysts are a common cause of swelling of the edentulous jaw in older persons (Figs 7.12 and 7.13). Residual cysts may interfere with the fit of dentures, but may slowly regress spontaneously. This is suggested by the progressive thinning of the lining (Fig. 7.14).
 |
| Fig. 7.12
Residual cyst. The causative tooth has been extracted leaving the cyst in situ. See also Figure 7.13.
|
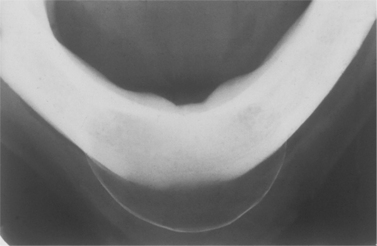 |
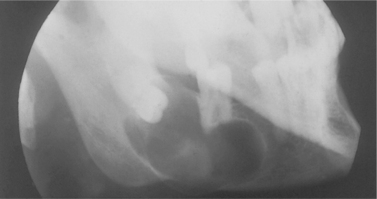
| Fig. 7.13
Radiographic appearance of the residual cyst shown inFigure 7.12. Note the thin bulging periosteal new bone layer which can give rise to the clinical sign of eggshell crackling. (Figures 7.12 and 7.13 kindly lent by Mr P Robinson.)
|
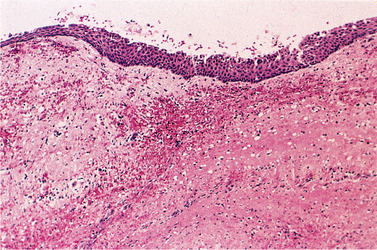 |
| Fig. 7.14
Lining of a residual cyst. There is only a minor degree of inflammation and the epithelium forms a thin regular layer.
|
Lateral radicular cysts can occasionally form at the side of a non-vital tooth as a result of the opening of a lateral branch of the root canal. They are rare and must be distinguished from lateral periodontal cysts which are another entity as discussed earlier.
Differential diagnosis
There are many causes of circumscribed areas of radiolucency in the jaws (Box 7.6).
Box 7.6
Differential diagnosis of cyst-like areas of radiolucency
Radicular cysts are usually readily recognised by their clinical and radiographic features. The cystic nature of a lesion can be confirmed by aspirating its contents through a needle inserted through the wall under aseptic conditions. The detection of fluid does not distinguish one cyst from another or a cystic neoplasm from a true cyst. The presence of cholesterol crystals is not of diagnostic significance.
Histologically, the lining of simple stratified squamous epithelium with an inflammatory infiltrate confirms the diagnosis. Distinguishing features of other types of cysts are discussed below.
Neoplasms
Benign (odontogenic) tumours or, occasionally, an ameloblastoma may resemble a simple cyst radiographically. Resorption of adjacent teeth suggests a neoplasm rather than a cyst but is not diagnostic in itself. It is essential that the whole of a cyst lining be available for examination, since part of the lining, even though neoplastic, may appear as a thin layer of flattened stratified squamous epithelium like that of a simple cyst.
Rarely, a metastasis in the jaw may cause a sharply defined area of radiolucency. More often it causes a lesion with a hazy outline and irregular shape. Tumours also tend to be painful and to grow more rapidly than cysts. Nevertheless, it may be difficult or impossible to distinguish them from infected cysts radiographically, but at operation the solid nature of a tumour will be obvious and histological examination will confirm the diagnosis.
Treatment
Enucleation and primary closure
Enucleation is the usual method and usually entirely effective (Box 7.7). The affected (dead) tooth may be extracted or root-filled and preserved. A mucoperiosteal flap over the cyst is raised and a window is opened in the bone large enough to give adequate access. The cyst is then carefully separated from its bony wall. The entire cyst is removed intact and should be sent in fixative for histological examination. The edges of the bone cavity are smoothed off, free bleeding is controlled and the cavity is irrigated to remove debris. The mucoperiosteal flap is replaced and sutured in place. The sutures should be left for at least 10 days.
Box 7.7
Advantages and limitations of enucleation of cysts
Advantages
• The cavity usually heals without complications
• Little aftercare is necessary
• The complete lining is available for histological examination
Possible disadvantages
• Infection of the clot filling the cavity
• Recurrence due to incomplete removal of the lining
• Serious haemorrhage (primary or secondary)
• Damage to apices of vital teeth projecting into the cyst cavity
• Damage to the inferior dental nerve
• Opening the antrum when enucleating a large maxillary cyst
• Fracture of the jaw if an exceptionally large mandibular cyst is enucleated
Any disadvantages are largely theoretical and in competent hands even very large cysts can be enucleated safely. Recurrence is remarkably rare. There are few contraindications: they are relative rather than absolute.
Marsupialisation
Marsupialisation is a largely outmoded treatment for radicular cysts. The cyst is opened essentially as for enucleation, but the lining is sutured to the mucous membrane at the margins of the opening. The aim is to produce a self-cleansing cavity which becomes, in effect, an invagination of the oral tissues. However, considerable aftercare is needed to keep the cavity clean. The cavity is initially packed with ribbon gauze and, after the margins have healed, a plug or extension to a denture is made to close the opening. Food debris has to be regularly washed out but, once the cavity has filled up from the base and sides sufficiently to become self-cleansing, the plug can be removed. The cavity usually becomes closed by regrowth of the surrounding tissue and restoration of the normal contour of the part. However, the orifice may close and the cyst re-form. Also, the complete lining is not available for histological examination.
The main application of marsupialisation is for temporary decompression of exceptionally large cysts where fracture of the jaw is a risk. When enough new bone has formed, the remaining cyst can be enucleated. Occasionally, retention of the tooth in a dentigerous cyst is needed and marsupialisation may allow it to erupt.
PARADENTAL CYSTS
Paradental cysts occasionally result from inflammation round partially erupted teeth, particularly mandibular third molars. They affect males predominantly, usually between the ages of 20 and 25 years. The affected tooth is vital but typically shows pericoronitis. Histologically, the cyst resembles a radicular cyst but for a more intense inflammatory infiltrate in the wall.
Enucleation is effective.
DENTIGEROUS CYSTS
A dentigerous cyst surrounds the crown of a tooth and is a dilatation of the follicle (Figs 7.15 and 7.16). The cyst is attached to the neck of the tooth, prevents its eruption and may displace it for a considerable distance.
 |
| Fig. 7.15
Dentigerous cyst. This cyst has been removed together with its associated tooth. The cyst surrounds the crown and is attached at the cementoenamel junction.
|
 |
| Fig. 7.16
Dentigerous cyst. The cyst has developed around the crown of the buried third molar (left), but has extended forward to involve the root of a vital second molar. It should not, however, be confused with a radicular cyst arising from the latter.
|
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


