6
The Art and Science of Biopsy and Cytology
In Chapter 1, in addition to head and neck soft tissue examination techniques, there is information about overall screening and diagnosis adjunct options as well detailed information about some diagnostic adjunctive procedures such as chemiluminescent reflectance and narrowband autofluorescence. This chapter provides detailed information about oral mucosal cytology and biopsy indications. The surgical biopsy remains the current gold standard of tissue diagnosis.
Oral Mucosal Cytology Indications and Contraindications
Oral mucosal cytology is a screening procedure unique and different from uterine cervical cytology screening (i.e., traditional Pap smear or liquid cytology Pap smear with or without HPV testing). The uterine cervix and oral/oropharyngeal mucosa are composed of similar stratified squamous epithelial cells; however, the biologic nature and behavior of the cells differ because of a substantially different physiological milieu. This is an important point to keep in mind, particularly with indication criteria, microscopic interpretation, and future management considerations.
Studies in the 1960s and 1970s confirmed routine Pap smears of the oral cavity had too many false positives and negatives. We acknowledge the improved sampling of oral cavity epithelial cells with the late 1990s Oral CDx brush biopsy cytobrush (described in Chapter 1) and some investigators reported improved specificity, sensitivity, and positive predictive value compared with conventional cytology. In addition, after reading encouraging results of liquid-based cytology results from uterine cervix studies, one of us (MAK) concluded that methodology could be useful for oral cytology specimens. Currently, the cytology method we support combines the advantages of a nylon-bristle cell collection device with liquid fixative for chairside cell transfer and immersion, transport, and slide preparation.
The following oral cytology indications and contraindications are based on our use of a liquid-based cytology process. It is important to remember the indications for cytology screening of the oral and oropharyngeal mucosa are very limited. Unlike the original Oral CDx brush biopsy’s indication of “nonsuspicious” oral “red or white spots” we recommend the indication should be for lesions suspicious for squamous cell carcinoma (e.g., unexplained nonhealing ulcer, erythroplakia, or speckled leukoplakia), especially when occurring in high-risk oral mucosal sites and the patient refuses or is unable to undergo a surgical biopsy. It should be emphasized that we consider the brush biopsy a form of cytology since architectural intact tissue from the surface and underlying connective tissue is not obtained. Additionally, leukoplakias should be investigated in a similar manner; however, it is more difficult to harvest deeper level keratinocytes due to the variable thickened keratin layer. In addition, indications include two infectious diseases: herpes simplex and candidiasis. Candidiasis can be diagnosed by cytology because the surface epithelial cells are associated with superficially embedded spores and/or hyphae of Candida albicans. Herpes simplex infection (primary or recurrent) can be diagnosed with cytology by sampling an intact vesicle or the peripheral area of a ruptured one (i.e., erosion or ulceration), which possesses infected keratinocytes. Epithelial cells infected with Herpesviridae exhibit microscopic pathognomonic morphological changes that, when combined with the viral infection’s clinical signs and symptoms, can result in an accurate diagnosis.
Leukoplakias and erythroplakias can have variable amounts of epithelial dysplasia involving the thickness of the surface epithelium or just benign cellular atypia secondary to mucosal inflammation within the epithelium (i.e., inflammatory exocytosis). It is imperative for the clinician to understand that the histological interpretation of an oral cytology sample of a leukoplakia or erythroplakia is limited to stating whether abnormal cellular changes are present or not. Thus, the cytology procedure does not confirm the presence or absence of epithelial dysplasia; dysplasia is a subjective microscopic diagnosis that requires architecturally intact stratified squamous epithelium (i.e., surgical biopsy) so that the width of dysplasia within the epithelium can be determined. In a cytology procedure, conventional or liquid technique, the epithelial cells are disaggregated as individual cells and/or small clumps of cells; therefore, a pattern of disruption of the normal epithelial maturation process (i.e., dysplasia) cannot be appreciated. Any positive atypical cellular finding that is not due to herpes infection or candidiasis must undergo a diagnostic biopsy procedure.
It is also critical for the clinician to understand that cytology procedures are only able to examine epithelial cells and thus any pathology that exists within the lamina propria (i.e., the connective tissue and its elements below the epithelium’s basement membrane) cannot be evaluated. The brush simply does not sample deeply enough to gather the pathological cells and/or substances. Examples of cytology sampling contraindications include amalgam tattoo, fibroma, mucocele, neuroma, and minor salivary gland tumors. Also, other specific epithelial proliferations such as squamous papilloma and verruca vulgaris cannot be diagnosed via cytology because they require the overall intact histological pattern and features only provided by surgical biopsy.
Cytology Technique Tips and Pitfalls
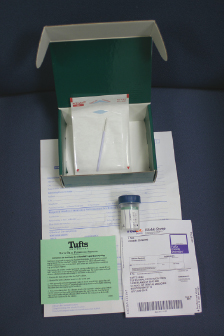
A suitable liquid cytology kit can be obtained from several oral pathology laboratories in the United States (Fig. 6.1). The free kit will typically be enclosed in a corrugated box or shipping tube that includes a specimen bottle filled with 10 mL of alcohol-based fixative (e.g., ThinPrep® or SurePath® brands), cytobrush (e.g., Medscand’s Cytobrush Plus®), requisition form, small plastic bag, and a prepaid overnight mailer and outer shipping bag. The requisition form is filled out completely with patient, doctor, and lesion information (details of the latter are discussed in the biopsy section, “Scalpel Biopsy Dos and Don’ts”).
It is very important to obtain an adequate harvest of keratinocytes from all levels of the oral mucosa’s stratified squamous epithelium. Whether the cytobrush selected has soft or firm bristles, the clinician must apply enough downward and back-and-forth force to obtain a transepithelial specimen. Once the harvested area demonstrates pinpoint bleeding, then the clinician has clinical verification of adequate depth since the vasculature resides only within the lamina propria below the basement membrane zone. As soon as the cells have been harvested it is crucial that they are immediately immersed in the liquid fixative container so that the cell sample does not air dry and destroy cellular detail. With the bristles of the brush immersed, the handle/shaft of the brush should be vigorously twirled with the fingers to agitate harvested cells off the bristles and into the liquid fixative. To retain as many harvested cells as possible for processing and analysis, the handle/shaft is cut off and the brush’s bristles are left within the specimen container for use during specimen processing. The cap of the fixative container is secured and the container is placed in the provided small plastic bag. The plastic bag is placed in the corrugated box or tube, and lastly the box or tube is placed in the overnight delivery service shipping bag with the prepaid mailing label affixed on its surface.
Biopsy Indication and Contraindications
Biopsy of oral and oropharyngeal tissues is the gold standard for diagnosis and is defined as the removal for diagnostic study of a piece of tissue from a living body. It has been used for more than 150 years to establish the diagnosis of an unknown medical condition and is the oldest and most reliable method currently available that can establ/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


