4
Differential Diagnosis of Common Oral Soft Tissue Lesions
Following the initial comprehensive head and neck soft tissue examination (Chapter 1), the clinician can identify the lesion as arising in the soft tissue and provide its detailed description (Chapter 2), determine its appropriate category (e.g., white lesion that rubs off, red lesion, ulceration) as listed in Chapter 3, and then create a nonprioritized list of all possible soft tissue lesions that may produce a similar clinical picture. The next step is to create a prioritized differential diagnosis list; the list should be rearranged with the most probable lesion ranked at the top and the least likely at the bottom. The process of priority ranking can be complicated at times so it behooves the clinician to be familiar with the signs and symptoms produced by a great many diseases and to possess statistical knowledge relative to the incidence of each disease entity. The priority ranking is directly related to the relative incidence of the lesions if all other factors about the lesions are similar. Thus, in developing a clinical differential diagnosis the clinician first ranks the lesions in order of their relative frequency of occurrence and then modifies this order based on age, gender, race, and anatomic location.
A special case can exist in which two or more lesions are synchronously present. If so, then seven possibilities must be considered:
- Lesions A and B are completely unrelated:
- Lesions A and B are both present as a matter of chance.
- Lesions A and B are related and
- Lesion A and Lesion B are identical.
- Lesion B is secondary to Lesion A.
- Lesion A is secondary to Lesion B.
- Lesion A and Lesion B are both secondary to a third lesion, which may be occult.
- Lesion A and Lesion B are manifestations of systemic disease.
- Lesion A and Lesion B form part of a syndrome.
Once a prioritized ranking differential diagnosis list has been created the clinician should recheck its credibility, particularly the top choices. This entails further examination of the lesion, asking the patient additional questions, possibly ordering additional tests, and a final reevaluation of all gathered pertinent data. The top choice or choices are referred to as the working or provisional diagnosis; in some instances, the first choice is overwhelmingly favored and becomes the singular working diagnosis. The working diagnosis dictates the proper management of the lesion, including possible surgery. The final diagnosis is usually provided by the pathologist who evaluates the biopsied tissue microscopically. In some instances the microscopic appearance of the lesion is not diagnostic in its own right and must be correlated closely with the previously submitted or gathered information. At times, an equivocal diagnosis remains and the clinical findings during surgery must also be considered.
Diagnostic Tips and Pitfalls
Acute Ulcers, Erosions, and Vesicles (Fig. 4.1)
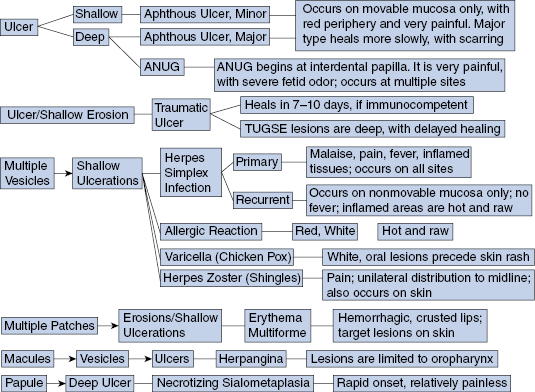
- Traumatic ulcer
- Tip—should heal in 7–10 days if the patient is immunocompetent; extremely common occurrence.
- Pitfall—traumatic ulcerative granuloma with stromal eosinophilia (TUGSE) is a very deep, slow-healing traumatic ulcer that can take weeks to months to heal. Also, factitial ulcers (self-inflicted) may be repeatedly traumatized despite the patient’s denial.
- Recurrent aphthous ulcer, minor type
- Tip—occurs only on movable mucosa.
- Pitfall—may appear identical to herpes simplex infection once the latter’s vesicle is ruptured. Many systemic conditions also have oral aphthouslike ulcerations.
- Recurrent aphthous ulcer, major type
- Tip—occurs only on movable mucosa.
- Pitfall—is not preceded by vesicle such as herpes simplex infection.
- Primary herpes simplex infection
- Tip—occurs anywhere in the mouth, on both movable and nonmovable mucosa (bound to bone, i.e., hard palate and attached gingiva). In addition to painful ulcers the patient will also have fever, malaise, lymphadenopathy, and stomatitis, which always includes the gingiva.
- Pitfall—often misdiagnosed as acute necrotizing ulcerative gingivitis (ANUG) prior to the onset and recognition of vesicles.
- Recurrent herpes simplex infection
- Tip—a crop of ulcers that occurs only on nonmovable mucosa (bound to bone; i.e., hard palate and attached gingiva); no other symptoms besides painful ulcers preceded by vesicles.
- Pitfall—mistaken for aphthous ulcer but preceded by a vesicle. Unlike aphthous ulcers, herpes simplex ulcers do not occur on movable mucosa.
- Acute necrotizing ulcerative gingivitis (ANUG)
- Tip—not a communicable disease. Debridement results in rapid resolution.
- Pitfall—can become extensive and spread to oral mucosa not associated with the teeth (i.e., acute necrotizing ulcerative mucositis, or ANUM).
- Allergic reaction
- Tip—cannot be wiped off.
- Pitfall—mistaken for leukoplakia, erythroplakia, and lichen planus.
- Erythema multiforme
- Tip—acute, rapid, or explosive onset; lips with hemorrhagic crusts; can have “target” (bull’s-eye appearing) skin lesions.
- Pitfall—not contagious; can become extensive; can be triggered by a drug reaction.
- Herpangina
- Tip—vesicles and subsequent not very painful ulcers are limited to the oropharynx including soft palate; often seen as an epidemic event in children.
- Pitfall—morphology mimics recurrent herpes but there is limited involvement: only occurs on posterior movable mucosa.
- Tip—vesicles and subsequent not very painful ulcers are limited to the oropharynx including soft palate; often seen as an epidemic event in children.
- Varicella (chicken pox)
- Tip—white enanthem precedes cutaneous exanthem (rash); painful and unilateral.
- Pitfall—prevalence increases with age; single occurrence (unlike herpes simplex).
- Herpes zoster (shingles)
- Tip—striking unilateral distribution up to midline of both face and oral mucosa (when involved).
- Pitfall—at times can appear identical to recurrent herpes simplex infection of the oral mucosa.
- Necrotizing sialometaplasia
- Tip—acute onset unlike malignancy, despite nonpainful deep ulceration (pain subsides when necrotic tissue sloughs out, leaving deep ulcer) with no overt history of trauma; usually occurs on the hard palate.
- Pitfall—mistaken for squamous cell carcinoma (clinically and histologically), which has chronic onset. Squamous cell carcinoma is rare on hard palatal mucosa.
Chronic Vesicles, Bullae, Erosions, and Ulcers (Fig. 4.2)
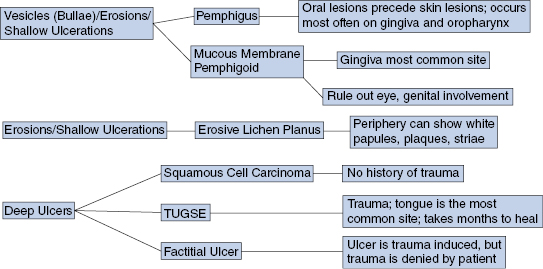
- Erosive lichen planus
- Tip—adjacent areas may exhibit white papules and striae; rare in children.
- Pitfall—desquamative gingivitis, allergic reaction.
- Squamous cell carcinoma
- Tip—no history of trauma; nonhealing lesion with indurated margins particularly in high-risk anatomical sites; often preceded by erythroplakia, to a lesser degree leukoplakia, and/or combination thereof; most often occurs on lateral tongue and floor of mouth.
- Pitfall—biopsy required for diagnosis if no improvement without assumption that it is a chronic infection; early metastasis.
- Mucous membrane pemphigoid
- Tip—rule out ocular or genital involvement; gingiva is most common site; antibody deposition at basement membrane zone.
- Pitfall—ocular involvement can lead to scarring and eventual blindness.
- Pemphigus vulgaris
- Tip—oral lesions (particularly in the posterior area) usually precede skin involvement; blood crusted lips; antibody to desmosomes.
- Pitfall—clinical similarity to erythema multiforme (EM) but does not have acute onset like EM.
- Traumatic ulcerative granuloma with stroma eosinophilia (TUGSE; traumatic granuloma; eosinophilic ulcer)
- Tip—lateral tongue most common site. Biopsy/surgery may trigger resolution.
- Pitfall—may mimic deep fungal infections and squamous cell carcinoma, so biopsy should be performed for diagnosis. TUGSE can occur on other oral mucosal sites besides the tongue.
- Factitial ulcer (self-induced)
- Tip—lacks induration and ragged outline. Trauma is denied by patient but presence of ulcer is unexplained.
- Pitfall—biopsy without further delay if ulcer persists after 2 weeks, to rule out malignancy.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


