Chapter 6
Sealers, Lining and Base Materials
Aim
The recommended use of sealers, lining and base materials has radically changed in recent times. The aim of this chapter is to give increased appreciation of the relationship between leakage around restorative materials and the maintenance of pulp vitality.
Outcome
Readers will be aware of techniques to protect pulp vitality, including the placement of direct and indirect pulp caps. The flow diagrams will aid clinicians in their choice of a restorative regime.
Protecting the Vitality of the Dental Pulp
The primary aim of managing caries and other damage to teeth should be preservation of pulp vitality. This is often best achieved by minimising pulpal inflammation. Even relatively superficial damage can lead to pulpal inflammation and symptoms of hypersensitivity (Brannstrom and Lind, 1965), Fig 6-1a. Where this has occurred and restorative intervention is required, the second aim of management is to minimise further pulpal inflammation by atraumatic minimal intervention. The action of cutting a diseased or damaged tooth further traumatises the pulp by application of mechanical and thermal stresses (Fig 6-1b). Important factors include drill speed, type of bur, pressure applied, time in contact with dentine and the use of water coolant.
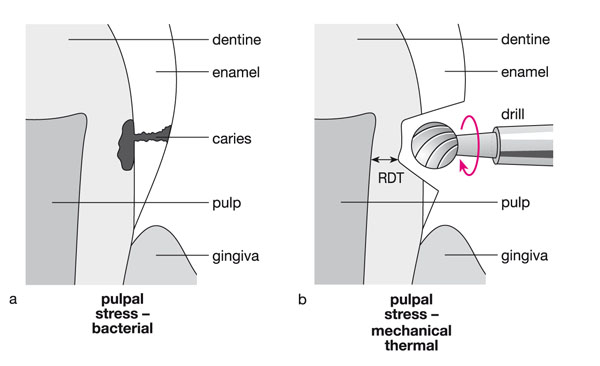
Fig 6-1 (a) The presence of a carious lesion may cause bacterial inflammation of the pulp. (b) Additional pulpal inflammation is caused by the action of cutting the tooth, which further traumatises the pulp by application of mechanical and thermal stresses: RDT = remaining dentine thickness.
The third aim of management is to choose restorative materials and procedures that do not irritate the pulp through the release of chemicals capable of passing through the dentine and causing adverse reactions in the pulp (Fig 6-2a). The final aim of management is to avoid late-onset pulpal inflammation, caused by bacterial ingress between the restoration and the cavity wall, in the absence of marginal seal (Fig 6-2b).
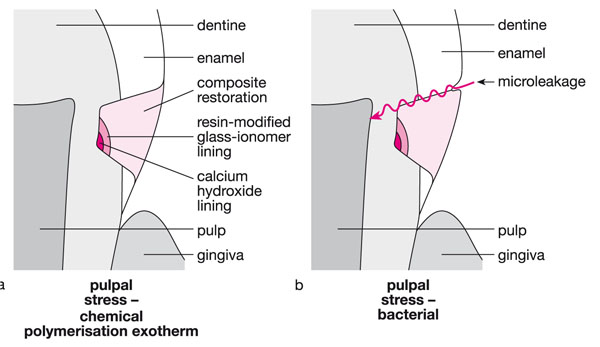
Fig 6-2 (a) Further pulpal inflammation may occur if lining and restorative materials are chosen that irritate the pulp by release of chemicals capable of passing through the dentine to the pulp. (b) Late-onset pulpal inflammation may take place if bacterial microleakage between the restoration and the cavity wall occurs.
Lining and base materials have important roles in preventing pulpal inflammation. The purposes of lining and base materials may include:
-
Acting as a bacteriostatic agent against any bacteria present in carious dentine.
-
Being biologically active and stimulating odontoblasts lining the pulp chamber to lay down tertiary dentine.
-
Protecting the pulp by preventing diffusion of chemicals from the restorative material through dentine.
-
Reducing leakage between the restoration and dentine.
-
Isolating the pulp from intraoral thermal stimuli.
-
Limiting fluid movement through dentine, which may give rise to symptoms of discomfort and pain.
-
Providing rigid support for the overlying restorative material, in particular under loading.
-
Blocking out undercuts if an indirect restorative technique is to be used.
Dentine is very effective at protecting the pulp from damage as it is a good insulator and reduces diffusion of chemicals from the cavity floor to the pulp (Stanley et al., 1975). An important factor in determining whether cavity preparation will cause pulpal change, by initiating secretion of a tertiary dentine matrix, is the remaining dentine thickness – the thickness of dentine between the floor of the cavity and the pulp. The preparation of shallow cavities, with 0.5–3.0 mm of remaining dentine thickness causes little irritation of the pulp, and therefore there is little stimulation of the odontoblasts to secrete reactionary dentine. The preparation of deep cavities, with 0.25–0.5 mm of remaining dentine thickness, causes a small reduction in numbers of odontoblasts following the injury, but maximally stimulates the surviving odontoblasts to lay down a thick layer of tertiary dentine. The preparation of very deep cavities, with 0.01–0.25 mm of remaining dentine thickness, causes greater trauma and a large reduction in odontoblast numbers. As a consequence, there are relatively few odontoblasts left to secrete tertiary dentine when it is most needed (Murray et al., 2002a).
Influence of Restorative Materials
Previously, it was thought that inflammation of the pulp was directly caused by toxins from restorative materials passing through the remaining dentine to the pulp. Now, it is thought that the effects of these chemicals are mild and short-lived, with pulpal irritation being caused by later-onset inflammation, induced by bacterial leakage (Watts and Paterson, 1987).
Under experimental conditions, when bacteria are excluded, most restorative materials cause little pulpal inflammation. In clinical service, however, it is almost impossible to prevent bacterial contamination of the tooth–restoration interface, with possible pulpal consequences. This leakage is often referred to in the literature as microleakage – the passage of bacteria, fluids, molecules or ions along the interface of a dental restoration and the wall of the cavity preparation. The ability to create a durable marginal seal and reduce microleakage varies according to the restorative material and the operative techniques employed.
Leakage
Restorative materials, including liners and bases, can protect the pulp by sealing the tooth from leakage or by their inherent bacteriostatic properties (or both).
-
Glass-ionomer cements are good at limiting leakage as they bond chemically to both enamel and dentine. In addition, glass-ionomer cements are bacteriostatic, given their ability to release fluoride and other elements, notably zinc. There i/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


