6
Prediction planning
- Be aware of the current methods of prediction planning.
- Understand and be able to apply the two-dimensional planning process in routine clinical practice.
- Be aware of the advantages and disadvantages of two-dimensional planning.
- Understand the steps in producing a three-dimensional ‘virtual patient’.
- Have knowledge of navigation surgery and its potential future role in orthognathic surgery.
6.1 Introduction
The aim of this chapter is to introduce the different methods of orthognathic prediction planning, highlighting current practice to state of the art three-dimensional planning. The strength and short comings of each method of planning will be discussed. This chapter will describe in detail the methods of planning that are currently used by the Team; both two dimensional prediction software (CASSOS – Computer Assisted Surgical Simulation for Orthognathic Planning) and three dimensional prediction software (Maxilim)*. The majority of computer planning programs apply a similar methodology which will help the reader transfer knowledge and techniques learned in this chapter into their own clinical practice.
6.2 Prediction planning for orthognathic surgery
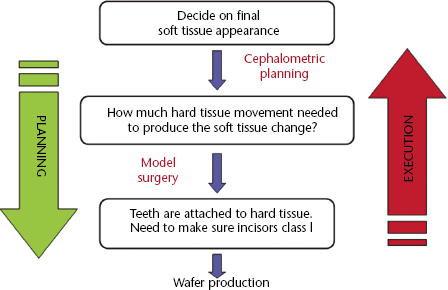
The successful outcome of orthognathic surgery requires precise surgical technique and comprehensive orthodontic treatment. More importantly the final outcome must provide an aesthetic improvement that meets the patient’s expectations and an occlusion that is functional. Involving the patient in the decision making process is an important part of pre-surgical planning and as such providing patients with a ‘realistic’ simulation of the post-surgical result is becoming a necessity. The current method of planning uses profile views of the patient in the form of lateral cephalograms and profile photographs. The challenge of planning is to position the teeth in an ideal class I incisor relationship whilst at the same time producing the correct final soft tissue appearance bearing in mind that the skeletal hard tissue lays in between (Figure 6.1).
Figure 6.1 Shows the interaction between soft tissue, hard tissue and teeth during the planning and execution phases of orthognathic surgery. Source: Ayoub, A.F. and Khambay, B. (2012) A paradigm shift in the diagnosis and management of dentofacial deformities. The Saudi Dental Journal, 24, 121–125. Reproduced with permission of Elsevier.
Orthognathic surgical planning should achieve the following objectives:
6.3 Methods of prediction planning
6.3.1 Model planning
Model surgery prediction is based on surgical procedures performed on study models, which are sectioned to achieve normal occlusal relationships. This gives an indication of the surgical skeletal movements required to correct the malocclusion but provides no information about the soft tissue change. It was soon realised that this approach may be detrimental to the facial profile and that an approximately ideal occlusion may not be accompanied with the best facial aesthetic results. However, model planning is still essential to predict the final dental occlusion and to construct the intermediate and final orthognathic wafers to guide the surgical procedure. This is dealt with in greater detail in Chapter 5 Orthognathic technical procedures.
6.3.2 Soft tissue profile prediction planning
Combined cephalometric tracings and photographs
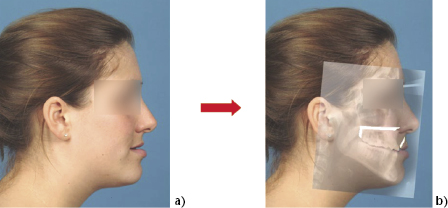
Henderson (1974) introduced a technique that combined cephalometric radiographic tracings with photographs. A lateral transparent positive 1:1 photograph was superimposed on the patient’s lateral cephalometric radiograph. A tracing was made of the relevant hard tissue structures from the cephalometric radiograph onto the photograph. The photograph was then sectioned along the planned osteotomy sites and moved according to the desired surgical movements. The soft tissues were then moved according to the known ratios of hard to soft tissue movements, as in Figure 6.2.
Figure 6.2 1:1 prediction planning. Pre-operative profile (a). Superimposed lateral cephalogram radiograph showing predicted hard and soft tissue movements following a maxillary advancement (b).
These photocephalometric planning techniques have proved useful in orthognathic planning and have been used in many centres, and are still being used in many units, to plan the outcomes of orthognathic surgery. These techniques, however, have a number of limitations:
6.3.3 Computerised prediction
In an attempt to overcome the limitations of the manual techniques, a number of computer-based packages have been developed. The early computer packages were able to generate simple line drawings of profile prediction. Following the evolution and development of computer hardware and software, prediction imaging packages are able to incorporate lateral profile photographs of the patient, which could then be morphed to produce photo realistic predictions.
All of the modern commercially available packages are in essence computerisations of the manual planning technique. Firstly, specific landmarks are digitised on both the lateral cephalometric radiograph and the profile photograph; the number of landmarks vary for each program. The prediction software then automatically superimposes the radiograph and photograph. Obviously the soft tissue on both the cephalogram and the profile photograph needs to be identical for the best superimposition. The method of superimposition is often not known to the operator and the factors which may effect the accuracy are therefore unknown. The orthodontist or surgeon is then able to analyse dental, skeletal and soft tissue variables against standardised sets of linear and angular measurements and plan the surgery on-screen. The software is programmed using mathematical algorithms to allow the simulation of hard and soft tissue movements. The final profile prediction is a ‘morphed and smoothed’ photo realistic prediction of the proposed surgical outcome. Some packages allow the clinician to “tidy-up” the lips if they appear incorrect; this however introduces a subjective element to the prediction which may introduce even larger inaccuracies.
Advantages of computerised prediction
Disadvantages of computerised prediction
6.3.4 Factors affecting the accuracy of prediction planning
The accuracy and reliability of prediction planning is dependant on a number of factors. These include:
6.3.5 Hard tissue and soft tissue ratios
Regardless of the method of prediction planning the hard and soft tissues are broadly the same and based on historical data, Figure 6.3. Orthognathic surgical simulation programs are based on algorithms that relate soft tissue response to the underlying skeletal change. The soft tissues are stretched, or become thinner as the maxilla is advanced in surgery and interpreting this interaction is important in predicting the outcome. The relative changes are expressed as mean ratios of soft tissue movements versus those of the hard tissues, and the software packages are based on these values. Therefore, though clinically useful, computerised predictions of soft tissue profile changes after orthognat/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


