8
High level osteotomies
- Have an understanding of the usage and indications for standard and high level osteotomies and the principles of timing for surgery.
- Have an explanation of the basic surgical procedures and the principles behind them.
- Recognise the surgical limitations, risks and possible complications that can occur.
- Have an understanding of the reasons for long term follow up and the necessity for repeat procedures as a result of failure of growth after birth.
- Have a basic knowledge for information to patients searching for treatment.
8.1 Introduction
There are a variety of osteotomies that may be used in the midface for the correction of deformity which have a small place in the repertoire of the maxillofacial surgeon primarily for the correction of craniofacial and asymmetric deformity. The principal ones are the Le Fort II and Le Fort III osteotomies outlined here.
Le Fort II and III osteotomies are based on the fracture lines which occur following trauma and these have been modified over the last 40 years to correct congenital deformities of the midface. They also may be used for post traumatic, secondary cleft and iatrogenic deformities (e.g. post radiotherapy) and they can be extensively modified to correct asymmetric deformity and for localised osteotomies in the craniofacial area.
8.2 Indications
8.2.1 The Le Fort II osteotomy (Figures 8.1a, 8.1b)
This is most effective where there is central midface (naso-maxillary) hypoplasia with both anteroposterior and vertical deficiency without significant orbital hypoplasia or ocular proptosis. There may be a degree of telecanthus or hypertelorism. It is most effective in von Binder’s syndrome (maxillo-nasal dysplasia), (Figure 8.2) and post traumatic cases (Figure 8.3). When there is infraorbital hypoplasia the procedure may be extended laterally, but there is a risk of damage to the infraorbital nerve. It is most useful for cases with a short hypoplastic nose, with moderate vertical and anteroposterior deficiency.
Figure 8.1 Le Fort osteotomy cuts.
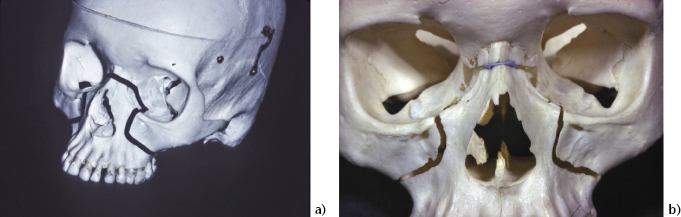
Figure 8.2 von Binder syndrome pre- and post-op.
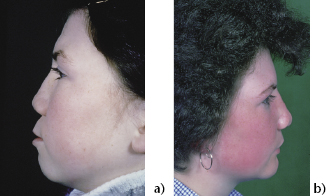
Figure 8.3 Malunited fracture corrected by Le Fort II osteotomy.

8.2.2 The Le Fort III osteotomy
This is primarily indicated for total midface hypoplasia, where there is deficiency affecting maxillae, malars and nasoethmoidal complex, especially in the presence of exorbitism. This is typically seen in syndromic and non-syndromic craniosynostosis, where the base of skull and the coronal sutures are affected. Many milder degree cases may be corrected by a subcranial procedure. This can also be used for untreated post-traumatic deformity and for major craniofacial clefting defects. An additional Le Fort I osteotomy is often required to increase the maxillary vertical dimension or to improve the dental occlusion. (The Kufner modification where the nasoethmoidal complex is left in its original position and the malars and maxillae are advanced is occasionally helpful but often it is difficult to obtain a good dental occlusion, and it is then better to do two malar osteotomies with a separate Le Fort I procedure.)
The Le Fort III osteotomy is widely used either subcranially or transcranially for deformities associated with the craniosynostotic syndromes of Crouzon, Apert, Carpenter, Pfeiffer and Saethre-Chotzen. Care needs to be taken when there is only slight exophthalmos associated with major midface hypoplasia which is sometimes seen in Apert’s syndrome. Any major advancement with distraction osteogenesis can lead to enophthalmos and then bone grafting of the orbits will be necessary. Distraction osteogenesis is particularly useful for severe maxillary retrusive deformity, as it largely avoids the necessity for extensive bone grafting. The latter is difficult to do when the child is very young, that is, between 1 and 5 years when surgery is necessary at that stage.
8.3 Timing of surgery
If surgery is to be carried out for aesthetic reasons this is best done at the end of the growth period (females 17 to 18 years and males 18 to 19 years) as a single procedure with pre and post surgical orthodontic care. However in most syndromic cases early release of cranial sutures is required between 8 and 15 months of age to allow the brain to grow. It triples its volume in the first year, after that there is only a small increase in its size. Premature suture closure will lead to raised intracranial pressure, brain damage and loss of vision. Early surgery for release of cranial sutures and frontal (supraorbital) advancement is then required. Following this the facial deformity appears much worse and sometimes this is complicated by postnasal choanal atresia accompanying the midface retrusion with airway problems and obstructive sleep apnoea. Early (<18 months) midface advancement surgery is difficult with poor control of the facial bones and it is better if possible to wait until 5 to 10 years. A tracheostomy or a CPAP machine may be required to improve the airway until surgery is carried out. Prior to any early surgery, it is essential to exclude other congenital anomalies, for example, cardiac, respiratory and neurological and to check the family history especially for other recessive and dominant conditions. A psychological assessment of children and young adults should always be considered before this type of surgery.
8.4 Special investigations
Prior to surgery a neurological check for raised intracranial pressure should be made with CT/MRI scanning. CT scanning of the mid- and upper face with three-dimensional, axial and coronal cuts is necessary. Any suspected or identified intracranial problems are additionally likely to require magnetic resonance imaging as well as the usual postero-anterior and lateral cephalograms for orthognathic planning purposes. If there is asymmetry of any significance then stereolithography is helpful. Intraoral dental views may be required as well as an orthopantomograph and dental models. From the general medical point of view a chest x-ray, routine haematology and biochemistry would be appropriate as well as a preoperative neurosurgical and anaesthetic assessment and a check for other systemic disease. A team approach is adopted for all orthognathic cases.
8.5 Le Fort II surgical procedure
An intraoral incision from right to left malar buttresses as for the Le Fort I osteotomy is made. Mucoperiosteal flaps are raised to expose the infraorbital margins and the nasomaxillary area and the whole of the pyriform aperture. Bilateral oblique canthal (medial) incisions are made through skin onto the frontal process of the maxillae just lateral to the external angular veins. The subperiosteal stripping is continued over the bridge of the nose, elevating the soft tissues well into the orbits without damaging the infraorbital nerves, nasolacrimal ducts and lacrimal sacs.
The bone cuts are made with burs starting midway between the infraorbital nerve and naso-lacrimal duct on each side slightly obliquely and inferiorly then horizontally across the zygomatic buttresses to the pterygo-maxillary junctions on both sides (Figure 8.1). Via the canthal incision a bur cut is made through the infraorbital margin and is then extended medially behind the naso-lacrimal duct with a small chisel. The bur cut is completed medially through the lateral wall of the naso-ethmoid elevating the soft tissues with an Aufricht retractor and across the bridge of the nose below the fronto-nasal suture to join a similar cut from the opposite side. The medial canthi remain intact and attached to the elevated periosteum. A curved Tessier chisel is then directed inferiorly through the canthal incision on one side to section the nasal septum and vomer completing the cut into the nasopharynx, at the same time checking its position in the nasopharynx. The lower portion of the pterygoid plates are separated from the maxillae with Tessier chisels. With Rowe’s disimpaction forceps the midface is mobilised, taking care to avoid tearing the naso-lacrimal ducts. This can be difficult in post-traumatic and secondary cleft deformities. I/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


