2
Dentofacial assessment
- Understand the importance of taking a full history from the patient.
- Understand the importance of correctly positioning the patient’s head prior to facial assessment.
- Be aware of the systematic approach required in carrying out a facial and intra-oral assessment of an orthognathic patient.
- Understand the function of the basic diagnostic records used in the management of orthognathic patients.
- Be aware of the commonly used objective soft tissue analyses.
- Be aware of the indications and purpose of three-dimensional imaging, including Stereophotogrammetry and Cone Beam Computerised Tomography.
- Be aware of the role of cephalometric analysis, including its limitations.
- Understand the importance of recognising progressive facial dysmorphology and the need for special investigations in some cases.
- Understand when referral to other medical and dental specialists is required.
2.1 Introduction
Assessment of the orthognathic patient should be carried out systematically to ensure that a complete picture of the presenting dentofacial dysmorphology is assembled. A pro-forma may be helpful in guiding the clinician through the assessment in planned sequence and documenting the findings in a structured manner. The purpose of this chapter is to describe the level of assessment that we consider to be essential on an inter-disciplinary planning clinic. Psychological assessment of the patient is an invaluable part of this and has been described in detail in Chapter 1. The procedure on our clinic is that all new patients are interviewed by the psychologist first and then progress to clinical examination only if given the ‘green light’.
2.2 General assessment
2.2.1 Patient’s concerns
Because orthognathic surgery is largely elective in nature, the patient’s concerns are the main reason for pursuing treatment and must be carefully elicited from the outset. Whilst most patients will describe one or more clear problems, some will be more vague and will have to be probed more thoroughly to establish exactly what they are seeking to derive from treatment. In general, patients’ concerns fall into the following categories:
If the psychologist can be present on the clinic when the patient is being examined, this is valuable in helping the patient to express their concerns and the clinicians to understand them.
2.2.2 Medical, dental and social history
As with any surgical or dental patient, a full medical history should be taken prior to clinical examination. It is not within the scope of this book to detail the medical conditions that will impact on the delivery of orthognathic surgery, but if the patient reports any significant illnesses at initial assessment it is prudent to contact the General Medical Practitioner or Consultant Specialist for clarification or further investigations prior to an appointment on the combined clinic.
It is important to establish the patient’s level of dental motivation and ensure that they will have the ongoing support of a General Dental Practitioner for the duration of their treatment. If there is a history of dental anxiety it is important to make sure that the patient will be able to cope with the challenges of surgical orthodontic treatment.
A patient’s social history should at least include questioning about home circumstances, smoking and alcohol consumption. It is also important to know about any history of mental health problems, but specialist questioning in this area is most appropriately undertaken at the psychology interview.
2.2.3 History of dentofacial dysmorphology
A history should be taken from the patient regarding the development of their dentofacial problems. This should include the following:
It is important to recognise progressive facial dysmorphology, which most commonly manifests as follows:
It is important to elicit the most accurate possible history regarding the progress of these conditions. Previous family or school photographs, if available, can be extremely helpful.
2.2.4 Stature and body form
The patient’s height and general body shape should be noted early on in the assessment, since orthognathic treatment should be aimed at delivering facial proportions that are in keeping with the patient’s build. A tall, lean patient is unlikely to suit a disproportionately reduced lower anterior face height and a short, broad patient is unlikely to suit an increased lower anterior face height. Similarly, a patient’s stature may influence the surgical plan in the antero-posterior plane. For example, in certain class III patients, standing height might play a part in deciding whether surgical correction would be by means of a maxillary advancement or a mandibular setback.
Where a patient is clearly overweight this can be a contra-indication for elective orthognathic surgery. In such cases, the patient may be required to reduce their weight before they can be considered for treatment. The Body Mass Index (BMI) is helpful as a guide.
2.3 Facial assessment
The following is a suggested systematic approach to clinical assessment of facial dysmorphology. See also Tables 2.1a and b.
Table 2.1a Soft tissue profile cephalometric landmarks
| Landmark | Definition |
|---|---|
| Tr | Trichion: the anterior hairline in the midline. |
| G | Glabella: the most anterior point on the soft tissue outline of the brow ridge. |
| N’ | Soft tissue nasion: the deepest point on the soft tissue outline below glabella. |
| Prn | Pronasale: the most anterior point on the outline of the nose. |
| Cm | Columella: the most anterior point on the columella of the nose. |
| Sn | Subnasale: the junction of the upper lip and the columella. |
| A’ | Soft tissue A point: the deepest point on the anterior outline of the upper lip below Sn. |
| Ls | Labrale superius: the muco-cutaneous junction of the upper lip. |
| Sts | Stomion superius: the lowermost point on the vermillion of the upper lip. |
| Sto | Stomion: the point of contact, in the midline, between the upper and lower lips, where the lips are competent. |
| Sti | Stomion inferius: the uppermost point on the vermillion of the lower lip. |
| Li | Labrale inferius: the muco-cutaneous junction of the lower lip. |
| B’ | Soft tissue B point: the deepest point on the anterior outline of the lower lip, above Pg’. |
| Pg’ | Soft tissue pogonion: the most anterior point on the soft tissue outline of the chin below B’. |
| Me’ | Soft tissue menton: the most inferior point on the soft tissue outline of the chin. |
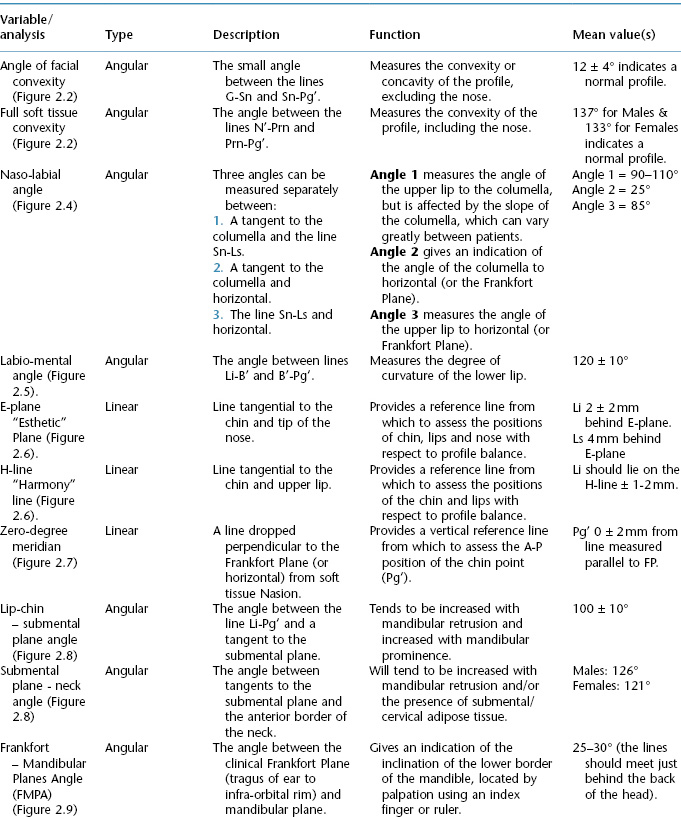
Table 2.1b Summary of soft tissue variables
2.3.1 Lateral view
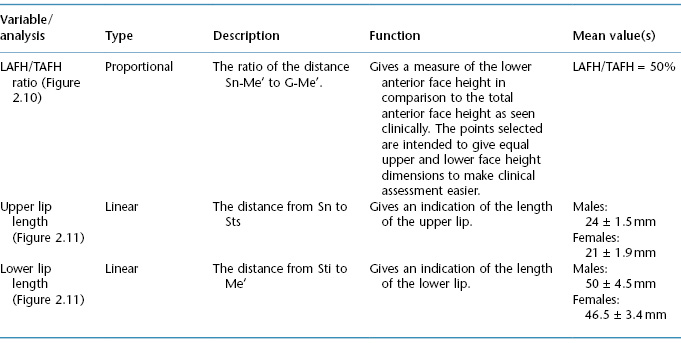
The patient should be seated comfortably with their back in an upright position and asked to adopt their natural head posture (NHP), in which they are generally viewed in everyday life. This can be made easier by asking them to look in a mirror mounted straight ahead of them. The alternative method of positioning the Frankfort Plane (FP) parallel to the floor may place them in an artificial position, since this not a reliable horizontal reference plane in patients with significant facial skeletal discrepancies. It has been shown that NHP is more reliable than FP for orientation of the head. Inappropriate head positioning can result in a false perception of the antero-posterior jaw relationship (Figure 2.1).
Figure 2.1 The patient’s head posture can affect the clinical impression of their antero-posterior jaw relationship.
Habitual tilting of the head to the left or right side should be avoided. However, for patients that have a condition that produces involuntary tilting, such as tortocollis (due to shortening of one of the sterno-mastoid muscles), this should be accepted as their normal posture, as it is unlikely to improve as a result of surgery.
It is important for the peri-oral soft tissues to be relaxed, particularly in patients with increased vertical proportions, who may have incompetent lips and will tend to habitually posture them together through mentalis muscle hyper-activity.
Viewing the face from the lateral aspect allows the assessment of:
- Jaw relationship and facial convexity.
- Forehead.
- Infra-orbital rims.
- Nose.
- Para-nasal region.
- Upper lip.
- Lower lip and chin.
- Lower lip to sub-mental plane angle.
- Mandibular plane angle.
Jaw relationship and facial convexity
The left and right sides of the head should be examined separately, since characteristic differences will be detected in asymmetric faces.
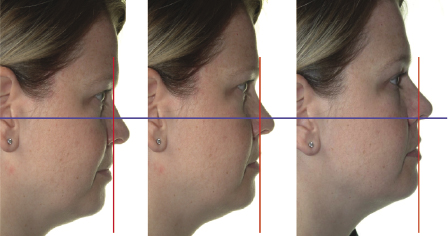
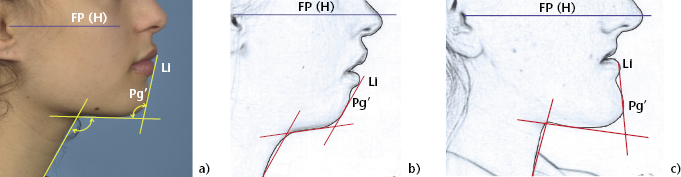
The relative antero-posterior positions of the maxilla and mandible, as well as the convexity of the profile, can be assessed subjectively by looking at the patient’s profile in natural head position. The facial convexity can also be measured objectively on a profile photograph, including or excluding the nose, as illustrated in Figure 2.2a. A class II jaw discrepancy will generally manifest as a convex profile (Figure 2.2b), while a class III profile will be concave (Figure 2.2c).
Figure 2.2 (a) Angle of facial convexity (the small angle between G-Sn and Sn-Pg’) excludes the nose, while the angle of total facial convexity (the small angle between N’-Prn and Prn-Pg’) includes the nasal tip. These angles tend to be increased in class II cases (b) and reduced in class III cases (c).
In some class III cases, the drape of the upper lip can mask the underlying maxillary deficiency to a large extent and present a deceptively normal soft tissue profile. This is most likely in high angle cases where there is a degree of bi-maxillary retrusion owing to the downward and backward position of the chin.
In class II cases, maxillary protrusion is uncommon, relative to the patient’s racial norm, but it is not uncommon to see bi-maxillary retrusion, particularly in patients with long facial types. In such cases, the telltale signs of maxillary deficiency will be present, such as para-nasal hollowing (Figure 2.3). In class III cases, maxillary deficiency is common but again, in high angle cases, bimaxillary retrusion with retrogenia can be present.
Figure 2.3 This patient with maxillary deficiency exhibits para-nasal hollowing, indicated by the yellow line.

Forehead
It is important to note the position and shape of the forehead, since it is one of the parts of the face that will remain completely unchanged by orthognathic surgery. If frontal bossing is present or the forehead is flat, this should be taken into account when assessing the jaw positions and the effects of surgery, such that harmonious facial balance will be achieved.
Infra-orbital rims
The antero-posterior position of the infra-orbital rim can be assessed relative to the globe of the eye and the supra-orbital ridge. A deficient infra-orbital rim will tend to accompany high-level deficiency of the maxilla and is usually a part of mid-face hypoplasia.
Nose
The shape of the nasal dorsum and the angle of the nasal tip may be affected by maxillary osteotomy and it should be carefully noted whether or not such changes are likely to be favourable. For example, a patient with maxillary deficiency who already has an up-turned nasal tip is likely to experience a worsening of this feature with a Le Fort 1 advancement osteotomy. On the other hand, a patient with a long facial type and a down-turned nasal tip may well experience an improvement in their nasal profile as a result of Le Fort 1 impaction osteotomy.
In addition, an assessment of the prominence of the nose in relation to the forehead and chin is essential, in diagnosing the jaw discrepancy and planning the required surgical correction (Figure 2.2).
Para-nasal region
The contour of the skin overlying the area just lateral to the alar base can be seen from the side view. A lack of bony support for the soft tissues in this region will produce a depression described as para-nasal hollowing, which is indicative of low level antero-posterior maxillary deficiency (Figure 2.3). Although most commonly associated with class III jaw discrepancies, it can also be present in class II cases with bi-maxillary retrusion.
Upper lip
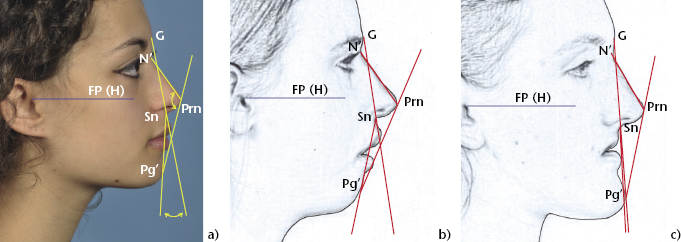
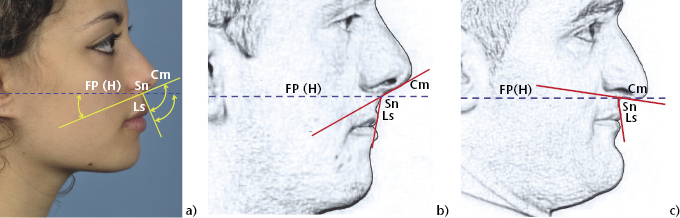
It is important to assess the form and angle of the upper lip. The naso-labial angle is often taken as an indication of the position of the underlying maxilla and incisors. However, it is prone to variation according to the slope of the columella and the curvature of the upper lip and the angle can be measured in a number of different ways (Figure 2.4a). A patient with maxillary deficiency will tend to show an increased naso-labial angle (Figure 2.4b). However, an unusually short upper lip may be more furled than average, or the columella may be down turned, giving rise to an acute angular measurement, even in the presence of maxillary deficiency (Figure 2.4c). Conversely, some patients present with a deficient maxilla but the proclined upper anterior teeth support the upper lip.
Figure 2.4 (a) The naso-labial angle is measured between Sn-Cm and Sn-Ls. The angles between these lines and the Frankfort Plane (or horizontal reference line) allow the slope of the columella to be accounted for. (b) In this class III case the naso-labial angle is increased. (c) This class III patient’s naso-labial angle is reduced due to a down turned columella, but the angle of the upper lip to horizontal is within the normal range.
Lower lip and chin
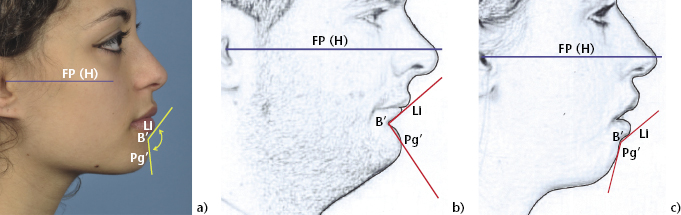
The curvature of the lower lip is dependent mainly on the depth of the labio-mental fold (Figure 2.5a), which in turn, tends to reflect the inclination of the lower incisors, the antero-posterior position of the chin point (soft tissue pogonion) and the lower anterior face height. As a general rule, a reduced lower anterior face height, with accompanying progenia, will produce an accentuated labio-mental fold (Figure 2.5b), whilst a flat lower lip will be associated with retrogenia and increased vertical dimensions (Figure 2.5c).
Figure 2.5 (a) The labio-mental angle (between Li-B’ and B’-Pg’) gives a measure of lower lip curvature. It is reduced in the short-faced patient shown in (b), and increased in the long-faced patient shown in (c).
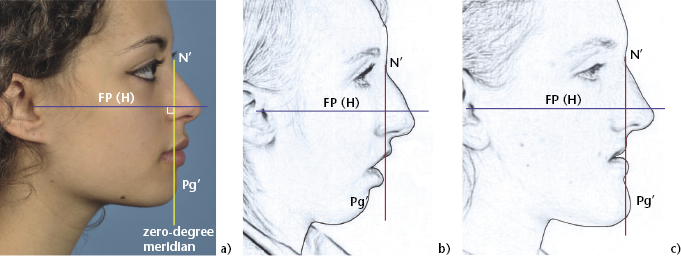
The profile balance of the lips in relation to the chin and nose can be assessed using various indicator lines, including the ‘Esthetic’ or E-plane and the Holdaway Harmony or H-line (Figure 2.6). The antero-posterior position of the chin should be assessed in relation to the forehead and the upper face. The zero-meridian line (Figure 2.7a) is helpful in clinically identifying mandibular retrognathism (Figure 2.7b) and prognathism (Figure 2.7c), but particular attention must be paid to the patient’s head posture since the position of the vertical line at the level of the chin will vary significantly with any upward or downward tilting (Figure 2.1).
Figure 2.6 The Ricketts “E” Plane is tangential to the chin and nasal tip. The Holdaway “H” line is tangential to the chin and upper lip.
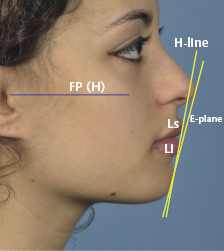
Figure 2.7 (a) The Ricketts zero-meridian line is a constructed vertical line dropped perpendicular to the Frankfort Plane (or horizontal) from N’. It gives an indication of the antero-posterior position of Pg’, which will lie behind the line in class II cases with mandibular retrusion (b) and in front in cases with mandibular prognathism (c).
Lower lip to sub-mental plane angle
The angle of the lower lip to the sub-mental plane (throat) is important for pleasing facial aesthetics and it should be close to a right angle in an average face (Figure 2.8a). In addition to the inclination of the lower lip, the angle is equally dependent on the slope of the sub-mental plane, which varies with the degree of mandibular prognathism, the chin position and the vertical dimension of the face, as well as the presence of sub-mental adipose tissue (Figure 2.8b,c). The appearance of excess tissue in this region can be unaesthetic, particularly if the throat length is short, and it is important to note how this might be affected by surgical changes to the position of the mandible and the chin.
Figure 2.8 (a) The lower lip to sub-mental plane angle is measured between the lines Li-Pg’ and a tangent to the submental plane. (b) A class II case with increased vertical dimension and retrogenia, in which the angle is increased and (c) A Class III case, in which the angle is reduced.
Mandibular plane angle
The angle of the mandibular plane can be assessed by placing an index finger or a ruler along the lower border of the mandible and the Frankfort Plane. The point of intersection of the two planes should be just behind the back of the head where the angle is average. The effect on this point of intersection can be seen in low and high angle cases in Figure 2.9. In the presence of facial asymmetry, the right and left mandibular planes may differ and must be assessed separately.
Figure 2.9 The clinical Frankfort-mandibular planes angle is reduced in short-faced patients (a) and increased in long-faced patients (b).
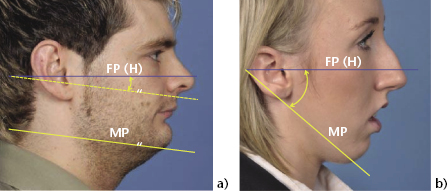
It must be remembered that the Frankfort Plane can deviate from normal and, as mentioned previously, may not be horizontal with the head in NHP. If there is any doubt then it is advisable to position the patient correctly and then use a true horizontal line as a reference.
2.3.2 Frontal view
Viewing the face from the front allows assessment of:
- Vertical proportions.
- Vertical asymmetries.
- Transverse proportions.
- Transverse asymmetries.
- Ear shape and position.
- Scleral show and eye lid shape.
- Upper incisor show.
- Lip form and symmetry.
Vertical proportions
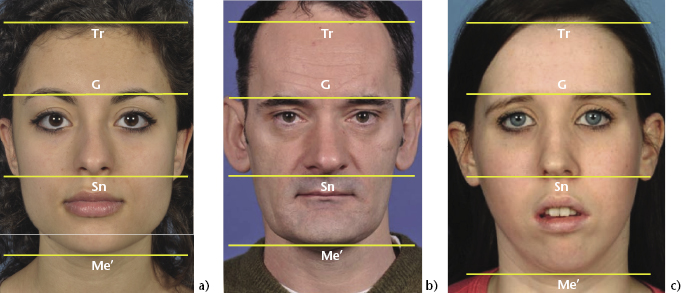
Viewed from the front, the face can be divided vertically into thirds and the dimensions of the upper, middle and lower facial heights compared. The vertical distance from subnasale (Sn) to soft tissue menton (Me’) represents the lower anterior face height (LAFH) and this can be compared to the total anterior face height (TAFH), represented by the vertical distance from glabella (G) to Me’. These landmarks are used so that the proportions of the upper and lower anterior facial heights are approximately equal in an average facial type. The ratio of LAFH:TAFH is reduced in short-faced patients and increased in long-faced patients (Figure 2.10).
Figure 2.10 (a) Normally proportioned face divided into equal vertical thirds (Tri-G’, G’-Sn and Sn-Me). Lower anterior face height reduced in a short-faced patient (b) and increased in a long-faced patient (c).
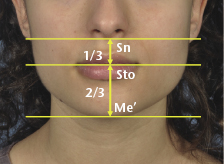
Within the lower anterior facial third, further sub-divisions allow the vertical proportions of the upper and lower lips to be assessed. The upper lip length is measured from subnasale to stomion superius, which is normally 50% of the length of the lower lip, measured from stomion inferius to soft tissue menton (Figure 2.11). Where the lips are incompetent, it is probably most valid to measure the heights of the upper and lower lips individually along with the overall lower face height proportions.
Figure 2.11 Vertical sub-divisions of lower anterior facial third, showing normal ratio of upper and lower lip lengths.
Vertical asymmetries
Upper facial asymmetry.
The evaluation of vertical asymmetries is usually carried out with reference to the inter-pupillary line. Occasionally the orbits may be at different levels (dystopia) and, if this is the case, judgement will be required to identify a horizontal plane that allows meaningful assessment of structures lower down the face. Vertical asymmetry of the zygomatic bones is usually associated with traumatic injuries, which have not been corrected appropriately.
Canting of the maxillary occlusal plane.
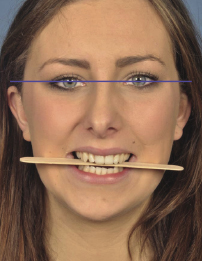
A common method of assessing canting of the maxillary occlusal plane is by placing a wooden tongue spatula across the premolars and relating it to the inter-pupillary line (Figure 2.12). Care should be taken to avoid being misled by over-erupted teeth or canine cusps of different lengths, which may tip the spatula in a way that does not accurately reflect the skeletal base.
Figure 2.12 A tongue spatula is useful in assessing canting of the maxillary occlusal plane.
Vertical mandibular asymmetry.
Vertical mandibular asymmetry is evident in patients with unilateral condylar hyperplasia, hypoplasia or agenesis, which affects the height of the rami. Hemi-mandibular hypertrophy causes a downward bowing of the lower border on the affected side, with increased depth of the body. If there is an accompanying cant of the mandibular occlusal plane with any of these conditions, then this should be assessed using a tongue spatula in the same way as for the maxillary plane.
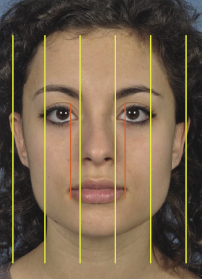
Transverse proportions
The face can be divided into fifths to allow transverse proportions to be assessed (Figure 2.13). This is particularly relevant in patients planned for Le Fort I advancement or impaction osteotomy, where the alar base is prone to flaring. A narrow alar base may well improve in appearance through surgery, while a broad one may be at risk of looking overly flared. Procedures available to the surgeon for controlling this are described in Chapter 7.
Figure 2.13 A normally proportioned face can be divided into equal fifths (long lines). The middle fifth should equal the width of the alar base and the inter-canthal distance. Further sub-divisions (short lines) illustrate that the width of the stoma should be approximately equal to the inter-iris distance.
Transverse asymmetries
Before assessing the transverse symmetry of the face it is essential to check that the patient is holding their head level, without any side-to-side tilting. The base of the neck and clavicles should be exposed, with the patient’s consent, to allow full assessment of the neck and head posture.
Envisaging the facial midline.
Every face has subtle asymmetries and only significant asymmetries require assessment. Before attempting to assess any transverse asymmetry it is necessary to envisage the facial midline. If an asymmetry involves just the mandible then it is usually straightforward to establish a reference line running down the middle of the forehead, bisecting the inter-pupillary line and continuing down through the middle of the dorsum of the nose and philtrum of the upper lip. Where more complex asymmetries are present higher up in the face, for example, in cases with dystopia, this is less straightforward and an element of judgement is required to envisage a reference line that most accurately represents the midline. The nose can also exhibit asymmetry of both the dorsum and the tip. It is essential to identify any nasal asymmetry and ensure that it is not influencing the position of the facial midline, before assessing the symmetry of the lower facial structures. Otherwise the extent of an asymmetry lower down the face could be either accentuated or diminished.
Upper facial asymmetry.
In the upper face, it is mainly the lateral projection of the zygomatico-orbital complex that needs to be assessed for symmetry.
Dental centrelines.
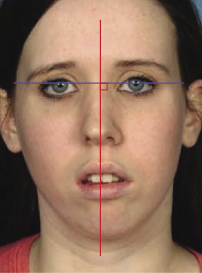
The upper centreline should first be assessed in relation to the facial midline (Figure 2.14). The exact upper centreline position can be difficult to determine, particularly in cases where there are other asymmetries present. Again, holding a ruler along the envisaged facial midline is a useful aid. The middle of the philtrum is also an important reference for the position of the upper centreline, particularly where nasal deviation is present. The position of the lower centreline should then be noted relative to the upper centreline and to the midpoint of the chin, as well as to the facial midline. Where there is a shift of the lower centreline relative to the facial midline, but not relative to the midpoint of the chin, it is important to determine whether it is due to a true mandibular asymmetry or a displacement on closure due to an occlusal interference, particularly if a unilateral buccal segment cross-bite is present (see also Section 2.4).
Figure 2.14 The facial midline is dropped perpendicular to the inter-pupillary line, provided the orbits are level. In this patient, there is deviation of the nasal tip to the right and a shift of the upper dental centreline and the chin point to the left.
Transverse mandibular asymmetry.
In evaluating transverse mandibular asymmetry, the position of the chin point relative to the facial midline must be carefully assessed. As mentioned above, it is important to take into account any nasal deviation as well as any asymmetry of the lips. Marking a dot where the middle of the soft tissue chin point is thought to be and then holding a ruler along the facial midline i/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


