Chapter 6 Occlusion
Bruxism
Most bruxism is mild and non-damaging to tooth tissue; as such, no treatment is required. However, for some, tooth wear and fracture may occur or the noise of grinding is unacceptable for partners and treatment is sought. For these patients a correctly adjusted hard acrylic splint can be supplied for night-time or daytime wear to protect the teeth. Such splints are referred to as stabilization splints and can be worn in the maxillary (Michigan splint, Figure 6.1; see also Chapter 4) or mandibular (Tanner appliance) arch.
An alternative splint is the localized occlusal interference splint (LOIS appliance, Figure 6.2). This consists of an acrylic plate retained by suitable clasps and two ball-ended wires which are placed between opposing teeth to interfere with the occlusion. Occlusal loading of the ball interferences leads to stimulation of periodontal mechanoreceptors, afferent feedback and reduction in occlusal loading. When used for bruxing habits, both splints act as a ‘habit breaker’ and patients can be gradually weaned off them.
Temporomandibular disorders
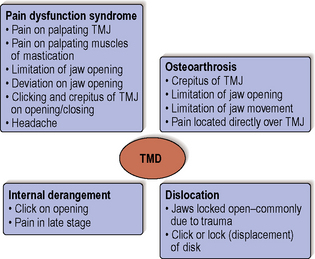
Within the dental literature there seems to be no agreement as to a definition for temporomandibular disorders (TMD). What is clear is that TMD covers a number of complex conditions with common signs and symptoms. The conditions are defined in the glossary of prosthodontics terms as those producing ‘abnormal, incomplete or impaired function of the temporomandibular joint(s)’. The most common conditions making up these disorders, together with their signs and symptoms, can be seen in Figure 6.3. A number of terms have been given to the signs and symptoms allotted to pain dysfunction syndrome, some of which include myofascial pain, craniomandibular dysfunction and mandibular dysfunction. Rarer causes of TMD are rheumatoid arthritis, psoriatic arthritis, developmental defects, infection, neoplasia and ankylosis.
Patient examination
Extraoral examination
Facial appearance
The facial appearance can firstly be assessed for facial asymmetries and skeletal relationship. With the patient’s teeth in contact, the lower face height should be assessed in proportion to the total face height, especially in patients complaining of missing teeth and tooth wear. Loss of teeth and occlusal stops could result in an overclosed appearance but a reduction in lower face height is unusual in patients with tooth wear. This is because of dento-alveolar development or compensation which counterbalances the loss in coronal tooth tissue height. In fact it has been suggested that dento-alveolar development takes place in the absence of tooth wear and some researchers have shown an increase in face height with age. This is the mechanism which leads to overeruption of teeth when taken out of occlusion – for example, by loss of an opposing tooth (Figure 6.4).
Intraoral examination – examination of the occlusion
Intercuspal position (ICP)
Intercuspal position can be defined as the position of the jaws when the maxillary and mandibular teeth are in maximum intercuspation. This has also been referred to as centric occlusion. Patients usually close from a rest position immediately into this position due to a conditioned path of closure. It is important to establish whether the occlusion in ICP is stable; that is, an occlusion where there is no possibility of tooth movement, namely overeruption, drifting or tilting of teeth (Figure 6.5). If teeth are extracted or lost due to other causes, or if they lose their contour (a carious lesion cavitating, tooth fracture, tooth wear), occlusal contacts and interdental contacts, teeth can move, often complicating any subsequent restorative work (Figures 6.4 and 6.6).
When teeth overerupt in the absence of periodontal disease, the alveolar process remodels and the gingival margin moves with the tooth (see Figure 5.3, Chapter 5). This dento-alveolar compensation can happen quickly in some patients and is a reason why temporary crowns should be placed following tooth preparation for crowns or bridges; the occlusal and proximal reduction will result in an unstable occlusion and if no temporary is placed, overeruption and drifting of teeth could occur. This would result in a prosthesis that does not seat fully and appear to be occluding prematurely or appear ‘high’ in ICP.
Centric relation, terminal hinge axis position and retruded contact position (RCP)
Centric relation describes the jaw relationship between the maxilla and mandible when the mandible is in a retruded position. Differing definitions of centric relation have focused on slightly different positions of the condyle in the glenoid fossa and some on the relationship of the head of the condyle to the interarticular disc. These are rather academic arguments as clinically the position of the condyle cannot be visualized or confirmed without complex equipment. A more pragmatic and practical definition was proposed by Christensen in 2004 which conforms to most dentists’ clinical practice. He described centric relation as the ‘most comfortable posterior location of the mandible when it is bilaterally manipulated gently backward and upward into a retrusive position’. When this is done the mandible opens and closes on an arc of curvature around an imaginary axis drawn through the centre of the head of both condyles; this imaginary axis is termed the terminal hinge axis (Figure 6.7). Measured in the incisor region the arc of opening around the terminal hinge axis position takes place for about 20 mm before the condyles start to translate down onto the articular eminence (Figure 6.8). When the mandible closes in the terminal hinge axis position the first tooth contact is called the retruded contact position (RCP). The terminal hinge axis position is said to be the most reproducible jaw relationship; however, small variations from day to />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses