Chapter 1 Management of dental caries
Dental caries the disease
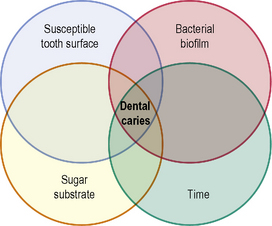
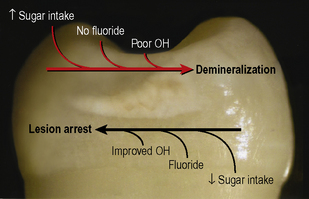
Dental caries is a disease that is common to all dentate individuals. At the hydroxyapatite crystal level it could be considered a ubiquitous phenomenon. For dental caries to occur a bacterial biofilm has to accumulate on a tooth surface. The bacteria within the biofilm metabolize dietary sugar substrates producing acids which, over time, lead to demineralization of the tooth tissue. Thus the requirements for the carious process may be depicted by the Venn diagram seen in Figure 1.1. However, this diagram is overly simplistic and implies that the disease process and its progression are inevitable. Clinically, this is not the case. Some tooth surfaces that are frequently covered in plaque do not develop clinically detectable caries whereas other tooth surfaces covered with plaque in the same mouth do. Many other factors, such as dietary habits, fluoride and saliva impact upon the disease process which is complex and dynamic in nature. From the earliest stage, continued demineralization is not inevitable and lesion arrest is possible by simply disrupting the plaque biofilm on the surface of the tooth at regular intervals. Very early lesions which are not detected clinically may therefore not progress to clinically detectable white spot lesions and the carious process is better represented by Figure 1.2.
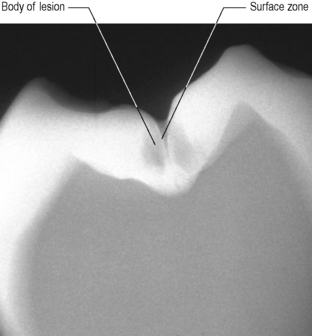
It is often said that if an early white spot lesion develops, remineralization can take place. While complete remineralization and resolution of the lesion is unlikely, the clinically apparent remineralization of a white spot lesion may also be due to its surface abrasion following improved oral hygiene procedures. Remineralization or regrowth of partially demineralized apatite crystals in the surface zone of an enamel lesion (Figure 1.3) has been reported. However, the relatively well-mineralized surface zone acts also as a diffusion barrier to ions, making it less likely that, in the underlying body of the lesion, supersaturation with respect to apatite will occur with subsequent mineral deposition. Prevention of the disease is therefore our primary aim. However, for many patients, this primary prevention fails and lesions develop. Caries risk assessment and early caries detection are important so that further prevention can be targeted to those patients and lesions that are in need. In this situation a method of monitoring the lesion is also important to determine the outcome of our preventive approach; that is, has the lesion arrested or progressed.
The restorative cycle
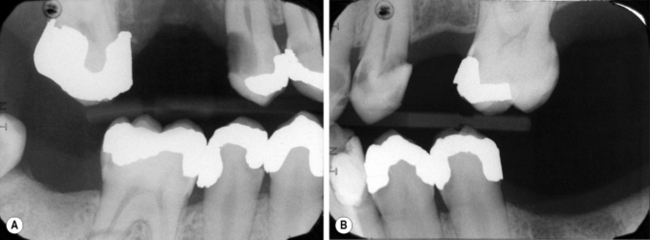
A significant proportion of a dentist’s work time is spent replacing restorations and the most common reason given to justify this clinical decision is the presence of secondary caries. This is caries that develops under or adjacent to a restoration placed to repair a carious lesion. The term secondary caries is, however, misleading as it implies that the restoration is somehow the cause. In certain situations this is true when the restorative procedures have been carried out incorrectly. For example, ledges create plaque stagnation areas, poor contact points allow food packing and poor adaptation with an inadequate bond of materials to tooth tissue leads to microleakage (Figure 1.4). Most ‘secondary caries’ is actually new caries that has just formed adjacent to the restoration and is better termed as such: caries adjacent to a restoration (CAR). The appearance of caries, following restoration of a tooth, illustrates the continued high caries risk of the patient and also shows that restoration alone does not change this. In order to prevent recurrence it is fundamental that the caries risk be managed. If successful, this might avoid the need for more advanced restorative work, and ensure its predictability when carried out.
Caries detection and diagnosis
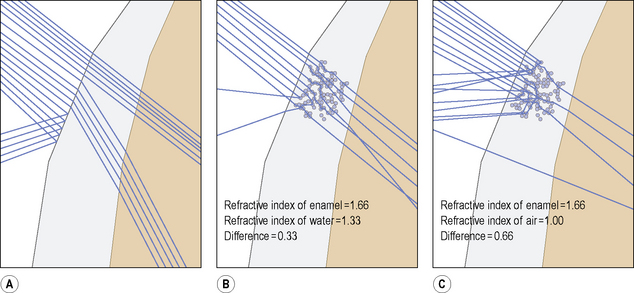
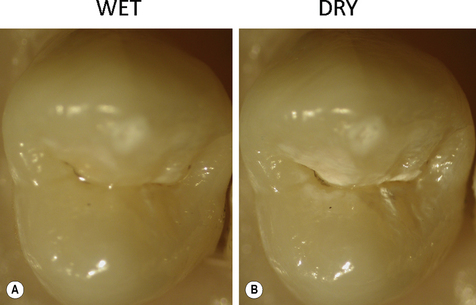
It is important when examining a patient for primary caries or caries adjacent to restorations that the teeth are examined clean. The carious process initially takes place in the biofilm on the surface of the tooth and the product of that process is the initial lesion in the tooth. To see the lesion and make a diagnosis the biofilm needs to be removed (Figure 1.5). It is also essential that the teeth are examined both wet and dry. The importance of drying is illustrated in Figure 1.6. When light illuminates a sound tooth, the light can either be transmitted, or it can undergo refraction or reflection. Refraction is the ability of a tooth to bend (scatter) light and will vary according to the refractive index of the material the light passes through. The porosities created in enamel during the carious process are normally filled with water (refractive index = 1.33) which has a refractive index close to enamel (1.66). In this situation little light scattering occurs. If the lesion is dried and the water is replaced with air which has a lower refractive index (1.0), the larger difference in refractive indices between enamel and air results in greater light scattering, enabling easier recognition of the white spot lesion. The occlusal lesion in Figure 1.7 clearly illustrates this and it stands to reason that a lesion that needs to be dried to enable its diagnosis is less severe than one that is seen even on a wet surface. The examination of clean teeth under both wet and dry conditions forms the basis for a clinical visual classification system known as the International Caries Detection and Assessment System (ICDAS II). This system characterizes lesions of increasing severity by correlating the visual appearance of the lesions with their histological depth (Table 1.1). The ICDAS II criteria can also be applied to caries adjacent to restorations. For further information on the ICDAS, visit the website http://www.icdas.org/index.htm.
Table 1.1 International Caries Detection and Assessment System (ICDAS II)a
| ICDAS Criteria | Collapsed Criteria for Clinical Use | Corresponding Histology |
|---|---|---|
| 0 No or slight change in enamel translucency after prolonged air drying (>5 s). | 0 No or slight change in enamel translucency after prolonged air drying (>5 s). | 0 No enamel demineralization or a narrow surface zone of opacity (edge phenomenon). |
| 1 Opacity or discoloration hardly visible on a wet surface, but distinctly visible after air drying. | 1 Opacity or discoloration hardly visible on a wet surface, but distinctly visible after air drying. | 1 Enamel demineralization limited to the outer 50% of the enamel layer. |
| 2 Opacity or discoloration distinctly visible without air drying. | 2 Opacity or discoloration distinctly visible without air drying. | 2 Demineralization involving between 50% of the enamel and the outer third of dentine. |
| 3 Localized enamel breakdown in opaque or discoloured enamel. | ||
| 4 Greyish discoloration from the underlying dentine. | 3 Localized enamel breakdown in opaque or discoloured enamel and/or greyish discoloration from the underlying dentine. | 3 Deminer/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses