6
Medical Emergencies
True medical emergencies in the dental office are rare and usually related to the complexity of the patient’s medical history, the difficulty of the dental procedures being performed, and the method of anesthesia/analgesia employed. Many are avoided if recognized early on, although some may require rapid and specific intervention when they arise. Vasovagal syncope is by far the most common medical “emergency” to occur in the in the dental office. It is less common in children than in adults. Less frequent, but of increased significance, are cardiovascular emergencies such as angina and acute myocardial infarction. Other important problems include hypertensive crisis, grand mal (generalized tonic–clonic) seizures, hypoglycemia, asthma, airway obstruction, anaphylaxis, and overdose of local anesthetic.
A thorough medical history and physical examination prior to the performance of the procedure are the keys to the identification of medical illnesses, the assessment of their severity, and the prevention of adverse events through appropriate preoperative preparation. For example, a patient with severe asthma may have a history of episodic high dose steroid use (Appendix 12, Table A12-1). This history, along with the assessment of the pulmonary status and ability to withstand an intravenous sedation or general anesthetic, provides valuable information for the treating clinician. This history of steroid use may lead to adrenal compromise with associated cardiovascular collapse under stress, which can be avoided with the appropriate prophylaxis.
The vast majority of medical emergencies in the dental office can be avoided by a good history and physical assessment and appropriate preoperative preventative measures. The medical complexity of the patient, the equipment available for management of the medical problem, and the actual management are all based upon the individual practitioner’s specific education, training, and scope of practice. The overview to follow is presented in both general and specific terms to provide readers with varying degrees of expertise and training a meaningful synopsis of the management of the most common medical emergencies in the dental setting. The use of algorithms is meant to provide an ordered, simple, step-by-step sequence for the management of these problems in a manner that provides clarity and priority in times of stress for both the patient and the practitioner.
Please refer to Appendix 12, Table A12-12 (Emergency Medications and Equipment), and Appendix 13 (Emergency Room Kit) at the end of this book.
Syncope
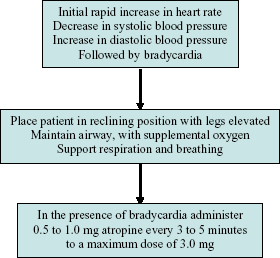
Syncope is the most common medical emergency in the dental setting. It can be the result of psychological stress (e.g. fear, pain, sight of blood), hypoglycemia, and pre-existing cardiovascular disease. Patients may describe nausea, light-headedness, blurry vision, and flushing. If the patient is attached to a cardiac monitor and sphygmomanometer, a syncopal episode, when witnessed, will be preceded by a brief episode of tachycardia, followed by bradycardia, hypotension, and a period of unconsciousness (Figure 6.1). Seizures and a postictal state immediately after syncope may be seen. Most syncopal episodes occur with unmonitored patients and thus the bradycardia, hypotension, and unconsciousness are the first signs and symptoms elicited, and all too frequently, it is the unconsciousness of the patient that is first noted.
Figure 6.1. Syncope.
Vasovagal Syncope
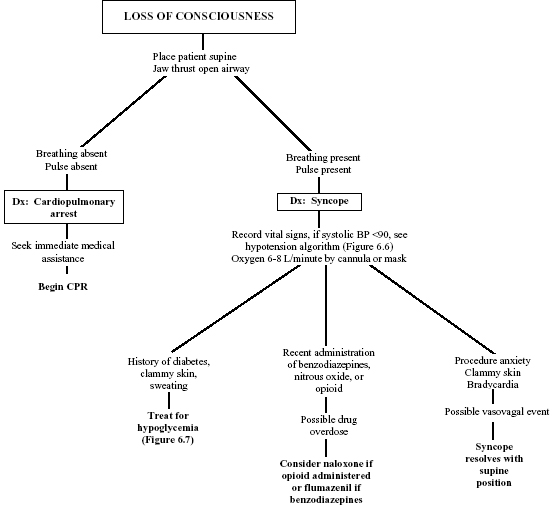
Psychological stress (fear, pain, sight of blood, illness) leads to increased vagal stimulation, venous pooling, and bradycardia. The result is decreased cerebral perfusion and loss of consciousness (Figure 6.2). This is the most common cause of syncope in adults in the dental surgery. Fifty percent of people have experienced syncope.
Figure 6.2. Evaluation of loss of consciousness.
Signs and Symptoms
- Pallor, flushed feeling, sweating, nausea, vomiting
- Weakness
- Light-headedness
- Dimming of vision
- Bradycardia
- Hypotension
- Brief unconsciousness
Treatment
- The management for syncope is supportive.
- Check for adequate pulse and respirations.
- Patient should be placed in Trendelenburg position (supine with feet elevated and head low). Pregnant females should be placed on their left side to prevent compression of the inferior vena cava.
- Loosen shirt collar to decrease carotid sinus stimulation.
- Provide oxygen at a flow of 6 to 8 L/minute by mask or nasal cannula.
- Aromatic spirits of ammonia placed into the nostril for five seconds should elicit a response in patients with vasovagal syncope.
- Blood pressure and pulse should be obtained. If blood pressure is less than 90 mmHg systolic, the patient should be treated as for shock.
- Syncope should resolve when the patient assumes the supine position. This is occasionally accompanied by brief (two to three seconds) tonic–clonic movements of the extremities.
- If the patient remains hypotensive, a fluid challenge may be provided (see the section of hypotension to follow) and atropine administered if intravenous access and medication administration is within the practitioner’s scope of practice.
- Once the episode appears to have resolved, be aware that the cardiovascular system does not fully recover for more than 30 minutes. There is the potential for the patient to have another syncopal episode if the dental procedure proceeds, and this prolonged recovery needs to be taken into consideration when the patient leaves the office.
Respiratory Difficulty
Numerous conditions result in respiratory difficulty. The key to management is to assess the patient while providing supportive care, to arrive at a diagnosis, and then to manage the patient based upon that diagnosis. For a patient who is short of breath, the algorithm in Figure 6.3 can help to triage the patient.
Figure 6.3. Evaluation of shortness of breath.
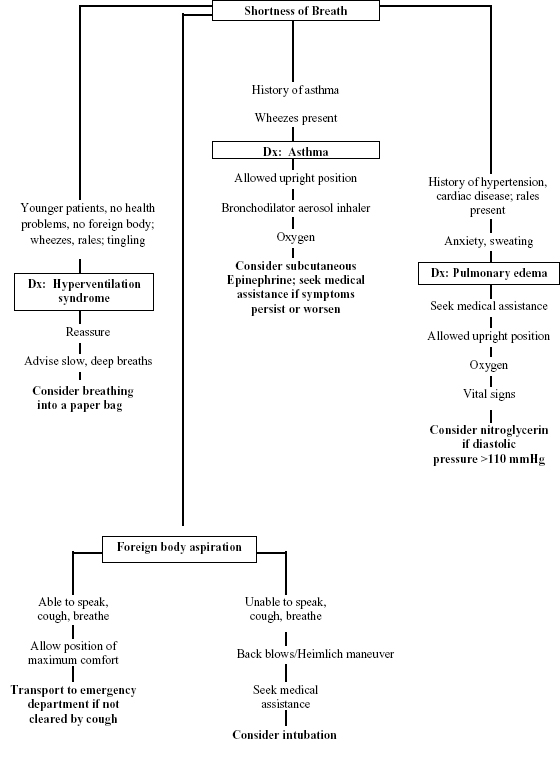
Pulmonary Edema
Pulmonary edema is the accumulation of fluid within the air spaces and parenchyma of the lungs. It generally leads to impaired gas exchange and may cause respiratory failure. It may be due to either the failure of the left ventricle of the heart to adequately evacuate blood from the pulmonary circulation, or from an injury to the lung parenchyma or pulmonary vasculature. There are multiple causes and the treatment is directed at improvement of the symptoms, correcting the etiology of the edema, and avoiding further damage to the lung. Pulmonary edema, especially in the acute setting, can lead to respiratory failure, cardiac arrest due to hypoxia, and death.
Signs and Symptoms
Pulmonary edema is precipitated by high blood pressure, myocardial infarction, arrhythmias, or noncompliance with medications. Manifestations include anxiety, dyspnea, sweating, tachycardia, and cyanosis. Lethargy is an ominous sign.
Treatment
- Medical assistance should be sought.
- The patient should be allowed to assume the position of maximum comfort, commonly upright.
- Oxygen 10 L/minute by oxygen reservoir mask should be administered. Use simple mask or nasal cannula if reservoir mask is unavailable.
- Vital signs should be obtained. Give sublingual nitroglycerin if diastolic blood pressure is above 110 mmHg.
Foreign Body Obstruction
If the Patient Can Speak, Cough, and Breathe
- Do not interfere. Allow the patient to assume the position of maximum comfort.
- If the foreign object is not cleared by coughing, the patient should be transported to an emergency department for further management.
If the Patient Is Unable to Speak, Cough, and Breathe
When managing patients in a dental setting, there are a number of circumstances that can cause an airway obstruction. Over-sedation and the posturing of the patient’s tongue, displaced dentures, cotton gauze, rubber dam, displaced teeth, dental instruments, overzealous irrigation, and even angioneurotic edema may cause some form of airway obstruction. The key to management is prevention through vigilance. Monitor the patient (and the airway) periodically. Keep track of instrumentation and irrigation. Be aware of the patient’s medical history.
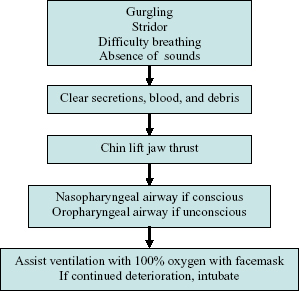
The management of an airway obstruction begins with recognition of the signs and symptoms, which include gurgling, stridor, difficulty breathing, and/or the absence of the sounds of a patent upper airway (Figure 6.4). The oropharynx should be inspected for foreign material and any secretions, and if present they should be removed and the mouth suctioned dry. If foreign material, secretions, or irrigation are not identified, the jaw should be anteriorly repositioned until the anatomic obstruction (tongue) is eliminated. For an unconscious patient, airway assistance with a nasopharyngeal or oropharyngeal airway may provide ventilatory assistance. Supplemental oxygen should be provided. For further deterioration, intubation may be required if it is within the practitioner’s scope of practice.
Figure 6.4. Airway obstruction.
Asthma
Medical History
Obtain a detailed medical history prior to treatment. Try to determine:
- Age of onset
- Precipitating factors (recent respiratory infection, seasonal change, allergies, exercise, pollutants, anxiety, stress, certain medications [salicylates, NSAIDS, cholinergic drugs, beta-adrenergic blockers], certain foods [milk, nuts, shellfish, strawberries, tartrazine food dye])
- In children, the primary type of asthma is allergic or extrinsic asthma which is most often triggered by specific allergens such as pollen, dust, and molds
- Frequency and severity (i.e., mild, moderate, and severe); last attack and its duration and the history of hospitalization (e.g., frequency)
- Current medications and compliance: Medication administration, frequency of oral steroid use, and history of intubation can be used to assess disease severity (Appendix 12-12)
- History of hypersensitivity to aspirin and nonsteroidal anti-inflammatory Drugs (NSAIDS)
- Family history of asthma, allergy, or other atopic disorders
Signs and Symptoms of an Asthma Attack
- Expiratory wheezes and prolonged expiratory phase (expiration normally twice as long as inspiration)
- Shortness of breath, tachypnea (Figure 6.3)
- Pressure on chest
- Nonproductive cough
- Increased respiratory effort (prominent neck muscles, nasal flaring, increased chest and abdominal movement); usually sitting upright, leaning forward
- Rapid pulse
- Apprehension
- Cyanosis (severe cases)
Prophylaxis
- Bronchodilator aerosol inhaler: The patient should bring the inhaler to the dental office and have it accessible to staff. The patient might want to take a puff just before the procedure.
- Oral antiasthmatic medications: The patient should be instructed to take medication as usual, if on a daily dose (Appendix 12, Table A12-1).
- Medications to avoid:
- Aspirin and NSAIDS
- Sedating medications due to depression of the central nervous system and impaired respiratory drive exacerbating respiratory distress during acute asthma attacks
Treatment
When managing the asthmatic in acute distress, it is the bronchospasm that needs to be addressed (Figure 6.5). Yet, it must also be remembered that aspiration of a foreign body or particulate matter can also induce a bronchospasm.
Figure 6.5. Bronchospasm.
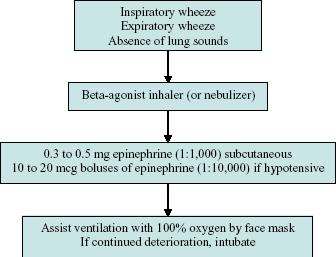
An acute asthma exacerbation or attack will present with respiratory distress and expiratory wheeze. Many asthmatics recognize their symptoms early on and can be of invaluable assistance in managing their own attacks. Immediate bronchodilation with inhaled beta-agonist bronchodilators is the first line of therapy and should result in partial to complete easing of the wheeze and shortness of breath. If there is little to no response to the bronchodilation, medical assistance should be sought urgently as an asthma attack can quickly turn into a life-threatening emergency requiring intubation.
Hyperventilation Syndrome
Hyperventilation syndrome may present as acute respiratory distress with a broad range of associated symptoms such as light-headedness, dizziness, nausea, chest pain, or shortness of breath. Hyperventilation is often associated with extreme anxiety occurring during periods of intense fear or apprehension. Commonly referred to as a “panic attack,” these episodes affect individuals differently. Fear of the dentist, the patient’s perception that he or she is having a heart attack or a “nervous breakdown,” or other worries can all precipitate this type of event. Many patients have symptoms associated with the “fight or flight” response of the sympathetic nervous system such as tachycardia, tachypnea, diaphoresis, dry mouth, dizziness, impaired consciousness, tingling of the extremities, and a variety of other symptoms (Figure 6.6).
Figure 6.6. Hyperventilation syndrome.
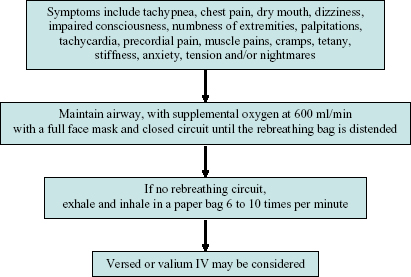
The management of hyperventilation begins with reassurance, with calm maintenance of an airway and provision of supplemental oxygen. Patients can be encouraged to use a rebreathing ventilatory circuit or paper bag to permit carbon dioxide to increase in the blood serum. For the individual who is having an uncontrolled or prolonged anxiety attack, intravenous diazepam or midazolam is helpful, if the administration of intravenous medication is within the practitioner’s scope of practice.
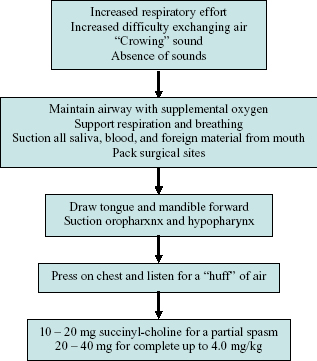
Laryngospasm
During the era that methohexital was the mainstay of ambulatory dental general anesthesia, laryngospasm was an “everyday” event. It still can occur when modern sedative and general anesthetic medications obtund the patient and the laryngeal structures are stimulated by the water used in irrigation, or foreign substances such as a tooth fragments, restorative material, prostheses, or instruments are displaced into the pharynx.
Laryngospasm must be identified rapidly. The practitioner will note increased respiratory effort when air exchange becomes difficult, the presence of high pitched “crowing” sounds if a partial laryngospasm exists, or a total absence of sounds if a complete laryngospasm occurs (Figure 6.7). The airway should be maintained and respirations supported. The mouth and oropharynx should be inspected for foreign substances that should be removed via suction, digital manipulation, or with a McKesson forceps. If the provision of intravenous medication and intubation is within the practitioner’s scope of practice, then succinyl-choline should be administered. If no response is elicited, emergency management is necessary. Emergency medical services (EMS) should be summoned if in an office setting, or a “code” called if in a hospital outpatient or inpatient setting.
Figure 6.7. Laryngospasm.
Cardiac and Vascular Emergencies
Cardiac Emergencies
The subject of cardiac emergencies and their complete management is beyond the scope of this publication. The reader is directed to the American Heart Association’s courses in Emergency Cardiovascular Care for Healthcare providers for a review of the definitive management of these problems. These guidelines are updated periodically and may be revised prior to a revision and reprinting of this book. The intent of this text is to provide dental practitioners with varying levels of training and scope of practice, with a simple, step-by-step, sequential approach to the evaluation and management of cardiac emergencies in order to provide the best outcome for the patient. The perspective taken is for assessment, stabilization, and transport until the appropriate expert can intervene. No matter how extensive the dental practitioner’s scope of practice may be, complex cardiac problems, cardioversion, and the use of complex anti-arrhythmic medications are best managed in an emergency room or inpatient setting, and not in a dental office or hospital dental outpatient facility.
Acute coronary syndrome (ACS) is a term used to refer to a constellation of symptoms caused by occlusion of coronary arteries. These range from angina to myocardial infarction (MI) and can be life-threatening if appropriate management is not begun immediately. All patients with a history of coronary artery disease or risk factors such as diabetes, hypertension, hypercholesterolemia, and smoking should be identified prior to procedures. History of past cardiac events, current medications, and known symptoms help alert the practitioner to any possible risk of an event during the procedure. Signs and symptoms of ACS can include mild to “crushing” chest pain “like an elephant is sitting on my chest,” with or without associated radiation down the left arm, into the jaw, or back; shortness of breath, diaphoresis, and other signs of distress. Diabetic patients and women may present with milder, “atypical” symptoms such as gas or indigestion (Figure 6.8).
Figure 6.8. Evaluation of chest pain.
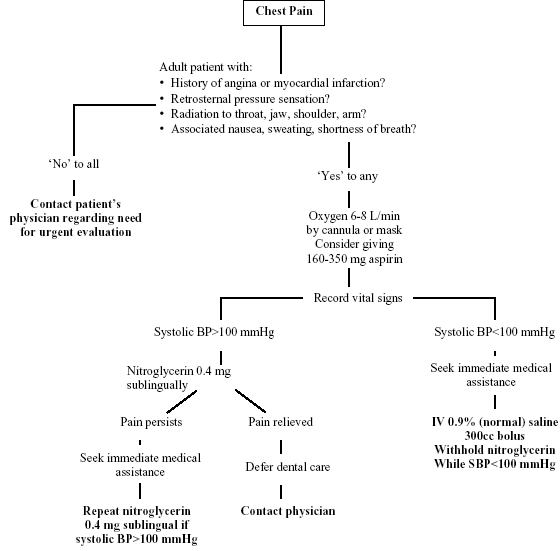
At the onset of any worrisome symptoms, all dental procedures should be terminated and the patient placed in a position that makes him or her feel comfortable. The dental practitioner should begin simple monitoring, assessment, and support for the patient with a sphygmomanometer, pulse oximeter, and/or electrocardiograph if available. Most patients with angina or MI are responsive and able to communicate although they may describe a sense of impending doom and panic. Patients with a history of stable angina can be very knowledgeable about their own symptoms and management and should be encouraged to treat their symptoms as they would at home with sublingual nitroglycerin if they believe this is their typical angina.
Emergency medical services should be summoned if in an office setting, or a “code” called if in a hospital outpatient or inpatient setting for patients with new or atypical symptoms, or those who show any sign of distress. Pulse, respirations, blood pressure, and oxygen saturation are helpful information for the cardiologist and resuscitative team. The airway should be supported, along with breathing and circulation. Oxygen should be provided via nasal cannula. Aspirin, 160 to 325 mg, should be administered orally for the patient to chew and swallow. Nitroglycerin, 0.3 to 0.4 mg, may be provided sublingually or via nasal spray, although this may cause severe hypotension in some MI cases and is best administered in the presence of emergency medical services. If the provision of intravenous medication is within the practitioner’s scope of practice, an intravenous line may be initiated and morphine administered. The practitioner should be prepared to begin basic (or advanced) cardiac life support at any time.
For patients with suspected ACS who become unresponsive, the principals and practices taught in basic or advanced cardiac life support should be initiated. All dental procedures should be discontinued. Emergency medical services should be summoned if in an office setting, or a “code” called if in a hospital outpatient or inpatient setting. Again, the material contained within this chapter is not intended to supplant such courses, but to put management of these problems into perspective when they occur in the dental setting. As such, these are considered “witnessed arrests” and more than one provider will be presumed to be present.
The patient should be placed on a back board or on the floor and pulse checked. If no pulse is present, chest compressions should begin with 30 compressions and two breaths for adults, or 15 compressions and two breaths for children (two rescuers are presumed to be present). After the initial compressions, the airway should be opened and breaths provided. If the patient is breathing, her or she may be placed on his or her side in a recovery position. If not, cardiopulmonary resuscitation (CPR) should resume with compressions (C) at a rate of at least 100 per minute, airway (A) maintained, and breathing (B) continued at a rate of eight to 10 breaths per minute. The rescuers should rotate every two minutes. If an automated electronic defibrillator (AED) arrives, the CPR should be continued until the AED is in position to be used, rhythm checked, and shock delivered if appropriate. CPR should be resumed and a rhythm checked every two minutes.
For practitioners who have taken Advanced cardiac life support education, whose education, training, and scope of practice permit, and whose facility is appropriately equipped, the next level of care may be provided. This includes but is not limited to the provision of intravenous (or intra-osseous) fluids, intravenous (or intra-osseous) medications, and endotracheal intubation or surgical airway access. Reversible causes for the cardiac event should be explored, including hypovolemia, hypoxia, hydrogen ion (acidosis), hypo/hyperkalemia, hypothermia, tension pneumothorax, cardiac tamponade, pulmonary thrombosis, coronary thrombosis, and medication toxicity. The patient should be routinely reassessed and administered CPR as necessary throughout. In all cases, administration of intravenous medications, endotracheal intubation, cardioversion, and the use of complex anti-arrhythmic medications are best managed in an intensive cardiac care setting, and not in a dental office or hospital dental outpatient facility. Assessment, stabilization, and transport to such a facility are appropriate responsibilities for the dental practitioner.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


