6
Hypersensitivity Reactions
To be honest, the world is full of spies and traitors. We know this sounds awfully paranoid, but really, as scientific people, we have to face reality. If you don t believe us now, that’s understandable, because frankly you haven’t read this chapter yet. If you don’t believe us at the end of this chapter, then you clearly did not understand anything you read here. What we want you to understand is that just when you think your defense line is secure and that peace is upon the land, the spies give away the secrets, the walls are weakened, and even your most trusted assistant is seen hanging around some sleazy nightclub (sure sign of a traitor!). Headquarters has given a code name to the covert, backstabbing process so that we can talk about it and baffle the enemy (who are probably listening in and reading this material over your shoulder right now . . . go ahead, look around and check!). The code name we use is “hypersensitivity.” Remember, when we use that word we are talking about TRAITORS!
Hypersensitivity represents an immune reaction that produces injury to the tissues of the host. It is involved in many forms of human disease.
Hypersensitivity may be classified into Types I, II, III, and IV. Types I to III are immediate responses that are mediated by antibody, while Type IV, or delayed-type hypersensitivity, is a delayed response that is mediated by T cells.
Type I
Immediate-type hypersensitivity
We will consider two means by which exposure to a foreign substance can result in anaphylactic hypersensitivity. One reaction involves an IgE-antibody response, while in the other, activation of the complement cascade by immune complexes results in the formation of anaphylatoxins.
In the first type of reaction there is binding of the Fc piece of IgE to the membrane of target cells. In humans, these are chiefly mast cells and basophils. There are two stages in anaphylaxis (several more were reported in Abilene, but they have since pulled out of town):
Stage 1. The individual is exposed to antigen for the first time, and this results in the production of homocytotropic antibodies (IgE and IgG1). These antibodies can bind to the surface of target cells via the Fc region, thus leaving the antigen combining site free to react with antigen. The cells are now sensitized.
Stage 2. The second exposure results in an antibody-antigen reaction at the surface of the sensitized cells. This triggers the release of mediators via degranulation of the mast cell or basophil.
Degranulation is initiated by antigens (allergens) bridging two cell-bound IgE molecules (Fig 6-1). This causes the target cell to release chemical mediators, such as (you guessed it!) histamine, PGD2, LTC4, LTD4, LTE4, eosinophil chemotactic factor of anaphylaxis, and platelet activating factor (PAF).
The actual release mechanism seems to be regulated by intracellular levels of cyclic AMP and cyclic GMP. A rise in cyclic AMP is associated with an inhibition of release, whereas cyclic GMP has an enhancing effect.
Drugs that modulate cyclic AMP are used in the treatment of anaphylactic reactions. These include epinephrine and theophylline.
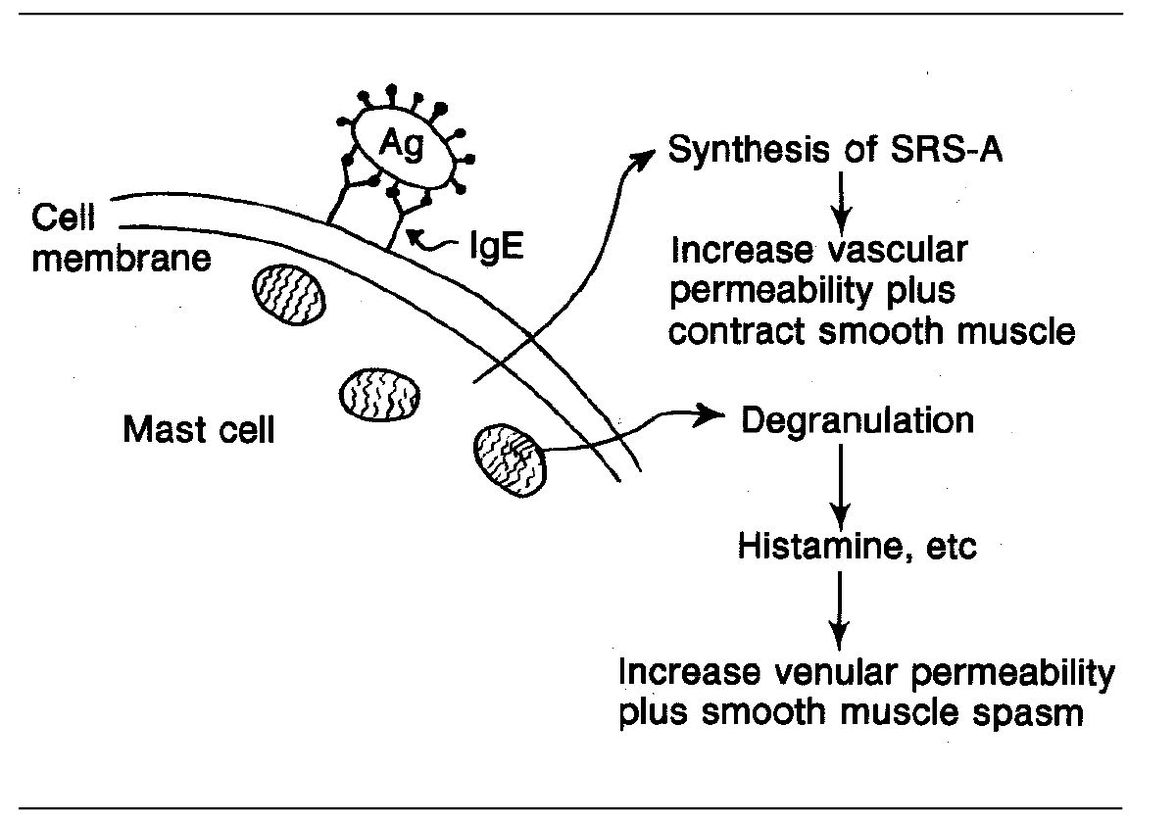
Fig 6-1 Anaphylactic reaction. (Ag) Antigen.
In complement-mediated anaphylaxis, complement fragments C3a and C5a (the anaphylatoxins) can trigger the release of mediators from mast cells and basophils directly.
The following allergens are most likely to produce anaphylaxis: pollens, grasses, weeds, drugs, dust (and mites), dander, molds (aspergillus), food (nuts, milk, berries, fish, etc), and insect stings.
The reactions are determined by the site at which antigen is introduced.
- In the skin, the local reaction is urticaria (hives).
- In the upper respiratory system the reaction produces hay fever.
- In the lungs the reaction causes bronchospasm (asthma) due to smooth muscle contraction.
- In the GI tract Type I hypersensitivity produces diarrhea and vomiting due to increased peristalsis.
- Anaphylaxis is a generalized allergic reaction characterized by hypotension and shock resulting from vasodilation and increased vascular permeability. The majority of deaths are due to respiratory complications (dyspnea, lower airway obstruction, laryngeal edema). The skin and GI tract are often affected as well.
Type II
Immune cytotoxic reactions
Type II hypersensitivity involves reactions between IgG or IgM antibodies and antigen that is bound to cells or tissues. The reaction results in the destruction of the cell or tissue by one of three mechanisms:
- Complement-dependent cell lysis (Fig 6-2). Circulating complement-fixing antibodies (IgM, IgG) react with antigen situated on the membrane of a cell (eg, a foreign red blood cell, the cells of an organ transplant, or an individual s own platelets, as occurs in autoimmune thrombocytopenia, etc). Activation of complement in this reaction results in generation of C5b–C9, the membrane attack complex (MAC) of the complement system. (Do you remember the “biologic effect” of C8 and C9? The effect is cell lysis.)
- Phagocytosis and destruction of antigen-bearing cells by phagocytes (neutrophils, macrophages) that have C3b or Fc receptors.
- Cytotoxic reactions may occur without complement activation. In this situation, NK cells with Fc receptors bind to cell-bound antibody via the Fc portion of the antibody (Fig 6-3). This may lead to extracellular killing (lysis) of the cell. The latter is known as antibody-dependent, cell-mediated cytotoxicity (ADCC).
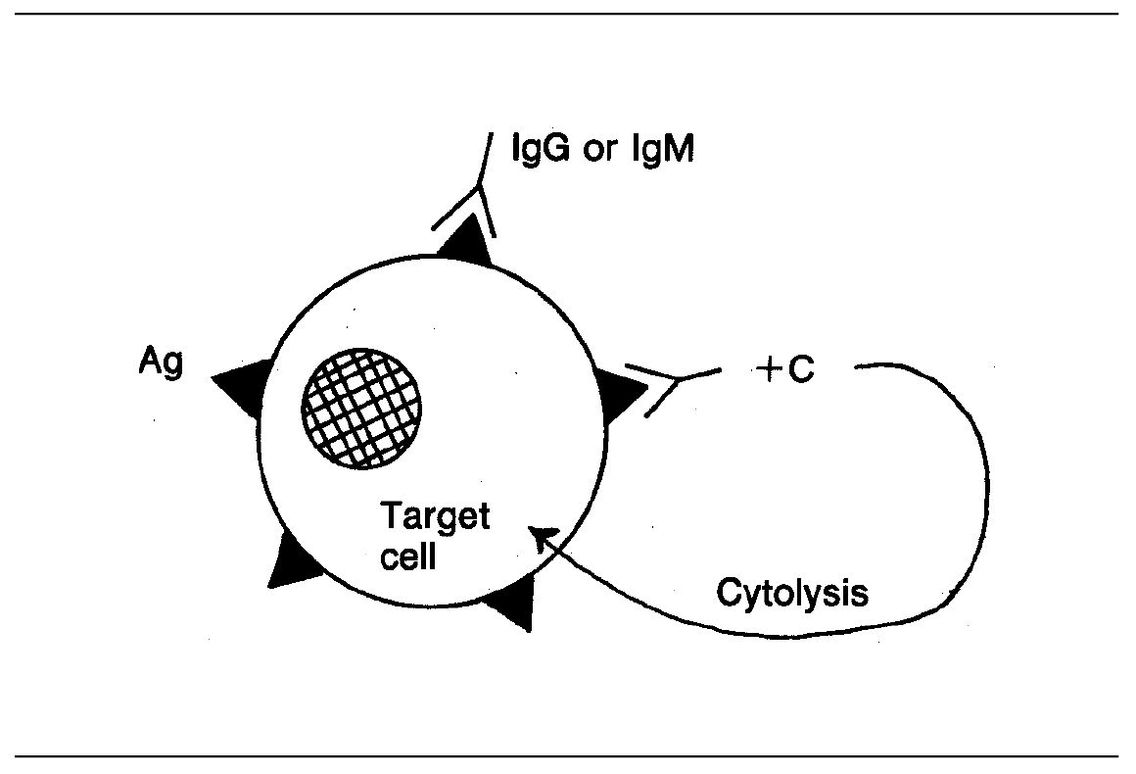
Fig 6-2 Complement-mediated cytolysis. (Ag) Antigen.
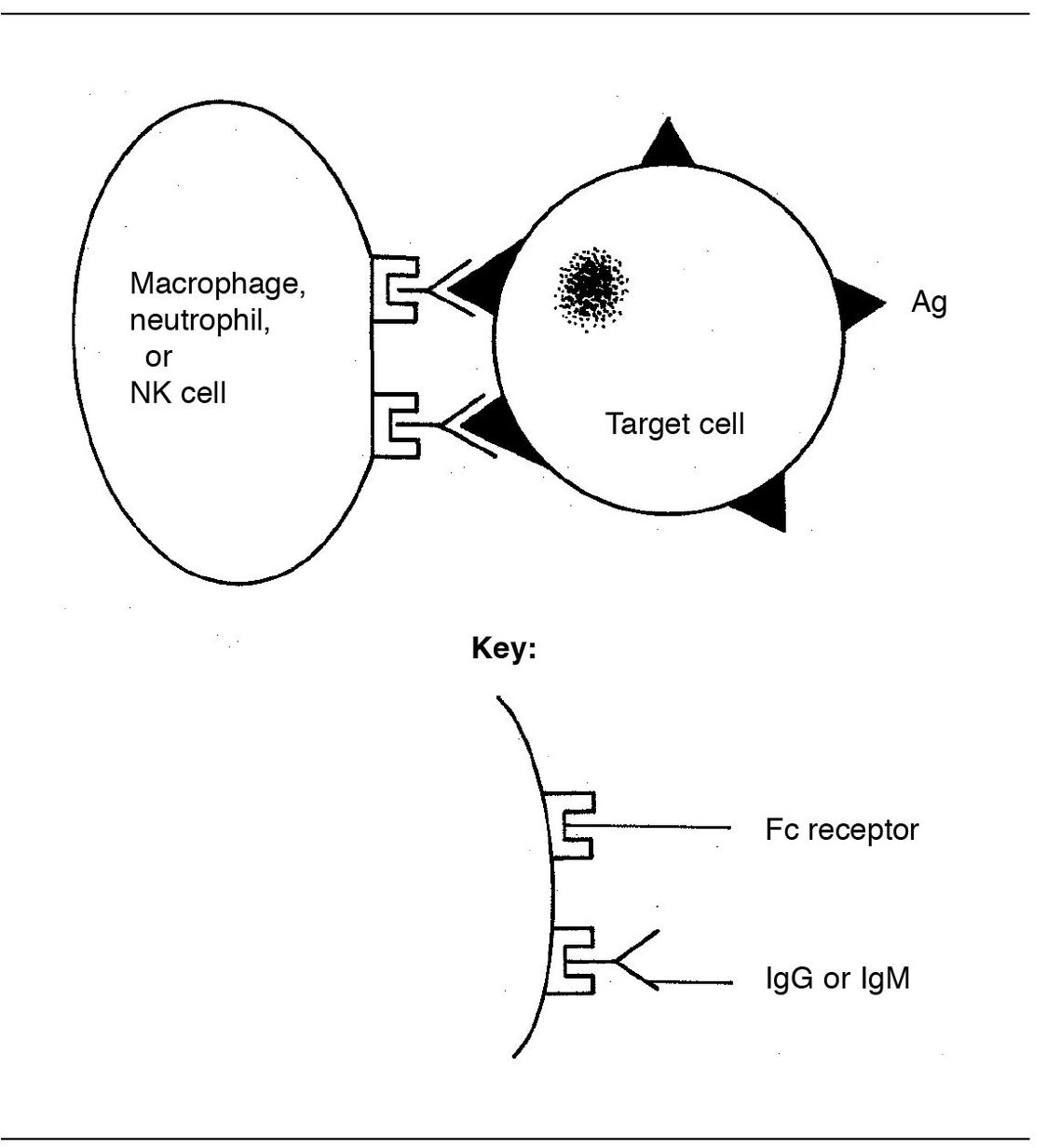
Fig 6-3 Antibody-dependent, cell-mediated cytotoxicity (ADCC). (Ag) Antigen.
Cytotoxic phenomena are involved in conditions such as autoimmune hemolytic anemia, some organ transplant rejections, and idiopathic thrombocytopenic purpura (destruction of blood platelets). Glomerular basement membrane can also be attacked (Goodpasture s syndrome).
In erythroblastosis fetalis, an Rh-negative mother is sensitized by red cells from an Rh-positive baby. Maternal antibodies (IgG) cross the placenta and destroy the baby s Rh-positive fetal red cells. This produces anemia and jaundice (due to the release of hemoglobin, which is converted to bilirubin).
Type III
Immune complex hypersensitivity
This is similar to Type II hypersensitivity in that it involves circulating complement-fixing antibodies (IgG or IgM), and activation of the complement system plays a role in initiating the response. Repeated exposure to the same antigen produces high levels of antibody in the serum. These antibodies bind to antigen molecules, resulting in the formation of immune complexes.
There are two types of immune complex–mediated injury, one associated with precipitation of large antigen-antibody complexes (the Arthus-type reaction), the other associated with soluble antigens (not bound to cells or tissues) that are in the circulation or tissue spaces (serum sickness–type reaction).
In the Arthus-type reaction the large immune complexes are deposited within blood vessels where they activate complement. Immune complexes are likely to become localized in blood vessels where there is branching, turbulence, or the presence of fenestrations.
Here’s what happens when the complement system is activated :
Chemotactic factor (C5a) attracts neutrophils that release their lysosomal enzymes, causing tissue damage. Since these reactions often occur within blood vessels, tissue damage generally includes vasculitis. Anaphylatoxins are generated, resulting in increased vascular permeability and edema.
The most common sites of immune complex deposition are the kidneys, heart, small blood vessels, and skin.
The Arthus reaction is the classic experimental model of localized immune precipitate–triggered injury. The stage is set for this reaction when a high serum titre of complement-fixing antibodies has been produced in an animal by repeated administration of an appropriate antigen, such as serum albumin.
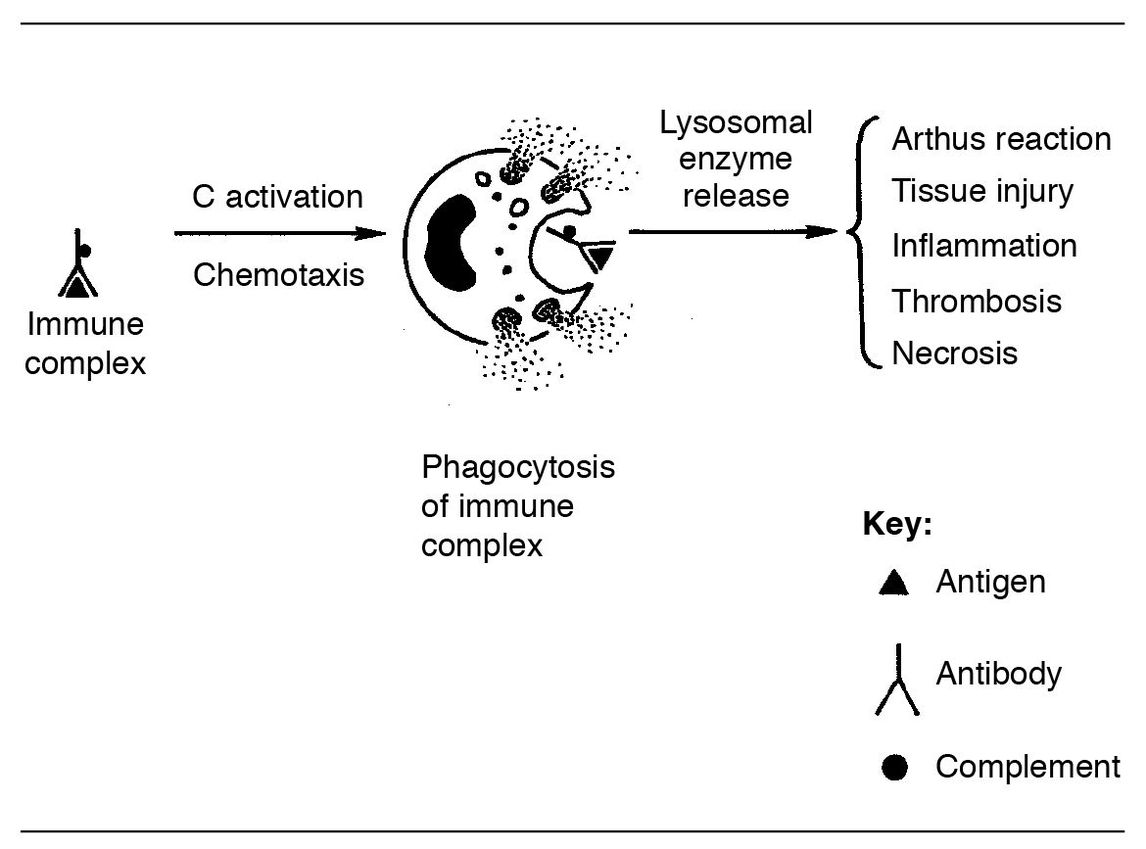
Fig 6-4 Arthus reaction.
The local Arthus reaction can be produced by local administration of the antigen, or, if the antigen is given intravenously, a systemic Arthus reaction can be induced. In either case, antigen unites with the antibody, and complement is activated within the vessels. Neutrophils are attracted chemotactically; they phagocytize the immune complexes, degranulate, and release their lysosomal enzymes.
These enzymes destroy the walls of blood vessels. As a result, platelets adhere, aggregate, degranulate, and attract more platelets. This leads to the formation of occlusive thrombi, and hemorrhage and ischemic necrosis ensue.
Figure 6-4 will help to explain the Arthus reaction. You can see that antigen unites with antibody, and complement is activated. Chemoattractants attract neutrophils, and they phagocytize the immune complex. This causes lysosomal enzyme release with its resultant host injury.
Antigens that are commonly associated with immune complex hypersensitivity include drugs and serum (serum sick/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


