6
Esthetic implant treatment
The demand for beauty and smile enhancement through cosmetic restoration or esthetic implant restoration continues to increase in our modern society. However, in the area of the smile, it is challenging and difficult to achieve highly esthetic results using implants. It is easy to understand that the patient’s tooth is still the best implant. Therefore, in order to become the treatment of choice, implant restoration has to offer a more natural look, beyond the results of conventional prostheses.
A modern concept of implantology should be based on predictable osseointegration associated with the harmonious integration of soft tissues. Osseointegration is attained if the basic surgical implant principles are respected, but esthetic predictability in the anterior zone is a different issue, and is more challenging to achieve, for a variety of reasons:
- Anatomical and biological considerations, and the patient’s immune potential.
- The patient’s local and general parameters, and any aggravating risk factors.
- Choices between invasive or less invasive surgical approaches.
- The clinician’s high degree of responsibility toward the demanding and well-informed patient!
- The patient’s high expectations with regard to the clinician’s dexterity and expertise!
- Scientific, clinical, and technological progress.
The objective of any esthetic implant treatment is to ensure that the restoration has a pleasant aspect and that the alignment of the soft tissue is correct.
Osseointegration, one of the most important revolutions in dentistry, represents a real answer to the patient’s needs, by offering a solution for total, partial, or single edentation. Implant protocols for the replacement of missing anterior teeth or compromised ridges have evolved considerably and modern approaches are much less invasive. But a predictably beautiful result is difficult to obtain using implants and more challenging to achieve in the anterior zone.
Replacing a single tooth in the esthetic zone with an implant restoration is one of the most demanding tasks in implantology. Therefore, the anterior region represents the most critical area from an esthetic standpoint and the most complex one with regard to the osseous and gingival architecture.
The anterior sector always becomes even more esthetically challenging during the replacement of a central incisor, because of the presence of the contralateral tooth and the adjacent teeth; thus the gingival tissues will serve as references for the volume, position, color, texture, marginal contour and interdental papillae, and so on at the end of the treatment (Touati, 2011).
Replacing a maxillary anterior tooth with an implant becomes extremely challenging in patients with a high smile line or gingival recession (Figs 6.1a, b). Therefore, implant placement in the anterior esthetic zone can be esthetically risky.
Figure 6.1 (a) A gingival smile, with an excess of gingiva on the lateral side. (b) Multiple Class I/II gingival recession.


In the area of the smile, immediate implantation after an extraction, or delayed implantation in a healed site with a thin biotype, generally also represents a great clinical challenge (Saadoun, 2010).
When a single central incisor is to be replaced by an implant crown without accompanying restoration of the adjacent teeth, the esthetic risk is even greater, as no compromises are acceptable with regard to the restoration and the surrounding gingiva (Goldstein et al., 2010).
The esthetic difficulties involved in implant dentistry are managing the soft tissue, and mimicking the natural appearance of the patient’s teeth and gingiva. Indeed, achieving the ultimate esthetic results in the anterior zone with implant restoration should be similar to achieving esthetic results with conventional restorative dentistry.
Radiography, cone beam, and CT scanning allow the clinician to evaluate the complexity of the case. It is imperative to assess the osseous and gingival states with precision before any treatment, since this information will guide the clinician in determining the best time for implant placement (immediate or delayed) as well as the type of temporization.
The presence of a thick cortical bone is one of the prerequisites for obtaining an adequate gingival profile. The use of biomaterial will give the best result, as long as it is combined with an immediate implant placement, allowing the clinician to correctly maintain the initial volume of the alveolar socket. When it comes to bone loss, there is no difference between immediate and delayed implant placement.
An esthetic gingival contour includes a harmoniously scalloped gingival line, the avoidance of abrupt vertical differences in clinical crown lengths between adjacent teeth, a convex buccal mucosa of sufficient thickness, and distinct papillae (Ahmad, 1998).
Esthetic success can really be predictable only through the development of a comprehensive treatment approach and a proper understanding of the biological parameters that can influence the esthetic outcome at the dental/implant restoration interface (Van Dooren, 2000).
For all of the surgical and/or prosthetic steps to culminate in a predictable esthetic result, there is an optimal treatment time, which is necessarily proportionate to the complexity of the case and the chosen treatment modality (Zuhr, 2011).
Peri-implant risk factors
With an increase in the average lifespan and a higher esthetic demand from older patients, a multidisciplinary approach enables the clinician to control facial and periodontal damage induced by tissue aging, combined with ongoing or aggressive periodontitis.
Our role is to diagnose what damage is caused by bacterial aggression on the periodontium and what is due to the normal aging of the dental and periodontal structures in these patients.
There is a consensus on the etiologic diagnosis of periodontal diseases. The infection cycle will only take place when four conditions are satisfied (Socransky and Haffajee, 1992):
- virulent bacteria are present
- saprophytic bacteria are absent
- the environment is favorable to the colonization of virulent bacteria (thin versus thick biotype), and
- the immune system does not react normally because of very bad habits (smoking or alcoholism) or an acquired deficiency (such as diabetes) or immune deficiency (such as AIDS).
The classic treatment of periodontal disease requires precise chronological therapy. The teaching of oral hygiene is an indispensable and essential step in the therapy prior to implant placement. Training patients to modify their bad dental habits, or their consumption of tobacco and alcohol, is part of a comprehensive approach to the treatment of the “patient” and not just the “disease”. Nonsurgical therapy is the starting point of any periodontal treatment. The physicochemical disinfection of the teeth and the oral cavity is a prerequisite for the initial therapy.
Antiseptics such as chlorhexidine mouthwash must be prescribed before and after scaling and root planing. This initial treatment step alone solves the problem in the majority of cases.
In a recent study by Elter et al. (2008), the adhesion of bacterial plaque on implant supragingival areas was significantly higher than in subgingival areas. The accumulation of biofilm in supragingival areas increased significantly on rough surfaces, whereas this influence was not detected in subgingival areas. Consequently, there was a significant influence of surface localization (supra- and subgingival) as well as surface modification on biofilm.
Surgical treatment, in the form of flaps with or without osseous surgery, combined with bone grafts, is necessary if the periodontal pockets are deep. This is a prerequisite for all other tissue regeneration techniques and root coverage (Dersot, 2011).
The procedures for periodontal surgery on natural teeth are much less challenging than implant surgery because of the differences between the tooth and implant surfaces. The maintenance phase is indispensable in evaluating the risks for recurring loss of attachment, especially when the patient has a family history of severe periodontitis and is a heavy smoker.
A prospective study over 5–15 years (Kehl et al., 2011), performed with sophisticated CT scanning on loaded implants placed on partially edentulous patients treated for chronic periodontitis (CP) or generalized aggressive periodontitis (GAP), has shown more significant buccal bone resorption on generalized aggressive periodontitis patients (2.3 mm) than on chronic periodontitis patients (1.75 mm). This study has also shown a significant thickness of keratinized gingiva in the mandible of the generalized aggressive periodontitis patient (1.12 mm) in comparison with the chronic periodontitis patient (0.85 mm). This decrease in gingival thickness is significantly correlated with the increase in bone resorption in the generalized aggressive periodontitis patient relative to the chronic periodontitis patient. The importance of the thickness of keratinized gingiva as the behavior of the bone resorption around the implant varies, according to the type of periodontal disease, is a new parameter that is becoming increasingly evident.
The logic of active periodontal treatment today, to be performed before any implant treatment, is to eliminate all etiologic, biological, and iatrogenic factors. An increasing number of scientific articles suggest that there is a tendency for smokers to have a higher number of pathogenic bacteria than nonsmokers, without an increase in the quantity of bacterial plaque (Figs 6.2a, b). This hypothesis confirms that tobacco has a harmful effect not on the subgingival environment, but primarily on the immune response (Nato, 2010).
The majority of publications agree that tobacco constitutes a major risk factor for periodontal disease. The link between smoking and calculus has not yet been clearly established. However, smoking is associated with higher susceptibility to periodontal disease and it induces a higher level of, and more rapid, bone destruction, with angular defects. Bone loss is increased by a factor of 2.3 among moderate smokers (ten cigarettes per day) and a factor of 5.3 among heavy smokers (17 cigarettes per day).
Figure 6.2 (a) The patient’s teeth, full of calculus and heavy nicotine staining. (b) The same patient after periodontal dental prophylaxis. (c) A diabetic patient checking her blood sugar, using medication in tablet and injection form.



Tobacco significantly reduces the benefits of nonsurgical and surgical periodontal therapy in terms of attachment gain, periodontal pocket reduction, bone gain, and root coverage. Augmenting the risk of failure in surgery, tobacco could become a major contraindication and obstacle to any surgical implant treatment. There is a consumption-related effect among these risk factors: the higher the consumption, the higher the risks (Nguyen, 2010).
It appears that the habit of tobacco smoking has a negative influence on periodontal healing. Even though its action mechanism is not totally understood, it has been shown that there is a link between smoking habits and factors such as systemic vasoconstriction, decrease in blood flow, polymorphonuclear leukocyte blood cell dysfunction, lymphocyte deficiency in the immune system, and inhibition in fibroblast proliferation and/or function. All these negative factors can be reversed if the patient stops smoking (Nato, 2010).
Are systemic factors affecting implant survival?
The various studies do not qualify the role of diabetes and smoking in implant failure, but together they support our continuing need to question the influence of systemic factors on implant survival in view of the possible complications and potential benefits that implant therapy may offer (Fig. 6.2c). Therefore, the benefit of implant therapy may be denied to some patients because of systemic conditions, which should be evaluated against the risk and our level of understanding of those risks. All of the systemic conditions should be under control before implant therapy is undertaken, to prevent any risk (Oates, 2011).
Selected personality traits may be used to predict patients’ satisfaction with implant-supported prostheses prior to treatment, and may also provide valuable information for the prediction of a satisfactory outcome before implant treatment is started – which could save time and money if the prediction is unfavorable. Dentists could be more cautious when faced with the possibility of patients’ rejection or dissatisfaction, before carefully deciding whether to opt for expensive and time-consuming treatment, or to modify the treatment plan in favor of a more reversible or less expensive one (Al-Omiri et al., 2011).
Table 6.1 Local implant risk factors
| Parameters | Favorable factors | Unfavorable factors |
| The level of the FGM | Identical, or more coronal to the margin of the adjacent teeth | More apical than the GM of the adjacent teeth |
| The periodontal biotype | Thick and flat; rectangular-shaped teeth | Thin and scalloped; triangular-shaped teeth |
| Proximal bone sounding of the adjacent teeth of the implant | The presence of bone at a 3 mm distance from the buccal side, and a maximum of 4.5 mm from the proximal side | Bone architecture with more than 3 mm on the buccal side, and more than 4.5 mm on the proximal side |
| The location of the tooth/implant restoration contact point | Less than 4.5 mm to the bone peak, and less than 3.5 mm between two implants | More than 5 mm to the bone peak, and more than 3.5 mm between two implants |
| The mesiodistal length of the edentulous crest | Enough bone space (1.5–2.0 mm) between the implant and the natural teeth, and a minimum of 3 mm between two implants | Less than 1.5 mm space between the natural teeth and the adjacent implant, or less than 3 mm between two implants |
| The bucco-palatal width of the edentulous crest | More than 6 mm, leaving > 2 mm of buccal bone from the implant | Less than 6 mm, leaving < 1 mm of buccal bone from the implant |
| The timing of the procedure | Immediate implant placement within a short time following the extraction; < day 0 to 8 weeks | Delayed implant placement: > 8 weeks |
| The surgical technique | No flap or incision, hence preserving the papilla | An incision affecting the papilla |
| Temporization | More than 6 months: stability of the peri-implant HST | Less than 4 months: recession of the peri-implant HST |
GM, gingival margin; FGM, free gingival margin; HST, hard and soft tissue.
All peri-implant procedures should respect the basic principles of periodontal surgery, taking into account the difference between the two entities – teeth and implants – and the role of local, general, and psychological risk factors, as described in Table 6.1.
The implant/mucosa interface differs in composition and measurement (Glauser et al., 2005), depending on whether the interface is with the implant’s machined surface (3.19 mm), the implant’s rough surface (2.40 mm), or the natural teeth (2.11 mm) (see Figs 4.29d–f), and these differences are important in understanding the susceptibility of implants to infection (Listgarten et al., 1991). The supracrestal collagen fibers are oriented in a parallel rather than a perpendicular configuration (Abrahamsson et al., 1997; Schupbach and Glauser, 2007). This creates a much weaker mechanical attachment compared to natural teeth. In addition, the ability of the peri-implant mucosa to regenerate itself is limited by its compromised number of cells and poor vascularity (Lindhe and Berglundh, 2000). Therefore, peri-implant and periodontal tissues may differ in their resistance to bacterial infection (Lindhe et al., 1992; Ericsson et al., 2000).
Soft tissue management
An optimal gingival frame surrounding implant-supported restorations is important in completing the illusion of natural teeth in the esthetic zone (Fig. 6.3a). The soft tissue framework (PES) plays a critical role in the visual perception of any anterior implant restoration (WES) (Fig. 6.3b). Without a pleasing gingival framework, even the most skilled restorative dentist and ceramist cannot predictably deliver an esthetically pleasing result (Leziy and Miller, 2008b); but without an implant restoration that respects and reproduces the optimal harmonious natural tooth gingival contour (Fig. 6.3c), it is also impossible to achieve an esthetic outcome (Saadoun, 2008).
Figure 6.3 (a) Natural teeth with optimal proportions and a harmonious gingival contour. (b) The optimal esthetic result on the left central incisor implant restoration, with a harmonious gingival contour (with respect to the gingival zenith enamel deformity). (c) An unpleasant esthetic result on the two adjacent implant restorations (the zenith of the gingival margin is on the mesial instead of on the distal), with a disharmonious gingival contour on the central/lateral incisor restoration.

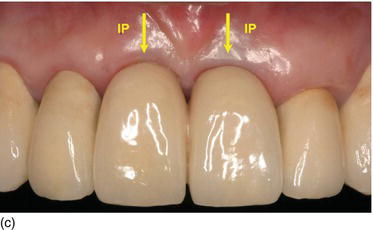
Therefore, the functional and esthetic success of implant treatment in the anterior zone depends not only on the quality of the restoration, but on preserving or regenerating the favorable hard and soft tissue architecture, and mainly on the final and long-term aspects of the contour and stability of the marginal gingival and proximal papillae, in harmony with the adjacent teeth (Rompen et al., 2003; Saadoun, 2010).
Around natural teeth, the techniques of plastic periodontal surgery allow a harmonization of the gingival contour and coverage of gingival recession while respecting the cosmetic quality of the tissue with regard to thickness, texture, and color. This is made possible through the use of lateral pedicle flaps or gingival grafts and, in particular, connective tissue grafts. The surgical protocol varies for partial or total coverage of the graft under an envelope, a tunnel, or a pedicle flap moved coronally or laterally.
In peri-implant cases, these plastic surgery procedures vary greatly according to the clinical situation: replacement of single or multiple implants, the morphology of the edentulous crest, the quality of the implant system, the biocompatibility of the material, and so on. Therefore, a robust general knowledge of plastic surgery is a prerequisite. Even though the savoir-faire with regard to teeth can also be applied to implants, it is not always sufficient for the recreation of an ideal gingival margin contour and interproximal papillae.
The facial tissue height and contour are important anatomical features for an esthetic restorative result, the other being bone levels at adjacent teeth, as already pointed out (Choquet et al., 2001; Ryser et al., 2005). The height and thickness of the facial bone wall determine the position of the midfacial mucosal margin and the contour of the alveolar ridge (Buser et al., 2004; Grunder et al., 2005).
Peri-implant soft tissues are more fragile and more delicate to manipulate, and even unpredictable during the healing phases, because they are inevitably traumatized due to the loss of the tooth and the several surgical sessions required to replace it with an implant that is integrated well into the hard and soft tissues. The more traumatized the implant site is, the more the potential for natural healing decreases. This limits the esthetic result, increases the frustration of the clinician, and leads to patient disappointment (Romagna, 2009).
It is a challenging task to achieve acceptable gingival esthetics around single anterior implants. Maintaining such an implant esthetic over time can be equally demanding, especially if the teeth that had to be extracted showed gingival recession initially and/or the absence of attached keratinized gingiva.
In the esthetic zone, the morphology of the soft tissues plays a central role in the achievement of satisfactory final results (Covani et al., 2007). The apical zenith of the facial gingival outline is located slightly distal to the mid-axis of the maxillary incisor. Although an implant-supported central incisor crown may closely duplicate the adjacent teeth, if the free gingival margins do not match, visual disharmony will ensue and the illusion will be lost (Kinsel and Capoferri, 2008).
The soft tissue framework plays a critical role in the visual perception of any anterior implant restoration. Therefore, it is necessary that an implant restoration respects and reproduces the optimal harmonious natural tooth gingival contour, to achieve an esthetic outcome. It is then equally important to create harmony between the restoration and the remaining dentition and soft tissue framework (Saadoun, 2008; Tucker, 2009).
Thus, during treatment, a considerable amount of effort is focused on enhancing the balance of the pink and white esthetics, using a combination of surgical and restorative treatments (see Fig 6.3b). It is usually easy to create such a balance, as long as the various stages of treatment are appropriately timed (Leziy and Miller, 2009).
The optimal esthetics can be maintained when the various components of the tissue are in a physiological relation and work in harmony. Therefore, if this relation is not biologically correct, an esthetically pleasing result will not be achieved (Salama and Jundslalys, 2003).
The risk of marginal tissue recession is more predictable with thin marginal mucosa in implantology than in periodontics. The objective of connective tissue grafting is to obtain a thicker zone of keratinized soft tissue, regain attachment to the tooth, and cover the radicular surface to restore the esthetics and eliminate hypersensitivity. This soft tissue thickening in implantology augments the tissue biotype, preventing peri-implant soft tissue recession, and allows for a more stable and predictable tissue level after tooth extraction, at the time of abutment placement and the taking of impressions, and after the temporary and final restoration.
It must be considered that when something is lost or removed, there is always a biological consequence. This often means that a soft and hard tissue deficiency will develop following the loss of a tooth (Leziy and Miller, 2007).
Furthermore, following tooth extraction, the osseous and gingival tissues are often altered, with horizontal and/or vertical loss, and the implant site is often insufficient for ideal implant placement. Some forms of socket preservation or augmentation invariably become necessary to treat horizontal and/or vertical deformation (see Table 4.6).
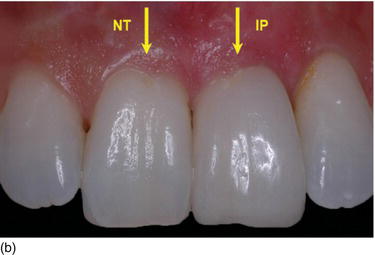
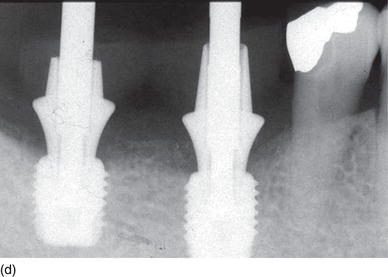
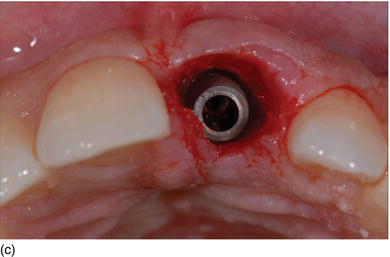
In the majority of machine submerged implants (Figs 6.4a), approximately 0.9–1.6 mm of crestal bone is lost in the first year of functioning after abutment connection and/or restoration, with the crestal bone being located at the first thread of the implant below the “microgap”; that is, the connection between the implant body and the prosthetic abutment. Moreover, the peri-implant soft tissue recession is 0.7–1.0 mm (Saadoun, 1997; Grunder, 2000; Small and Tarnow, 2000; Small et al., 2001).
This ongoing gingival recession remains a reality today. It reveals the fragility of the peri-implant structure (bone and soft tissue), and it also creates an esthetic prejudice without jeopardizing the functional aspect of the restoration (Cardaropoli et al., 2006; Kan et al., 2007; Saadoun and Touati, 2007; Evans and Chen, 2008).
A wide range of factors are known to have a deleterious effect on crestal bone resorption (Figs 6.4b–d) and affect early crestal bone loss in the majority of endosseous dental implants (Koszegi Stoianov, 2010):
Figure 6.4 (a) The majority of submerged implants lose 0.9–1.6 mm of crestal bone after implant/abutment connection in the first year of functioning.
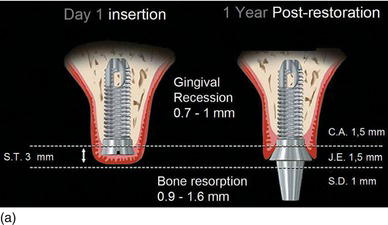
Figure 6.4 (b) The alveolar socket after premolar and molar extraction. (c) Immediate implants placement with healing abutments. (d) Switch platform prosthetic abutments were able to maintain the crestal bone at the top of the Mega-Gen implant platform. (Courtesy of Dr. K.B. Park, Seoul, S. Korea.)


- surgical and anatomical considerations
- the amount of keratinized gingiva
- the design of the mucoperiosteal flap
- bone quality and/or density
- an implant design with a divergent collar
- trauma during the surgical procedure
- the thickness of the buccal and lingual cortical plates of the bone remaining after osteotomy
- the healing process in the submerged or nonsubmerged implant protocol
- exposure of the implant during healing of the soft tissue
- the level of the microgap connection in relation to the bone crest
- the tooth–implant or inter-implant horizontal distance
- the establishment of the implant’s “biological width”
- the lack of a soft tissue seal in the peri-implant mucosa
- the use of an abutment with a diameter equal to or less than that of the implant body
- the repeated removal and replacement of the abutment, with disruption of the soft tissue seal
- preloading and loading restorative phases with a functional occlusion
- excessive occlusal forces due to parafunctional occlusion, and
- the patient’s oral hygiene, and local and systemic aggravating factors.
It is evident that full control of all the variables that play a role in bone loss around implants after implantation, especially around the implant crest module during the first year of implantation, is beyond any clinician’s domain, given the biological (patient), human technical (clinician), and engineering (implant divergent collar design and connections) aspects that contribute to this complex problem (Marincola et al., 2009).
Human implant histology over a 3-year period has shown that the apical migration of the implant junctional epithelium (JE) is halted by the attachment of the connective supracrestal fibers to the Laser-Lok® microchannel collar surface and hence resorption of cervical bone is prevented (Nevins et al., 2008). The supracrestal position of the implant’s Laser-Lok® collar limits the apical migration of the junctional epithelium, allows the attachment of perpendicular connective fibers, and prevents crestal bone loss.
The analysis of 49 implants in a recent study by Shapoff et al. (2010) showed a mean crestal bone loss of 0.44 mm at 2 years postrestoration, and 0.46 mm at 3 years. All bone loss was contained within the height of the collar, and no bone loss was evident at the level of the implant threads.
Literature reviews on the topic of peri-implant recession over the past 5 years have proven that bone resorption has been limited to an average of 0.46 mm following the evolution of:
- precise diagnosis, with less invasive surgery
- improved implant design – with regard to the body, surface, collar and diameter, and microthreads, and
- precise abutment/crown restoration connection (Zadeh, pers. comm., 2010).
When tooth extraction is planned, clinicians must decide when to extract, how to manage the extraction sockets to minimize ridge remodeling, and what method of tooth replacement will be used (immediate, delayed, or late). The residual or reconstructed ridge is generally the weak link in an esthetic oral rehabilitation, because the hard and soft tissues can never predictably be regenerated to the previous natural level, despite preservation and augmentation procedures.
Maintaining the buccal part of the root at the time of the tooth extraction may be another way of preventing crestal bone level change and soft tissue recession. However, further long-term studies are needed. At 4 months, new cementum develops at the apical part of the tooth and bone loss of 0.2 mm is observed on the buccal gingival margin (Hürzeler et al., 2010).
After an extraction, preservation of the peri-implant soft tissue architecture and texture, combined with maintenance of the marginal bone levels, are absolute prerequisites for long-lasting esthetic success. Regardless of the implant approach (immediate implant placement with flapless surgery, immediate implant placement and loading, or delayed/late implant placement), several issues are of paramount importance to an ideal treatment outcome: atraumatic extraction techniques, ideal three-dimensional implant placement, supplemental ridge augmentation when necessary, and adjunctive soft tissue regeneration augmentation to enhance the soft tissue biotype and tissue volume. Under the right conditions, nature itself takes care of the major part of the healing process (Leziy and Miller, 2007).
An association exists between bone and soft tissue preservation around implants, and this has a direct influence on esthetics. As a support for the soft tissue, this stable marginal bone is a determinant of the long-term esthetic stability, and vice versa.
The preservation of crestal bone around dental implants cannot be attributed to a single factor. The final esthetic outcome is the result of a number of important parameters, especially in the challenging esthetic zone (Saadoun, 2010; Sonick et al., 2012) (Fig. 6.5):
Figure 6.5 The esthetic risk management parameters.
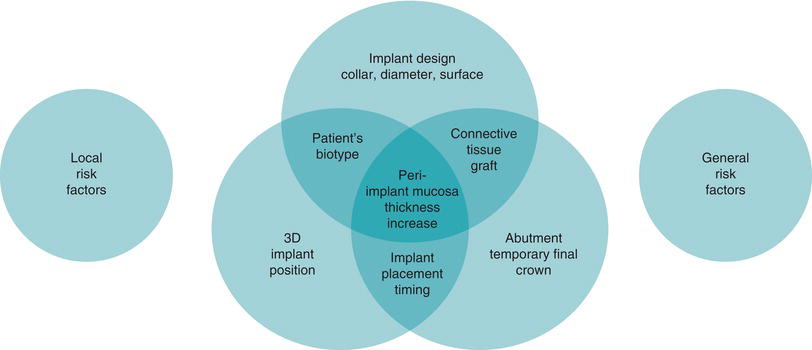
- the implant design, collar, surface, and diameter
- the patient’s biotype – thick or thin
- the biological width
- the timing of the extraction and of placement of the implant
- forced eruption before tooth extraction
- flap design – flapless versus pedicle roll or flap elevation
- the tridimensional position and orientation of the implant
- the timing of placement of the connective tissue graft
- the implant/abutment connection
- temporary or final restoration, and
- occlusal loading with or without functional occlusion.
All these various and multiple parameters are considered as posing risk to the esthetic zone, especially if they do not work together in synergy, to achieve the objective of a final increase the peri-implant mucosa.
Implant biomechanical considerations
There is a major management protocol for the parameters that aim to enhance the patient’s soft tissue thickness biotype around an implant restoration (Fu et al., 2011):
- From an engineering perspective, it is widely accepted that the bone loss around the implant’s crest module is multicausal in nature. These factors are related to the design of the implant collar (the design of the crest module/implant connection).
- From a mechanical standpoint, if same-diameter implants with the three different available crest module designs (divergent, parallel, and convergent) are to be placed in a given region, the convergent-shaped crest module implant will be less likely to lead to a loss of cervical bone, due to the higher level of bone around the crest module, which will help to dissipate the functional loads (Shi et al., 2007).
- Among the contributing factors over which the private practitioner has control is proper treatment planning to ensure the right number and the correct positioning of implants. The bone volume of the implant site should allow ideal positioning of the implant, which is the cornerstone of esthetic success.
- Determination of the right number and correct positioning of implants facilitates proper restoration and occlusal adjustment, thus greatly diminishing the human contribution to crestal bone loss (Marincola et al., 2009).
- The implant should be inserted in an optimal three-dimensional (3D) implant position and orientation, either manually or using a surgical guide, and the following rules should always be respected:
- Mesiodistal position: 1.5–2.0 mm between a tooth and an implant, and 3 mm between adjacent implants; 3.5–4.5 mm between the upper central incisors (Figs 6.7a–c).
- Buccolingual position: 2–3 mm inside from the line joining the adjacent gingival margins (Figs 6.7d–f).
- Apico-coronal position: 3 mm apically from the gingival margin of the implant site (Figs 6.7g–j).
- Factors affecting the esthetic outcome are the implant location, the horizontal buccal size gap, and the thickness of the buccal wall.
- The tridimensional implant position and angulation induces the emergence profile, the architecture of the peri-implant soft tissue, the level of the scalloped gingival margins and the interdental papillae (Saadoun and Le Gall, 1992).
- From a clinical point of view, implants installed into extraction sockets – either manually or using a surgical guide – by means of a model-based (Figs 6.8a–f) or computer-based approach should be utilized to facilitate extreme precision with regard to implant placement. The use of digital instrumentation based on 3D imaging has brought new dimensions to implant therapy:
- The buccal cervical implant collar should not go beyond a line joining the buccal enamel convexity of the adjacent teeth; nor should it go beyond 3 mm from a line joining the two cemento-enamel junctions (CEJs).
- Any buccal positioning of the implant will definitely thin out the remaining buccal cortical plate. This is why it is important to place a smaller implant in a slightly more palatal position, to prevent this phenomenon from occurring.
- In a study by Chen et al. (2007), when implant shoulder was placed buccally in the fresh extraction socket, three times more soft tissue recession occurred. Therefore, the implant should be positioned palatally, and 1 mm apically to the buccal crest.
- It is imperative, in the esthetic area, to place the implant slightly palatally for a 2–3 mm of buccal bone crest to remain present or to be established. The buccal/implant gap is always grafted (S. Leziy, pers. comm., 2010). Therefore, when implants are placed palatally, the buccal gap of > 2 mm should be filled with bone, exposing less implant on the buccal aspect.
- In sites with thick bony walls (> 1 mm), more bone fill occurs if the gap is < 2 mm.
- Age and smoking negatively affect bone fill (Paolantonio et al., 2001; Tomasi et al., 2010).
- The implant should be positioned approximately 1 mm deeper than the level of the buccal alveolar crest, and in a lingual/palatal position in relation to the center of the alveolus, in order to reduce or eliminate exposure above the alveolar crest of the endosseous (rough) portion of the implant (Caneva et al., 2010).
- More apically positioned implants suffer less implant exposure buccally.
- The microgap in the implant/abutment connection exists naturally in the two-part implant system. In most cases, it is susceptible to microbial seeding and micromovements between the parts during clinical occlusal function.
- Both the microgap and micromovements may lead to localized bacterial inflammation and associated crestal bone loss if the microgap is within a minimum distance, less than 5 mm, from the alveolar crest (Deporter et al., 2008). Therefore, the connection between the implant and the abutment should ideally be biomechanically resistant. Furthermore, the implant/abutment connection is the point of concentration for all the functional stresses. This will induce micro-disconnection, which causes the seal to deteriorate.
- It is necessary to ensure a good seal in this connection to prevent micromovements, because any leak at the interface between the implant and the abutment will be prejudicial to the health of the biological width (Maeda et al., 2007).
- This seal will depend on some specific mechanical considerations:
- Indexation is achieved by a passive hexagon resting in continuity with an active cone, preventing implant deformation.
- Platform switching is obtained by having an abutment diameter that is smaller than the implant diameter.
- Resistance is achieved by the friction of the abutment as it enters the implant (a Morse cone with an angle of 2–3° or a cone with 5.2° of conicity). The purpose of this type of internal connection is to spread out the loading of the transversal forces.
- Anti-rotation is realized by friction between two cones with 15° and 3° conicity.
- The friction decreases the space between the internal connection and the prosthetic abutment. Consequently, the dispersion of the occlusal forces on the implant’s internal surfaces decreases the microgap.
Figure 6.6 (a) A diagrammatic representation of the three different types of implant design. (b) The divergent, parallel, and convergent cervical collars of three different implant designs. (c) The back-tapered coronal design provides additional cervical bone volume for optimal soft tissue support after implant placement. (Courtesy of Nobel Biocare.)
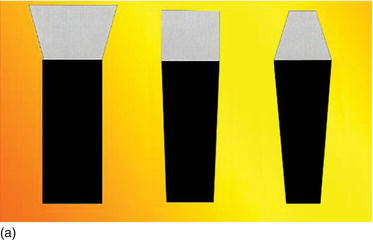

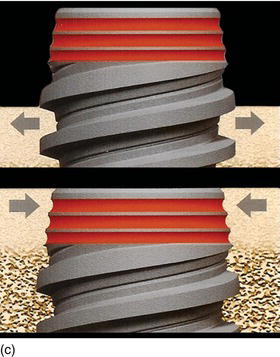
Figure 6.7 (a) A mesiodistal position of 2 mm between the tooth and the implant. (b) The mesiodistal position on the cast model (occlusal view). (c) The mesiodistal position on the patient (occlusal view). (d) A bucco-palatal position of 2–3 mm from the gingival line of the adjacent teeth. (e) The bucco-palatal position on the cast model (left view). (f) The bucco-palatal position on the patient (left view).
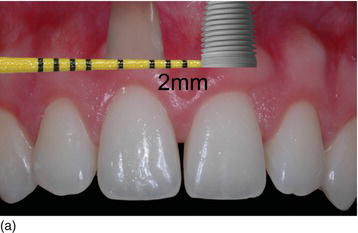
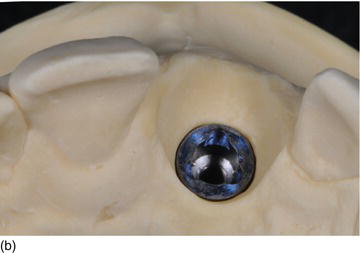

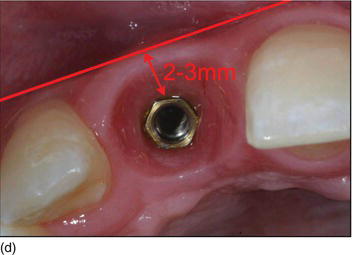

Figure 6.7 (g) An apico-coronal position of 3 mm from the gingival margin to the implant platform. (h) The apico-coronal position on the cast model (palatal view). (i) The apico-coronal position on the patient (right view). (j) An interproximal distance of 4.0–4.5 mm between two adjacent implants for the two maxillary central incisors. (Figures (b), (e), and (h) courtesy of Mr. G.M. Etienne, Pulnoy, France.)

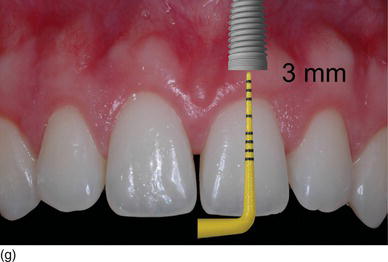


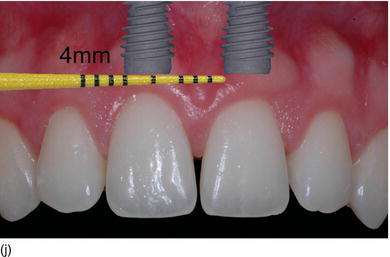
Figure 6.8 (a) A model-based surgical guide placed on the maxillary teeth. (b) Immediate implant insertion after extraction of a tapered drive implant, with a convergent collar and an aggressive thread in order to achieve good primary stability. (c) A 3D implant position, with the implant in a slightly palatal angulation. (d) A zirconium abutment placed immediately, with a retracting cord to take the impression. (e) An X-ray of the Morse cone abutment, with the switch platform between the implant and the abutment. (f) The final restoration, with excellent PES/WES. (Courtesy of Dr. M. Groisman, Rio de Janeiro, Brazil.)





Only a Morse cone connection can create a seal compatible with a healthy biological width and prevent crestal bone loss (Puchades-Roman et al., 2000).
The maintenance of the marginal bone is crucial both from a functional as well as an esthetic point of view. Preserving the marginal bone levels and establishing the biological width at the abutment level are really all about ensuring the right stimulation of the bone and promoting healthy soft tissue (see Fig. 6.7f). Therefore, healthy soft tissue and well-maintained marginal bone are interdependent. The one cannot exist without the other, because while it is vital that the soft tissue protects the bone, the bone must also be maintained to help support the soft tissue – a necessary symbiosis.
Figure 6.9 (a) A Morse cone abutment in the Neodent Drive® implant guarantees the seal connection and the thickness of the peri-implant tissue. (b) The Biomet Prevail® implant, which allows the switch platform to enhance the soft tissue thickness. (c) The NobelReplace™ conical connection hex platform, which provides a strong seal connection with a maximum peri-implant tissue volume. (d) The strong and tight fit of the NobelReplace™ internal conical connection abutment. (e) The NobelReplace™ three-lobe platform shift, which improves the esthetic appearance of the soft tissue. (f) Nobel Abutment® built-in platform shifting with an internal tri-channel connection. (Figures c–f courtesy of Nobel Biocare.)

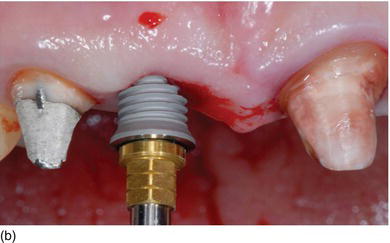
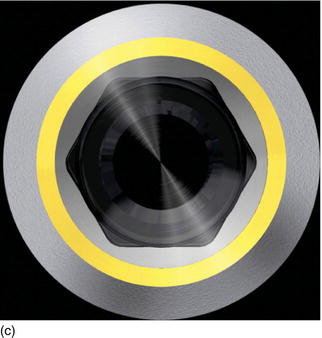

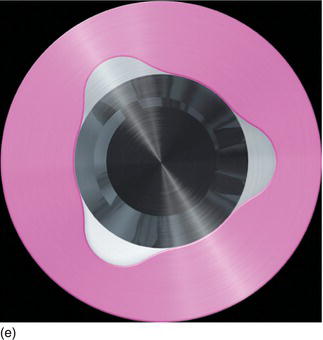

Figure 6.9 (g) The Nobel Curvy® abutment on a Nobel-Replace™ implant increases the subgingival tissue volume.

Peri-implant mucosa thickness
The acquisition of a significant buccal bone volume alone has, with time, proved to be insufficient to maintain ideal gingival architecture. In fact, it is recommended to systematically boost the initial gingival biotype by adding a connective tissue graft, no matter what the thickness and quality of the soft tissue at the outset (Figs 6.10a–i).
Reinforcement of the peri-implant gingiva to thicken and stabilize it is mostly done by adding connective tissue in the form of a free connective graft with a coronally advanced flap, or combined with the pedicle flap, according to the initial clinical situation and the surgical protocol, in order to prevent any risk of gingival recession (Degorce, 2009).
The absence of keratinized gingiva – or the presence of a limited amount, with regard to both thickness and height – increases bacterial plaque accumulation and induces secondary bone resorption and marginal gingival recession. Therefore, a soft tissue graft to increase the quality and quantity of keratinized gingiva permits the control of plaque accumulation and limits tissue inflammation, which will directly minimize crestal bone resorption and peri-implant soft tissue recession (Rompen, 2011).
Because of the fact that cementum in natural teeth is more preferable than implant titanium, and that there is no more vascularization from the periodontal ligaments, a contraction of 66% of the graft has been observed at 6 months (Bukhardt et al., 2008).
Lastly, it is necessary to create an optimal concave submergence profile />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


